Prehospital code stroke (CS) systems have been proved effective for improving access to specialised medical care in acute stroke cases. They also improve the prognosis of this disease, which is one of the leading causes of death and disability in our setting. The aim of this study is to analyse results one year after implementation of the new code stroke protocol at one hospital in Asturias.
Patients and methodsWe prospectively included patients who were admitted to our tertiary care centre as per the code stroke protocol for the period of one year.
ResultsWe analysed 363 patients. Mean age was 69 years and 54% of the cases were men. During the same period in the previous year, there were 236 non-hospital CS activations. One hundred forty-seven recanalisation treatments were performed (66 fibrinolysis and 81 mechanical thrombectomies or combined treatments), representing a 25% increase with regard to the previous year.
ConclusionsRecent advances in the management of acute stroke call for coordinated code stroke protocols that are adapted to the needs of each specific region. This may result in an increased number of patients receiving early care, as well as revascularisation treatments.
Los sistemas de código ictus prehospitalario han demostrado ser eficaces en la mejoría del acceso a una atención médica especializada en el ictus agudo y en condicionar un mejor pronóstico en la enfermedad, que es una de las principales causas de muerte y discapacidad en nuestro medio. El objetivo de este estudio es analizar los resultados del primer año de puesta en marcha del nuevo protocolo de código ictus (CI) en Asturias en un solo centro.
Pacientes y métodosSe incluye de forma prospectiva a los pacientes que acuden dentro del protocolo de código ictus a un centro de tercer nivel asistencial durante el periodo de un año.
ResultadosSe analiza a 363 pacientes. La edad media fue de 69 años y en el 54% de los casos se trataba de varones. Para el mismo periodo del año previo las activaciones extrahospitalarias de CI fueron 236. Se llevaron a cabo 147 tratamientos recanalizadores (66 fibrinólisis y 81 trombectomías mecánicas o tratamientos combinados), lo que supuso un incremento del 25% con respecto al año previo.
ConclusionesLos recientes avances en la terapéutica del ictus agudo hacen necesaria la instauración de protocolos coordinados de CI que se adapten a las necesidades de cada región concreta, lo que puede resultar en un incremento del número de pacientes atendidos precozmente, así como de los tratamientos revascularizadores realizados.
Cerebrovascular diseases are the most common cause of disability in adults and one of the main causes of death in Spain.1 In the specific case of Asturias, stroke has become the leading cause of death in women in the region and the third most frequent in men.2 Several treatment measures developed in recent decades have improved the prognosis of stroke patients. Such measures include the introduction of tissue plasminogen activator (IV tPA),3 approved in Europe in 2002, and the more recent validation of endovascular treatment for stroke secondary to large-vessel occlusion (LVO).4–10
Another important treatment measure was the 2006 Helsingborg Declaration,11 which proposed stroke units (SU) as the most effective hospital resource for managing acute stroke and established a clear objective for 2015: to ensure that all stroke patients receive assessment in a stroke unit.
In light of the above, the creation of a coordinated code stroke (CS) protocol tailored to the specific needs of each region is a vital step towards ensuring that all patients will have quick, efficient access to a centre of reference in cerebrovascular disease. Coordinated, well-organised CS protocols require cooperation between neurology departments and prehospital emergency services.12
These protocols must also include diagnostic tools that assist in triaging patients by stroke severity so as to refer each one to the most suitable hospital. The National Institute of Health Stroke Scale (NIHSS) is the most widely used and validated scale both for diagnosis and for predicting stroke outcomes. A cut-off point of 10 has been found to predict presence of an LVO with high sensitivity and specificity.13 Other scales, such as the Los Angeles Prehospital Stroke Screen (LAPSS), have been widely used in prehospital stroke triage and are of comparable effectiveness to the NIHSS for diagnosing LVO, given a cut-off point of 4.14 Despite there being a wide range of stroke scales other than the LAPSS, most of which are based on a selection of items from the original NIHSS (examples include the Rapid Arterial Occlusion Evaluation [RACE15] scale and the sNIHSS-416), the NIHSS is the prehospital triage tool which has most commonly been used by physicians and paramedics over the years.
The region of Asturias covers a territory of 10 603.57 km2 and has 1 051 229 inhabitants according to the most recent data from Spain's National Statistics Institute.17 This region is characterised by rugged terrain and a population that is scattered widely across its outlying areas, which even today leads to communication problems.
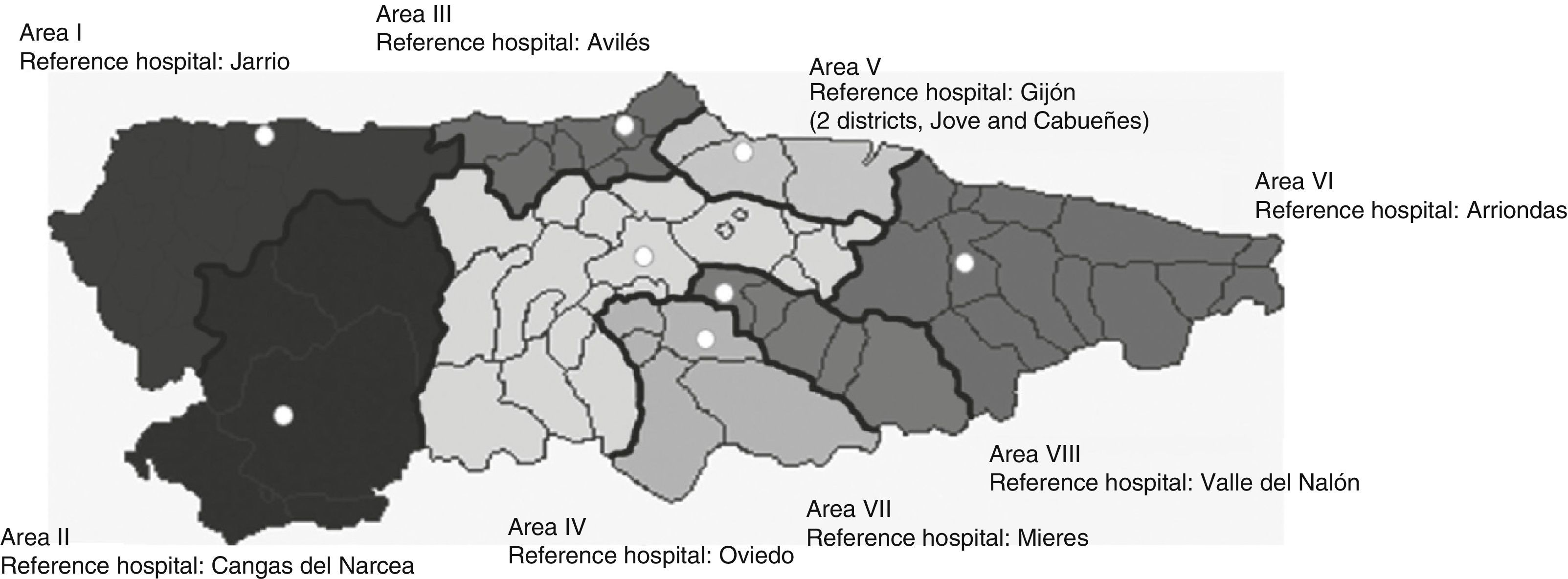
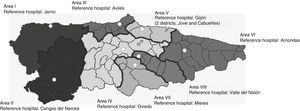
The province of Asturias is divided into 8 health districts (Fig. 1), each of which has a reference hospital. Only the reference hospitals in health districts IV (Hospital Universitario Central de Asturias [HUCA], Oviedo) and V (Hospital de Cabueñes, Gijón) have an on-call neurologist available 24hours a day, 7 days a week; a stroke unit; and the ability to perform acute stroke treatment (both IV tPA and endovascular therapy at the HUCA and only IV tPA at Hospital de Cabueñes).
Healthcare areas in Asturias.
Source: Modified from Benavente et al.21
The protocol for stroke management used in Asturias before the implementation of CS is now obsolete; previous studies already proposed endovascular therapy as an effective alternative to intravenous fibrinolysis.18–20 Before the CS was introduced, patients in health district V were referred to Hospital de Cabueñes, a hospital equipped to provide only IV tPA and unable to perform endovascular therapy, should it be necessary. For this reason, a new protocol was designed in 2013.21 Since there is a high correlation between the stroke scale scores (NIHSS and other prehospital stroke scales) recorded by various prehospital emergency services and by neurology departments22,23, the emergency medical services (SAMU) apply the NIHSS and LAPPS scales in order to determine the most suitable reference centre for each patient.
The purpose of this study was to prospectively gather and analyse data on patients transported to HUCA as a result of CS activation.
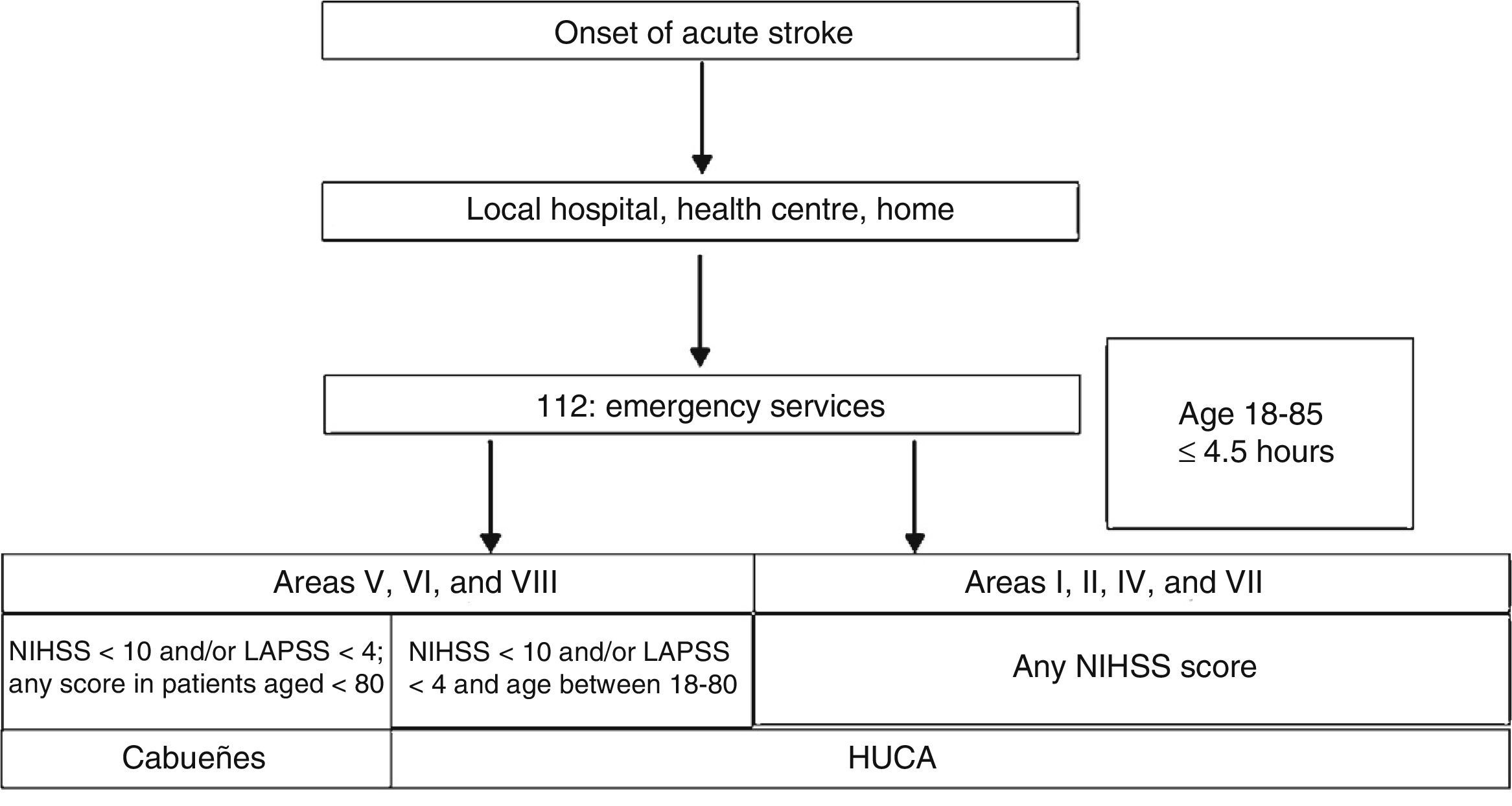
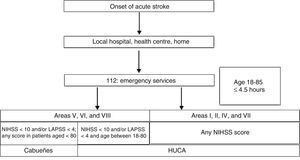
Patients and methodsThe CS protocol as designed and implemented in May 2013 is shown in Fig. 2. SAMU personnel attended a 30-minute training session on the use of the NIHSS and LAPSS scales; training was delivered by a neurologist specialising in cerebrovascular diseases. Unlike in other regions, SAMU staff in Asturias are physicians; the reliability and effectiveness of these services in administering the NIHSS has been validated in a previous study.22,23
The emergency coordination team decides where to refer patients based on the data gathered by prehospital emergency personnel (NIHSS and LAMS scores) and recorded on a specifically designed form.
Data were prospectively collected from 1 June 2013 to 31 March 2014. The emergency coordination team automatically registers all calls with a CS activation using a simple electronic form that includes such data as original location, age, sex, and referral hospital. The on-call neurologist obtains demographic, clinical, and imaging data as well as NIHSS and LAPSS scores for all patients arriving at the emergency department following CS activation.
We present demographic, clinical, and radiological data and other information gathered by SAMU from all patients transferred to HUCA as part of the prehospital CS protocol, and from those patients receiving care at HUCA following in-hospital CS activation, during the first year following the implementation of the updated CS. These data were compared to the number of CS activations in the same period of the previous year and the treatments administered. We were unable to conduct a more thorough comparison due to the lack of a previous register of CS activations at the hospital in question.
ResultsAll patients with symptoms of acute neurological deficit who called the emergency telephone number were included in the CS protocol. According to the register kept by SAMU services, CS was activated in Asturias on 438 occasions between 1 June 2013 and 31 May 2014. No data is available on those patients with acute stroke for whom emergency services were not called but who were taken to smaller hospitals located in outlying areas, as these hospitals do not keep stroke registers.
Of all patients for whom CS was activated, 91 (21%) were transferred to Hospital de Cabueñes and 347 (79%) to HUCA.
For the same period in the previous year, CS was activated by prehospital personnel on 236 occasions.
In addition to the patients derived under the new prehospital CS protocol, there were 9 in-hospital CS activations and 20 CS activations in the HUCA's emergency department. This gives us a total of 385 CS activations at HUCA during a 12-month period. We were able to collect data on all variables for 363 patients.
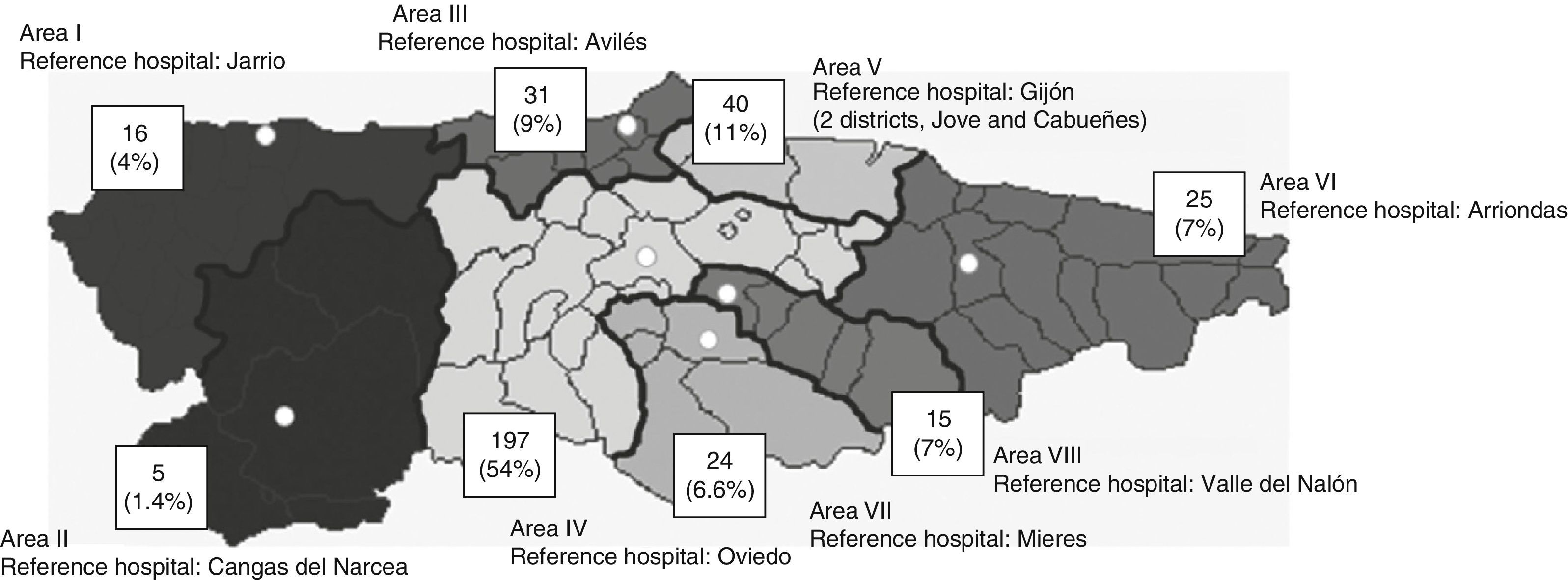
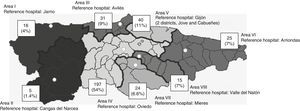
Demographic dataThe mean age in our sample was 69 years (range, 25-85); 165 patients were women (46%) and 198 were men (54%). Most of the patients were transferred from a prehospital setting (98%), either from their homes (80%) or from a local health centre (18%). In the remaining cases, CS was activated in-hospital. Most patients were transported to the reference hospital in an advanced life support ambulance (67%); the remaining patients were transferred in conventional ambulances (25%), private vehicles (6%), and by helicopter (2%). Fig. 3 shows patients’ place of residence by health district.
CS patients’ place of residence by healthcare area.
Source: Modified from Benavente et al.21
Mean time from symptom onset to arrival at the hospital was 1hour 43minutes (1hour 50minutes for the same period in the previous year).
Clinical dataMost of the patients had ischaemic stroke (66%) or haemorrhagic stroke (15%), with smaller percentages of stroke mimics (12%) and transient ischaemic attack (7%).
According to the Oxfordshire Stroke Project Classification24 for ischaemic stroke, the most frequent types recorded in our study were total anterior circulation infarct (33%) and partial anterior circulation infarct (29%), followed by posterior circulation infarct (27%) and lacunar circulation infarct (LACI) (11%).
The median NIHSS score was 14 points (4-25).
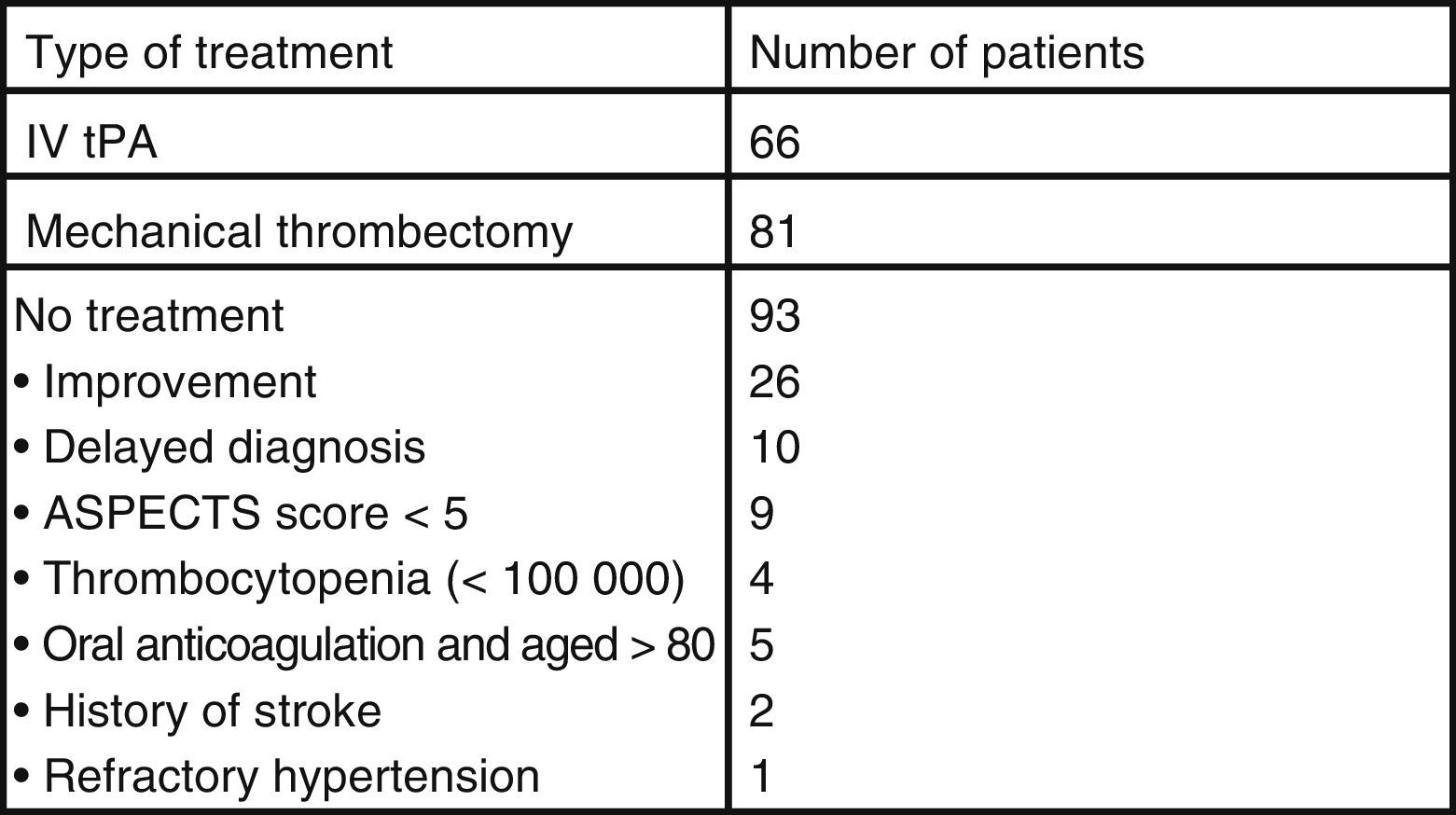
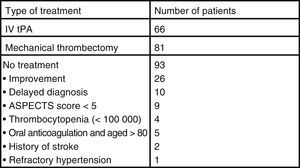
Fig. 4 lists the treatment used and the reasons for not administering treatment for ischaemic stroke. Of the 240 patients with ischaemic stroke, 66 (27.5%) received IV tPA only and 81 (34%) underwent mechanical thrombectomy (MT), either alone or combined with IV tPA.
In the same period of the previous year, 70 patients were treated with IV tPA and 45 with MT. This represents a 25% rise in the number of patients treated with the implementation of the new protocol.
Following acute management, 222 patients (61%) were admitted to the SU at HUCA, 79 (22%) to the general neurology department, and 45 (12%) to the intensive care unit (part of the department of intensive medicine); the remaining patients were not admitted to HUCA's neurology department, either because they had stroke mimics or because they were referred back to their reference hospital.
All patients underwent a CT scan at baseline; 231 patients (64%) also underwent CT angiography.
DiscussionPrevious studies have demonstrated that the implementation of CS prehospital protocols is effective both in taking advantage of the available treatments and in improving stroke patients’ access to specialised care and SUs and their long-term functional outcomes.25–30
Given the recent advances in therapeutic options for acute stroke, with the validation of endovascular treatments for LVO, prehospital transportation systems and triage protocols should be modified in order to offer patients efficient, equal, and timely access to reference hospitals equipped to provide acute stroke treatment.
This study shows that the CS protocol implemented in Asturias in May 2013 led to an increase in the provision of early specialised care, with a larger number of CS activations and increased use of the available thrombolytic and endovascular therapies.
The number of CS activations in Asturias is high, and is comparable with such other Spanish regions as Catalonia, which has a larger target population and a prehospital CS protocol which has been active for more years.12,30–32 However, the results of this study do not correspond to the total number of patients with acute stroke in the region, since those patients transferred to and treated at Hospital de Cabueñes and those older than 85 were excluded.
The analysis of results also shows a continuing imbalance in access to acute stroke care in the different areas of the region. Outlying regions, which according to the latest census data account for 133231 inhabitants and have the most elderly population, represent only 12.4% of CS activations. This suggests that there is a need to implement specific training measures aimed both at the healthcare professionals of those areas and at the local population. It also underscores the need for a telemedicine system to overcome the existing geographical barriers.
This study therefore shows that establishing prehospital CS systems offers clear, although not sufficient, benefits in the emergency care provided to patients with cerebrovascular diseases. These systems also lead to a higher number of CS activations and recanalisation treatments, as well as a slight decrease in prehospital times.
FundingThis study has received no funding of any kind.
Conflict of interestThe authors have no conflicts of interest to declare.
The authors would like to thank the professionals working in the emergency medical services of Asturias, and the emergency department and radiology department at Hospital Universitario Central de Asturias.
Please cite this article as: García-Cabo C, Benavente L, Martínez-Ramos J, Pérez-Álvarez Á, Trigo A, Calleja S. Análisis del primer año del nuevo protocolo de código ictus en Asturias. Experiencia de un único centro. Neurología. 2018;33:92–97.