Informal caregivers provide care to dementia patients, and this service prolongs their stay at home.
ObjectivesTo describe characteristics of dementia patients in the province of Alicante, as well as the profiles and roles of caregivers who assist them.
Patients and methodsMulti-centre prospective study carried out in 4 neurology departments in Alicante (June 2009–January 2010). Dementia patients’ relatives/caregivers were included in sequential order. The following variables were analysed: (a) Demographic information pertaining to the patient and caregivers (age, sex, marital and employment status, educational level, relationship to patient); (b) patient's family unit; (c) motivating factor for primary caregiver (PC); (d) secondary caregiver (SC) roles; (e) country of citizenship of formal caregiver (FC) and source of remuneration (private/public); (f) caregivers’ knowledge of dementia.
ResultsMost of our patients live at home (74.8%), and are female (69%) with Alzheimer's disease (78.4%) in a moderately severe stage (GDS level 4–5, 71.6%). PCs and SCs are mainly women (72.1% and 60.5%, respectively), middle-aged and directly related to the patient (sons/daughters account for 64.3% of the PCs and 54.4% of the SCs); most are homemakers with a low educational level. Caregivers in the first category (PC) provide care due to moral obligation (75%), while those in the second (SC) involve patients in leisure or other stimulating activities (82.3%). Absent caregivers tend to be males (73.3%) residing long distances from the relative (52.4%). The FC tends to be female (91.7%), Spanish (81.8%) and privately remunerated.
ConclusionsWomen dominate the network of caregivers for dementia patients, whether as principal caregivers, supporting caregivers or formal caregivers (in all cases, they have only limited training in dementia management). Males are largely absent. Better knowledge of the care structure supporting dementia patients may be helpful in the overall management of these patients.
Los cuidadores informales garantizan el cuidado de los pacientes con demencia, prolongando la estancia en su domicilio.
ObjetivosDescribir las características de los pacientes con demencia de la provincia de Alicante, así como los perfiles y roles de los cuidadores implicados en su manejo.
Pacientes y métodosEstudio prospectivo multicéntrico realizado en 4 consultas de neurología de la provincia de Alicante (junio del 2009–enero del 2010). Inclusión consecutiva de familiares/cuidadores de pacientes con demencia. Analizamos: (a) datos demográficos del paciente y cuidadores (edad/sexo, estado civil/laboral, estudios, parentesco); (b) unidad de convivencia del paciente; (c) motivación para el cuidado del cuidador principal (CP); (d) roles del cuidador secundario (CS); (e) nacionalidad del cuidador formal (CF) y origen remuneración (privada/institucional), y (f) formación en demencias de los cuidadores.
ResultadosNuestros pacientes residen en su domicilio (74,8%). Principalmente, son mujeres (69%) con enfermedad de Alzheimer (78,4%) moderadamente grave (GDS 4–5, 71,6%). CP y CS son mujeres (72,1% vs 60,5%), de edad media, parentesco directo (hijo/a 64,3% vs 54,4%), nivel cultural bajo y amas de casa. Las primeras garantizan el cuidado por obligación moral (75%), las segundas se ocupan del ocio/estimulación del paciente (82,3%). Los grandes ausentes son los varones (73,3%), quienes residen lejos del familiar (52,4%). El CF es una mujer (91,7%), española (81,8%) con remuneración privada.
ConclusionesLa mujer es el elemento principal en la red de cuidadores de pacientes con demencia: como CP, de apoyo o CF (todos con escasa formación en demencias), siendo el varón el gran ausente. Conocer la estructura de cuidados de estos pacientes facilitará su manejo.
The last few decades have seen a marked ageing trend among the world's population accompanied by an increase in age-related diseases. Forms of dementia offer the most cause for concern since the enormous costs they generate mean that they pose massive problems for societies and healthcare systems. Most patients with dementia are very elderly and suffer from highly debilitating chronic disease. As a result, they become increasingly dependent on assistance provided by others in order to perform even the most basic activities of daily living. The family typically takes over these tasks; patients’ families are the main providers of long-term care. Normally, networks or support groups of informal caregivers may include family members, friends, neighbours, and people close to the patient who perform non-remunerated care tasks. Their contributions are essential because this type of care enables patients to remain with their families for longer time periods, thereby decreasing economic and social costs.1–5
However, the significant changes taking place in our society will have an impact on the informal care system for dementia patients. This is especially true with regard to roles filled by women, who have typically acted as primary caregivers, since their presence in the labour market continues to grow.6,7 These social changes, and their transcendental effects on care for dementia patients, mean that we must be aware of new care models.
Our article aims to describe the caregiver network providing service to dementia patients in the province of Alicante. We will analyse characteristics of the patients receiving care in the network, as well as the profiles and roles corresponding to the different types of caregivers involved in patient care and management.
Patients and methodsWe carried out a prospective study in 4 general neurology departments in the province of Alicante between June 2009 and January 2010. The study included families/caregivers of dementia patients monitored by these consults in consecutive order. Patients diagnosed a minimum of 1 year prior to recruitment, with any type of dementia at any stage, were included. We excluded patients diagnosed less than 1 year prior to recruitment; those whose PC or SC could not be contacted (they attended appointments alone or with a formal caregiver [FC]); patients residing in assisted-living centres; and patients whose relative/caregiver refused to sign the informed consent form.
Our working definitions are as follows:
- -
Primary caregiver (PC): person who assumes responsibility for providing companionship, support, and daily care to the dementia patient; person most frequently in the company of the patient (normally a direct relative or spouse).
- -
Secondary or supporting caregiver (SC): person who assists or substitutes the PC as needed in order to provide care for the dementia patient. May be a relative, friend, or neighbour.
- -
Formal caregiver (FC): person hired to care for a dementia patient in exchange for remuneration. The FC typically is not a family member or close acquaintance of the patient.
- -
Absent caregiver (AC): a relative, spouse, or other close acquaintance who is expected to be involved in and contribute to the patient's care based on his/her relationship with the patient, but who does not engage in care activities for some reason.
The study examines the following variables:
- -
Concerning the patient: demographic data (age, sex, educational level, marital status); clinical variables (degree of cognitive decline according to the modified GDS/Reisberg scale8 and dementia type; and household arrangement (HA, people sharing a household with the patient, place of residence, day care attendance, presence of an FC).
- -
Concerning the PC: demographic data; relationship with patient; household arrangement (with patient or distance from patient's residence); employment status (considering the possibility that the PC has petitioned for reduced working hours or left a job to care for the patient); motives for caring for the patient (moral duty, to ensure the patient's dignity and gain personal satisfaction, gratitude toward/repayment of the patient, social pressure, lack of funds for a residential centre); and presence of physical/emotional problems.
- -
Concerning the SC: demographic data; roles in care (general patient coordination, economic or medical management, transport, treatment monitoring, help with domestic tasks, help performing activities of daily living, and participation in the patient's leisure time and cognitive stimulation).
- -
Concerning the FC: demographic data; nationality; source of remuneration (public funds or private funds from the family).
- -
Concerning the AC: demographic data; distance to the patient's residence.
- -
Level of training in dementia displayed by each type of caregiver.
Information was entered in a relational database (Access 2000, Microsoft Office) designed specifically for this study. The database recorded all the patients visiting the department, plus any accompanying family members and/or caregivers, according to the inclusion and exclusion criteria. For the descriptive data analysis, we used estimated percentages or means with their respective margins of error expressed as standard deviations for a 95% confidence interval. Arithmetic mean and standard deviation were used for the descriptive analysis of patients’ ages. We used the chi-square test to compare qualitative variables and the t-test to compare quantitative variables.
Data was only obtained from the patients and caregivers included in the study after the informed consent statement was signed by either the patient (for mild to moderate cases of dementia) or the relative/caregiver (for moderately severe to severe cases of dementia).
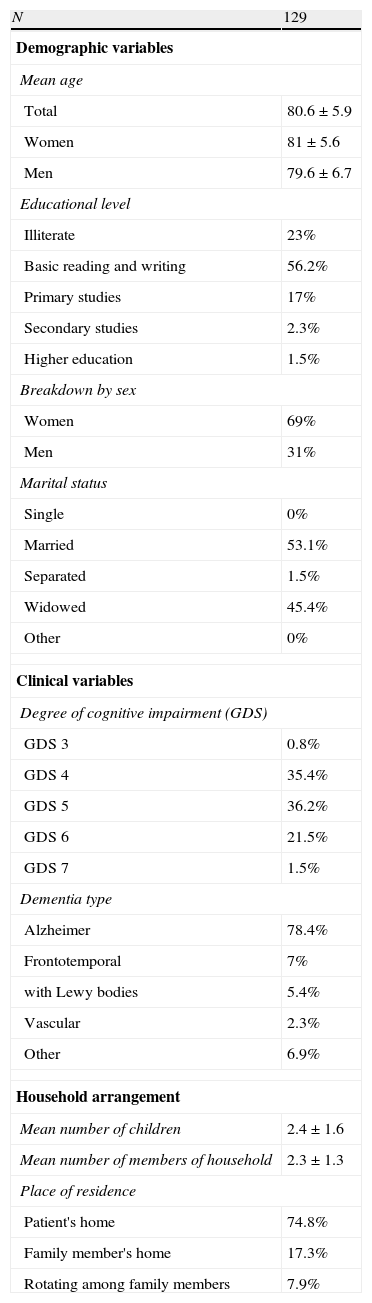
ResultsDuring the study period, 129 patients were included (89 women [69%] and 40 men [31%]) with a mean age±SD of 80.6±5.9 years. Most patients were described as having a low to very low educational level (56.2% had basic reading and writing skills; 23% were illiterate) and either married (53.1%) or widowed (45.4%). We recorded a moderate to moderately severe degree of cognitive decline in 71.6% of patients (GDS of 4 in 35.4% and GDS of 5 in 36.2%). The most common type of dementia was Alzheimer disease (78.4%). The average number of children per patient was 2.4 (SD=1.6) and the average number of people in the household was 2.3 (SD=1.3). We noted that 74.8% of patients continued to live in their own homes, while 7.9% circulated between relatives’ different households. Of the patients, 91.4% lived with another person, a spouse in over half the cases (53.1%); most spouses were female (54.8%). Only 11.6% of the patients had an FC and 20% of the total attended day care (Table 1).
Characteristics of dementia patients.
| N | 129 |
| Demographic variables | |
| Mean age | |
| Total | 80.6±5.9 |
| Women | 81±5.6 |
| Men | 79.6±6.7 |
| Educational level | |
| Illiterate | 23% |
| Basic reading and writing | 56.2% |
| Primary studies | 17% |
| Secondary studies | 2.3% |
| Higher education | 1.5% |
| Breakdown by sex | |
| Women | 69% |
| Men | 31% |
| Marital status | |
| Single | 0% |
| Married | 53.1% |
| Separated | 1.5% |
| Widowed | 45.4% |
| Other | 0% |
| Clinical variables | |
| Degree of cognitive impairment (GDS) | |
| GDS 3 | 0.8% |
| GDS 4 | 35.4% |
| GDS 5 | 36.2% |
| GDS 6 | 21.5% |
| GDS 7 | 1.5% |
| Dementia type | |
| Alzheimer | 78.4% |
| Frontotemporal | 7% |
| with Lewy bodies | 5.4% |
| Vascular | 2.3% |
| Other | 6.9% |
| Household arrangement | |
| Mean number of children | 2.4±1.6 |
| Mean number of members of household | 2.3±1.3 |
| Place of residence | |
| Patient's home | 74.8% |
| Family member's home | 17.3% |
| Rotating among family members | 7.9% |
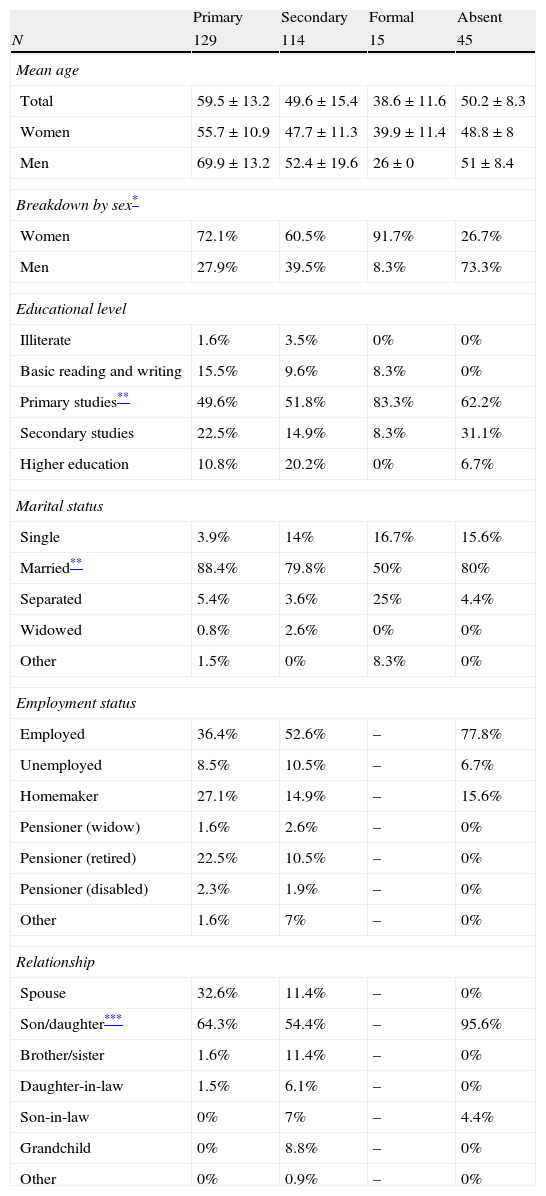
We included 129 PCs (93 women [72.1%] and 36 men [27.9%]) with a mean age±SD of 59.5±13.2 years. Most were married (88.4%) with an intermediate to low educational level (22.5% had some secondary education and 49.6%, primary only). Caregivers were the patient's children in 64.3% of the cases; 32.6% were spouses. Regarding employment status, 36.4% were actively employed, although 13.1% had petitioned for reduced working hours in order to care for the patient and 5.4% had left their jobs for the same reason. Homemakers and retirees accounted for 27.1% and 22.5% of the caregivers, respectively. Most caregivers either lived with their patients (64.8%) or near them (30.8%). Table 2 displays the demographic information corresponding to the different types of caregivers.
Demographic characteristics of different types of caregivers.
| Primary | Secondary | Formal | Absent | |
| N | 129 | 114 | 15 | 45 |
| Mean age | ||||
| Total | 59.5±13.2 | 49.6±15.4 | 38.6±11.6 | 50.2±8.3 |
| Women | 55.7±10.9 | 47.7±11.3 | 39.9±11.4 | 48.8±8 |
| Men | 69.9±13.2 | 52.4±19.6 | 26±0 | 51±8.4 |
| Breakdown by sex* | ||||
| Women | 72.1% | 60.5% | 91.7% | 26.7% |
| Men | 27.9% | 39.5% | 8.3% | 73.3% |
| Educational level | ||||
| Illiterate | 1.6% | 3.5% | 0% | 0% |
| Basic reading and writing | 15.5% | 9.6% | 8.3% | 0% |
| Primary studies** | 49.6% | 51.8% | 83.3% | 62.2% |
| Secondary studies | 22.5% | 14.9% | 8.3% | 31.1% |
| Higher education | 10.8% | 20.2% | 0% | 6.7% |
| Marital status | ||||
| Single | 3.9% | 14% | 16.7% | 15.6% |
| Married** | 88.4% | 79.8% | 50% | 80% |
| Separated | 5.4% | 3.6% | 25% | 4.4% |
| Widowed | 0.8% | 2.6% | 0% | 0% |
| Other | 1.5% | 0% | 8.3% | 0% |
| Employment status | ||||
| Employed | 36.4% | 52.6% | – | 77.8% |
| Unemployed | 8.5% | 10.5% | – | 6.7% |
| Homemaker | 27.1% | 14.9% | – | 15.6% |
| Pensioner (widow) | 1.6% | 2.6% | – | 0% |
| Pensioner (retired) | 22.5% | 10.5% | – | 0% |
| Pensioner (disabled) | 2.3% | 1.9% | – | 0% |
| Other | 1.6% | 7% | – | 0% |
| Relationship | ||||
| Spouse | 32.6% | 11.4% | – | 0% |
| Son/daughter*** | 64.3% | 54.4% | – | 95.6% |
| Brother/sister | 1.6% | 11.4% | – | 0% |
| Daughter-in-law | 1.5% | 6.1% | – | 0% |
| Son-in-law | 0% | 7% | – | 4.4% |
| Grandchild | 0% | 8.8% | – | 0% |
| Other | 0% | 0.9% | – | 0% |
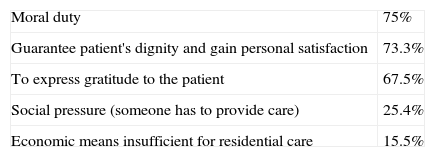
Physical impairments of all types were reported by 29.2% of PCs; 36.9% reported emotional problems (depression and/or anxiety). Half of the PCs considered that they were essential to the patient's care, while 71% confirmed that they received assistance from other family members (63.7% had the support of at least one SC). Regarding reasons why PCs assumed the responsibility of caring for the patient, 75% indicated moral duty; 73.3%, to guarantee the patient's dignity and gain personal satisfaction; 67.5%, out of gratitude to the patient; 25.4%, because someone had to provide care; and 15.5%, due to lack of funds for a residential centre (Table 3).
Main reasons for caring for dementia patients as cited by primary caregivers.
| Moral duty | 75% |
| Guarantee patient's dignity and gain personal satisfaction | 73.3% |
| To express gratitude to the patient | 67.5% |
| Social pressure (someone has to provide care) | 25.4% |
| Economic means insufficient for residential care | 15.5% |
We gathered information from 114 SCs (69 women [60.5%] and 45 men [39.5%]), with a mean age discretely lower than that of the PC group: 49.6±15.4 years. Their educational level was somewhat higher (20.2% had attended university), and most were married as well (79.8%). Most SCs were sons or daughters (54.4%), but the group included other relatives in addition to spouses (siblings, grandchildren, daughters-in-law). Most remained actively employed (52.6%) (Table 2).
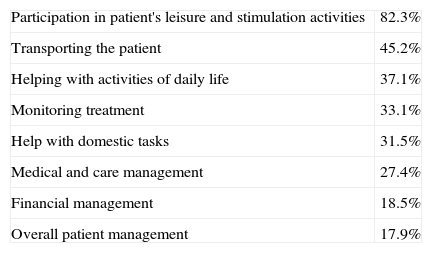
SCs were mainly involved in the patient's leisure activities and cognitive stimulation (82.3%) or in helping the patient perform activities of daily living (37.1%). However, it was much less common for them to assume responsibility for other more complex tasks, such as the management of medical care (27.4%) or overall patient coordination (17.9%) (Table 4).
Roles filled by secondary caregivers.
| Participation in patient's leisure and stimulation activities | 82.3% |
| Transporting the patient | 45.2% |
| Helping with activities of daily life | 37.1% |
| Monitoring treatment | 33.1% |
| Help with domestic tasks | 31.5% |
| Medical and care management | 27.4% |
| Financial management | 18.5% |
| Overall patient management | 17.9% |
The 45 ACs we recorded included 33 men (73.3%) and 12 women (26.7%). They were somewhat younger than the PC group (mean age 50.2±8.3 years) with a discretely higher educational level (62.2% had completed primary school; 31.1% had some secondary studies). ACs were predominantly married (80%) and actively employed (77.8%); almost all were the patients’ children (95.6%) (Table 2). In just over half of the cases, they resided far from the patient (52.4%).
As stated in previous paragraphs, 11.6% of our patients also had at least 1 FC. This group was composed mainly by women (91.7%) with a mean age of 38.6±11.6 years. Half were married and 25% were separated; their educational level was low (83.3% had completed primary school). Most were Spanish citizens (81.8%) and 89% of their remuneration came from a private source, the patient's family (Table 2).
Lastly, we should cite lack of dementia education; only 26.2% of principal caregivers, 27.3% of secondary caregivers, and 13.6% of formal caregivers had any training in dementia.
DiscussionIn recent decades, dementia researchers have shown increasing interest in informal caregivers who provide care to patients owing to several reasons. First, dementia prevalence is increasing significantly and this trend is associated with a growing demand for patient care. Second, questions are being raised about whether or not informal caregivers will be available in the future. Last of all, these topics are being examined in the context of reforms to the healthcare and social welfare systems.9
Dementia, given its chronic, progressive nature, is associated with a growing need for care. Families feel obliged to provide this care to the patient, and have come to be the main providers of long-term care. This being the case, families tend to set up networks of informal or supporting caregivers who complete tasks for the patient. The fact that they are not paid indicates monetary and social savings1–5 with regard to direct costs (which does not reflect the indirect or intangible costs10). Their labour is fundamental, as it enables patients to remain in the family household for longer periods of time. On this topic, we should note the lack of differences between patients in our study and those reported in prior studies.4,11,12 In three-quarters of the cases, patients continued to live at home, although we are beginning to see other different care models, such as rotation between different relatives’ households (7.9%), presence of an FC (11.6%), and day care attendance (20%).
Society assumes that women are to be responsible for caring for dependent people, based on a series of arguments regarding the way they are raised, the values they supposedly embrace, and their role in society. Conventional wisdom holds that women are better prepared to care for both the patient and the patient's home, since this is merely an extension of the typical activities that women have learnt to carry out as wives and mothers.13 Our study confirms this tendency since most PCs (72.1%) are women with very well-defined characteristics that have already been listed by other authors4,9,14,15: homemakers with a low educational level who are directly related to the patient (generally daughters) and who either live with the patient or nearby (P<.01). This profile is exemplified by a generation of women, middle-aged at present, whose training has channelled them into a caregiving role, as has been mentioned before.
Numerous studies show that caring for patients with Alzheimer disease is extremely stressful.16 Levels of anxiety and depression are higher among caregivers than in the rest of the population; we also see increased consumption of psychoactive drugs17 and poorer self-reported health among caregivers.18 Regarding those variables, PCs in our study did not differ from those in previous studies; 29.2% presented physical problems and 36.9% presented emotional problems (depression and/or anxiety).
Being responsible for patient care requires a great deal of the caregiver's time, and this makes it extremely difficult to combine employment with performing care tasks. Managing a relative with dementia and engaging in paid work is often not feasible, especially in more advanced stages of the patient's disease. As a result, women – as primary caregivers – too often have to give up their paid employment temporarily or indefinitely, or pass up any opportunities of seeking paid employment.19 Although 36.4% of the PCs in our study were actively employed, 13.1% had reduced their working hours in order to care for the patient and 5.4% had left their jobs for the same reason. We have not found any prior studies on dementia that reflect this extremely transcendental aspect of dementia care. The most immediate consequence is the economic loss suffered by the entire family unit, added to the limits imposed on the caregiver's personal development and ability to build social relationships and support networks.
Mediterranean cultures still maintain the tradition of caring for patients in the family home, whereas other models of care, including hiring FCs and residential care for patients in early stages, are now widespread in northern European countries.20 We believe that understanding why a PC assumes responsibility for an ill relative is extremely relevant, not only for understanding the structure of informal care, but also for detecting excessive caregiver burden. Recall that as many as 75% of the PCs in our study cited moral obligation as their reason for providing care, and 15.5% would resort to residential care for the patient if they possessed the necessary means. In any case, most PCs (71%) count on the support of other family members acting as SCs. With this in mind, it should be said that many published studies tend to assess the characteristics and functions of PCs without considering the possibility of there being other caregivers.4,9,11–13 Our analysis of caregiver characteristics showed that SCs were also predominantly female (60.5%), directly related to the patient (mostly daughters) (P<.01), and with intermediate to low educational levels. They tend to perform tasks that are simple or less time-consuming, such as participating in the patient's leisure or stimulation activities (82.3%). They also assist with activities of daily living (37.1%), but tend not to take charge of the more complex tasks such as medical care management (27.4%) or general patient management (17.9%); these processes fall to the PC.
Since this study is intended to evaluate different types of caregivers, we will now address the AC. The striking difference here is the predominance of males (73.3%) who are middle-aged, have a slightly higher educational level (primary school in 62.2% and secondary school in 31.1%), are actively employed, and live far from the patient. Considering our results, it seems clear that sex, kinship (P<.001) and household arrangement are the main variables determining which family member will assume the role of caregiver.14,21
As stated previously, our dementia patients are cared for in the family home under the supervision of a PC and 1 or more SCs. This may be an effect of Mediterranean culture; it may also point to poor development of social policy in Spain as exemplified by how long it took for families to receive the monetary stipends established by the Spanish law promoting personal autonomy and care for dependent people (Ley de dependencia, ratified on 5 October 2006).22 In the province of Alicante, Gomis et al. measured a mean waiting period of 293 days before dementia patients could be assessed in order to receive benefits, and 368 days before their cases were resolved,23 between the date cited above and 2008. This could explain why only 20% of the patients in our study attend day care and only 11.6% have FCs, who in 89% of all cases are paid by the family itself.
People who provide care to dementia patients have a heavier burden than do caregivers of patients with other illnesses or physical disabilities.15,24–26 With this in mind, training caregivers will help improve the way they perceive and approach their daily lives.27–29 We must stress the lack of dementia education in caregivers of all types (especially formal caregivers) since less than a third of the total had any training in dementia.
Our study's main contribution is that it goes beyond merely describing the PC and provides a detailed analysis of the network of caregivers assisting dementia patients, the roles they play, and their reasons for providing care. Based on our analysis, women are clearly the key players in this network, whether as PCs, secondary or supporting caregivers, or FCs (despite their lack of dementia education); men are largely absent. These women who manage and accompany patients tend to do so out of moral duty, and in many cases, lack of sufficient economic means for residential care. Nevertheless, the important changes taking place in modern society will have an impact on the system of informal care for dementia patients. The basic tendency is a decrease in traditional care for patients in the family household owing most of all to the gradual disappearance of the extended matriarchal family. This change is caused by the entry of women (PCs) into the labour market, decreasing birth rates, and increases in the number of separated and divorced couples.6,7
Social changes promote the development of new care models, including one that is very visible at present: the involvement of more people of both sexes, with pre-established roles and motives. Understanding how a patient's care is structured will make patient management an easier task.
However, we would like to point out some limits that should be considered when interpreting the results. First of all, a selection bias may be present since not all of the patients seen in the 4 neurology consults were included; we excluded those who refused to participate and any whose PC could not be located. Secondly, there may be an informer bias, since the same informer provided all data corresponding to the caregivers/relatives. Our relatively small group of patients and low numbers of subjects in certain caregiver groups (formal or absent caregivers) may limit the possibility of extrapolating results to the general population. Lastly, considering that the purpose of our study is restricted to describing the caregiver network, we have not entered into economic factors or provided an exhaustive description of the physical or psychological illnesses derived from caregiving.
In conclusion, the marked social changes which are occurring, and their transcendental impact on dementia care, give rise to the need to understand new care models for this type of patients: number of people involved, roles fulfilled, networks established, problems detected, etc. Understanding and describing these models will eventually promote the development and implementation of social welfare policies and guarantee that caregivers receive adequate assistance and support. It is therefore necessary to perform larger studies in different geographical areas in order to confirm and expand on our findings.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Toribio-Díaz ME, et al. Red de cuidadores informales de los pacientes con demencia en la provincia de Alicante, descripción de sus características. Neurología. 2013;28:95–102.
This study was featured as an oral presentation at the 62nd Annual Meeting of the SEN, held in Barcelona in November 2010.