Charles Bonnet syndrome is a rare condition which usually affects elderly patients, especially women, due to ophthalmological involvement, whether due to retinal or anterior segment disease.1,2 We report a case of Charles Bonnet syndrome in a young patient with bilateral atrophy of the optic nerve secondary to intracranial hypertension due to cerebral venous thrombosis.
Our patient was a 44-year-old man who started to present multiple cerebral venous sinus thrombosis of unknown origin at the age of 30. Smoking was the only risk factor he presented at the time of thrombosis. Sequelae of thrombosis were partial seizures with secondary generalisation and sensory symptoms and intracranial hypertension with bilateral oedema of the optical nerve. Treatment was started with acenocoumarol, carbamazepine, a lumboperitoneal shunt, and fenestration of both optical nerves, which did not resolve atrophy. At the age of 40, as partial seizures decreased and 3 electroencephalography studies revealed normal results, we decided to suspend antiepileptic treatment.
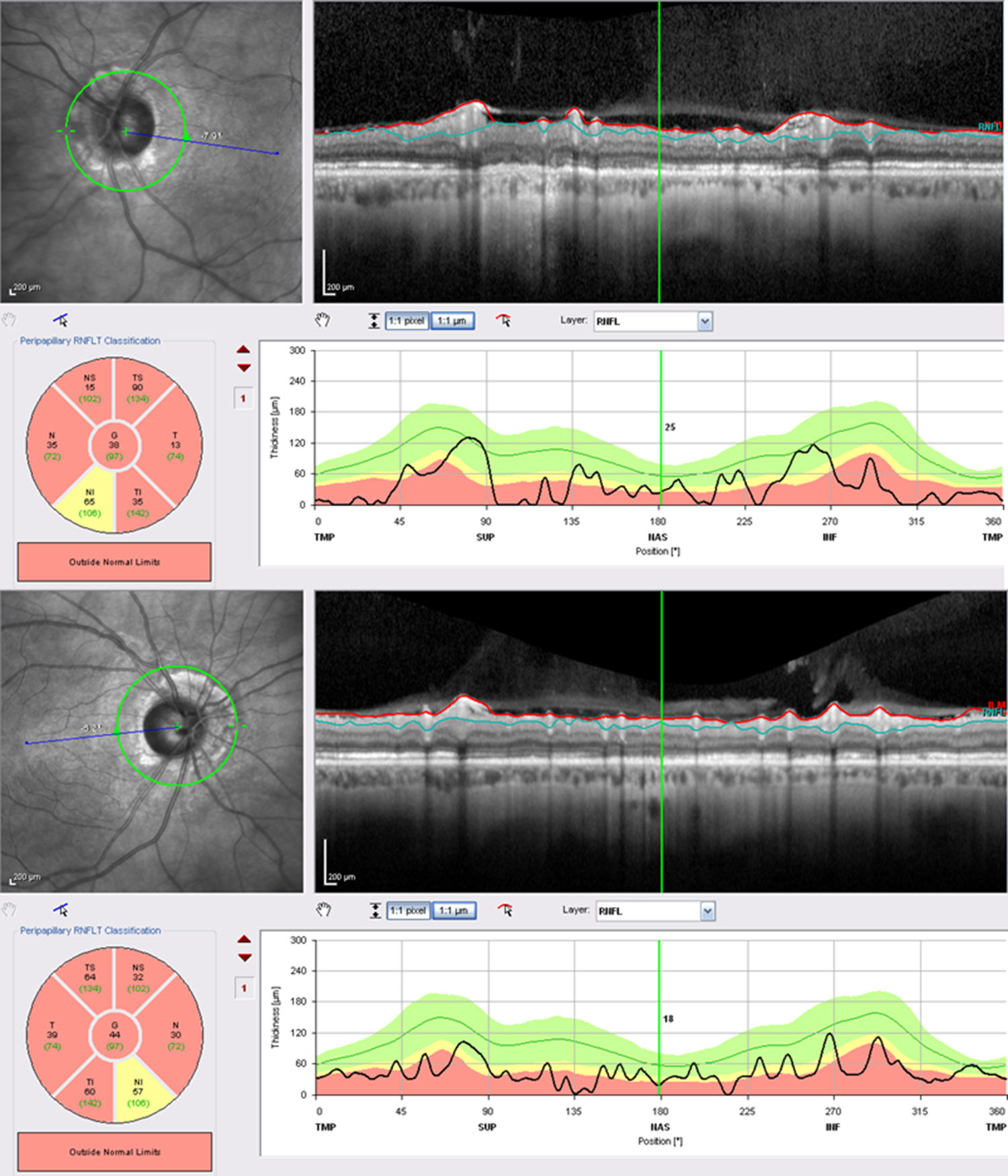
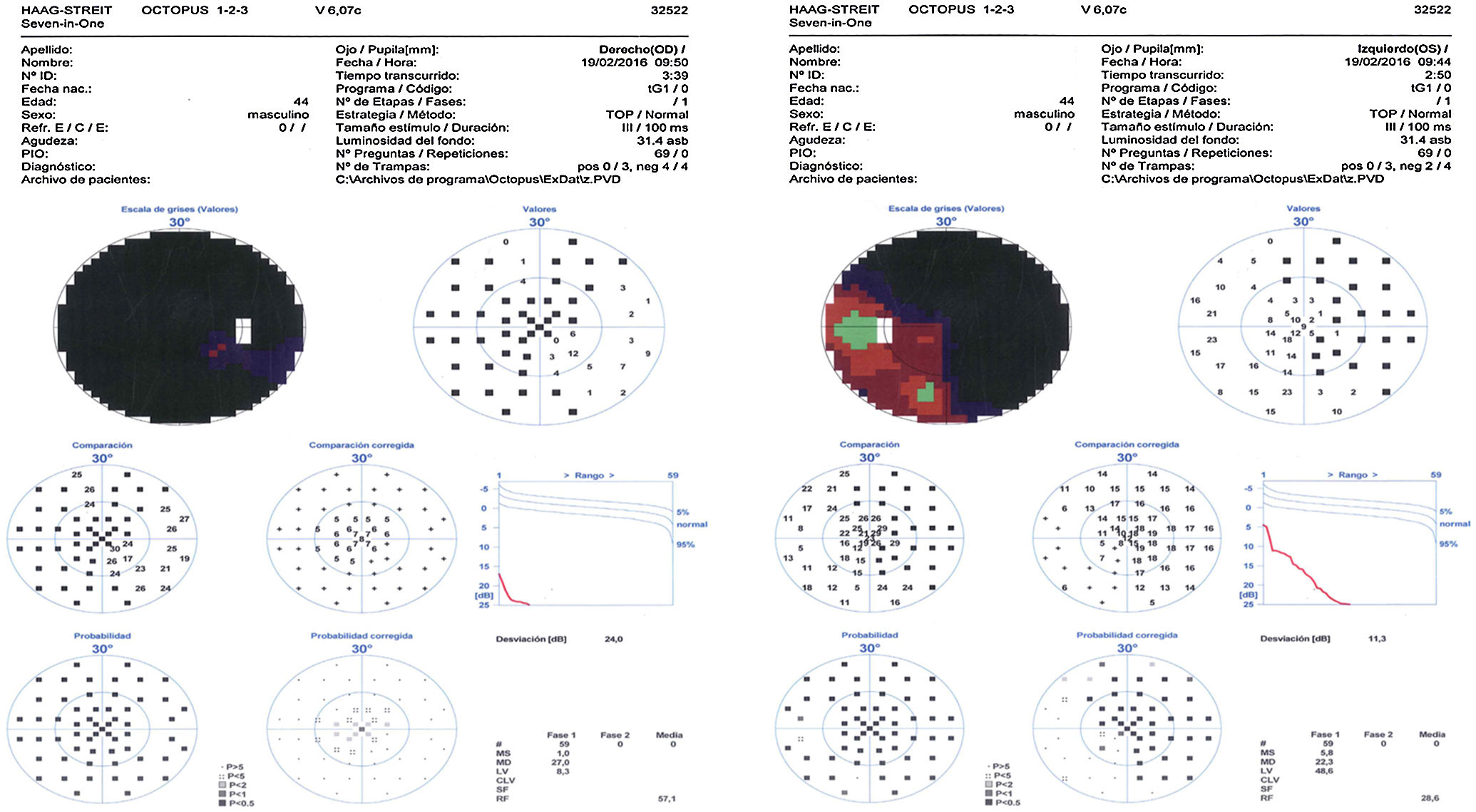
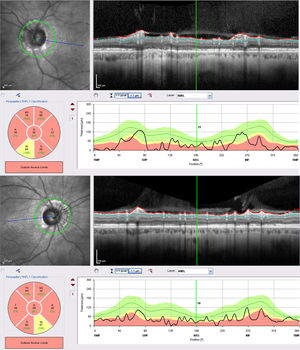
At the age of 42, he developed visual hallucinations of serpentine elements, lasting more than 10minutes; we requested a magnetic resonance imaging (MRI) study to rule out occipital alterations, due to suspicion of sinus rethrombosis. No changes were detected with regards to the previous MRI studies. We requested an additional electroencephalography; results were considered normal for the patient's age. Since then, the patient has reported seeing a yellow car recurrently appearing at different points of the visual field, in both monocular and binocular vision. Episodes lasted from seconds to hours, with no associated symptoms, disorientation, or headaches. The patient did not associate the visions with fatigue, any particular activity, or with changes to light conditions or position. He was fully aware of the phenomenon and reported that hallucinations caused him no discomfort; therefore, no new treatment was started. Visual acuity was 0.4 in the right eye and 0.25 in the left. He presented severe atrophy of both optic nerves (Fig. 1) and severely restricted visual field (Fig. 2).
Charles Bonnet syndrome is described as visual hallucinations in patients with vision loss. The syndrome has classically been described in elderly patients, especially women.3 It consists of a type of hallucinosis, since the patient is fully or partially aware of the phenomenon, which usually involves a high level of anxiety; hallucinations manifest suddenly, with no voluntary control. Duration ranges from seconds to days.
Most case series report more severe visual impairment than in our case, with the syndrome manifesting in patients with macular degeneration, cataracts, or glaucoma.4 It has also been associated with such eye treatments as photodynamic therapy, laser retinal photocoagulation, and injection of anti-angiogenic agents. Before establishing a diagnosis, and given the patient's history, it is important to rule out such other causes of visual hallucinations as inflammatory, toxic-metabolic, infectious, and especially neurological diseases, such as epilepsy, migraine, or Lewy body dementia.5 In this case, there was high suspicion of epilepsy due to occipital lobe involvement, given the appearance of simple hallucinosis; with more complex hallucinations, it becomes more improbable.
Aetiopathogenesis of the syndrome remains unknown. The most frequently considered theories attribute it to deafferentiation; according to this hypothesis, sensory deficiency due to vision loss would cause endogenous activation of the visual cortex.2 No model is completely accepted, and none explains why the majority of patients with impaired vision do not present hallucinations. Therefore, many authors postulate a possible link between the syndrome and the presence or risk of cognitive impairment.6 However, this association is yet to be demonstrated.
In our case, despite the patient's good visual acuity, the origin of hallucinations may be related with a severely impaired visual field due to atrophy of the optical nerve secondary to intracranial hypertension.
As previously described,7 severely impaired visual field due to optic tract lesions may trigger neuronal deafferentiation and the development of Charles Bonnet syndrome in patients with relatively good visual acuity.
In conclusion, Charles Bonnet syndrome is a complex set of symptoms of increasing incidence, and requires a multidisciplinary approach including ophthalmologists, neurologists, and psychiatrists in order to avoid misdiagnosis and prescribe correct treatment. Epilepsy and Charles Bonnet syndrome may coexist, revealing neuronal network dysfunction.8 Further studies are needed to achieve greater understanding not only of the syndrome but also of the neurophysiological basis of hallucinations.
Please cite this article as: Cifuentes-Canorea P, Camacho-Bosca I, Perucho-González L, Santos-Bueso E. Síndrome de Charles Bonnet en paciente joven con antecedentes de epilepsia. Neurología. 2019;34:488–490.