Cerebral hyperperfusion syndrome (CHS) is a rare but very severe complication of carotid revascularisation surgery. We present a case with an extremely rare form of presentation.
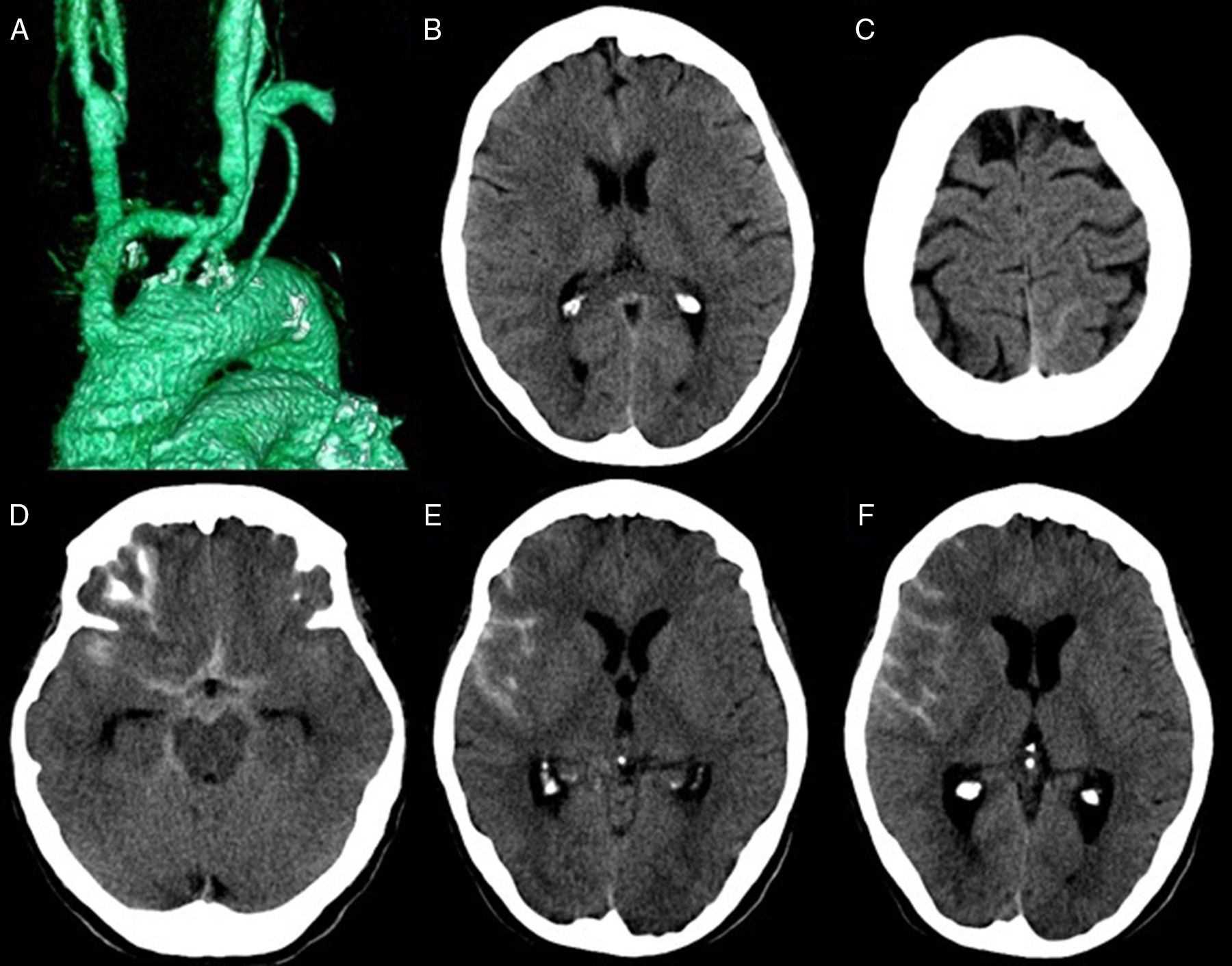
Our patient was a 57-year old woman with a personal history of smoking, type 2 diabetes mellitus, arterial hypertension, dyslipidaemia, and chronic lower limb ischaemia, who was admitted due to right subclavian steal syndrome. An angiography study revealed occlusion of the brachiocephalic trunk from its origin, proximal stenosis (50%) at the origin of the left common carotid artery, and proximal stenosis (80%) of the left subclavian artery. She then underwent reconstruction of the supra-aortic trunks with a bypass from the aortic arch to the bifurcation of the brachiocephalic trunk and to the left common carotid artery using Dacron grafts (Fig. 1A). The patient progressed favourably until postoperative day 5, when she developed intense, holocranial, pulsatile headache associated with nausea; headache did not improve with traditional analgesics. The general and neurological examinations yielded normal results, with unusual blood pressure (BP) values (165/85mmHg). A head CT scan showed a small subarachnoid haemorrhage (SAH) (Fig. 1B and C). In light of these findings, we requested an arteriography, which did not reveal presence of aneurysm, other vascular malformations, arterial dissection, signs suggestive of reversible cerebral vasoconstriction, or other causes of SAH. We suspended acetylsalicylic acid, which the patient was taking, and started treatment with labetalol to reduce BP to below 140/90mmHg, which slightly improved the patient's clinical condition. The headache intensified 2 days later, with predominantly right-sided hemicranial pain, and an increased sensation of nausea. We performed a new head CT scan, which revealed signs of rebleeding (Fig. 1D-F). A transcranial Doppler ultrasound showed increased mean flow velocity in both middle cerebral arteries (MCA), which was more pronounced in the right MCA (110cm/s; left MCA: 80cm/s). Results of a new angiography study were normal. Suspecting a diagnosis of CHS, we referred the patient to the internal medicine ward for monitoring and strict control of BP. Subsequent progression was favourable, with progressive resolution of symptoms and the SAH. A new angiography study performed one month later showed no alterations.
(A) Supra-aortic CT scan with volumetric reconstruction showing a bypass originating in the ascending aorta with distal anastomosis in the brachiocephalic trunk and in the left common carotid artery (Y-shaped bypass graft). (B and C) Head CT scan showing a small SAH in the anterior interhemispheric fissure (B), and the left posterior parietal sulcus (C). (D-F) Head CT scan showing an SAH in the suprasellar cistern, anterior interhemispheric fissure, and the right Sylvian fissure (D), as well as in right convexity sulci (E and F).
CHS is an infrequent complication, typically associated with carotid revascularisation procedures. Most reported cases have been associated with stenting or endarterectomy; however, the syndrome has also been reported in patients undergoing extracranial-intracranial bypass, and less frequently in supra-aortic bypass (SAB).1 Impaired cerebral autoregulation has been proposed as the pathogenic mechanism in brains affected by chronic ischaemia, which present difficulties adapting to a new situation of excessive blood flow. In this context, CHS seems to be more frequent when multiple revascularisations are performed in a single procedure. Other reported risk factors observed in our case are history of arterial hypertension and diabetes mellitus, the use of antiplatelets, and the persistence of postoperative systemic hypertension.1–3
CHS may manifest as cerebral oedema, intracranial haemorrhage (ICH), and very rarely as SAH; isolated SAH has not been described in cases of CHS secondary to SAB.4–7 The appearance of ICH has been observed to occur from several hours to 28 days after the procedure1; specifically, in cases of SAB, ICH has been reported to occur on day 1 to 7 after the procedure4–7; our patient presented signs of SAH on day 5 and a new bleeding episode on day 7.
The main clinical manifestations of CHS are altered level of consciousness, headache, neurological impairment, and seizures. Our patient presented intense, predominantly right-sided pulsatile headache, one of the most frequent manifestations of the disease.2
Transcranial Doppler ultrasound is highly useful in diagnosing excessive cerebral blood flow, with an increase of over 100% in mean flow velocities after revascularisation being compatible with CHS. In our case, we observed increased mean flow velocities, mainly in the right MCA, but there was no preoperative study against which to compare.
The use of vasodilators (hydralazine, nitrates, calcium channel blockers, etc.) is not recommended; the antihypertensive treatments of choice are labetalol and clonidine, which have no impact on cerebral circulation.8 Our case only required treatment with labetalol, which was sufficient to control BP and symptoms.
In conclusion, CHS is an infrequent but possible complication in SAB. CHS may progress to cerebral oedema, intracerebral haemorrhage, and subarachnoid haemorrhage, with isolated subarachnoid haemorrhage being extremely rare.
Please cite this article as: Díaz-Díaz A, Otermin-Domínguez E, Ponce-Marrero P, Hernández-Vicente G, Falero-Pérez R. Hemorragia subaracnoidea tras bypass de troncos supraaórticos: una presentación infrecuente del síndrome de hiperperfusión cerebral. Neurología. 2019;34:491–492.