Health systems in numerous countries around the world are suffering a serious burden as a consequence of the COVID-19 pandemic. As a result of this situation, the follow-up of such chronic diseases as dementia may be at risk. Similarly, neuropsychiatric complications related to lockdown measures may also be neglected; Argentina’s lockdown has been the longest implemented in Latin America. This study aims to determine the frequency of the different types of medical consultations for neurocognitive disorders and the predictors for requiring consultation since the beginning of the lockdown.
MethodsWe performed a descriptive, observational, cross-sectional study based on data collected through an online survey.
ResultsData were collected on 324 participants, with 165 (50.9%) having had at least one medical consultation. Consultations were held by telephone in 109 cases (33.6%), by e-mail in 62 (19.1%), by video conference in 30 (9.3%), and at the emergency department in 23 (7.1%). Predictors of requiring consultation were Clinical Dementia Rating scores ≥1 (P < .001) and diagnosis of Alzheimer disease (P = .017). Higher Neuropsychiatric Inventory scores were found in the group of respondents who did require medical consultation (P < .001), but no significant differences were found between groups for Zarit Burden Interview scores.
ConclusionWe identified a high prevalence of behavioural disorders and caregiver burden during lockdown. Nevertheless, only 50% of respondents had sought medical consultation (by telephone or email in 52.7% of cases). Care of people with dementia must be emphasised, guaranteeing follow-up of these patients.
Varios países del mundo padecen una grave carga en sus sistemas de salud como consecuencia de la pandemia por COVID-19. Esta realidad pone en riesgo el seguimiento de patologías crónicas como las demencias. Asimismo, la atención de las posibles complicaciones neuropsiquiátricas relacionadas al aislamiento preventivo de la población (cuarentena), que en el caso de Argentina, se considera la más prolongada de Latinoamérica. El objetivo del presente trabajo es determinar la frecuencia de las distintas modalidades de consulta médica en relación a la patología neurocognitiva del paciente y las variables predictoras de consulta desde el inicio de la cuarentena.
MétodosEstudio descriptivo observacional, transversal basado en la recolección de datos a través de una encuesta.
ResultadosHubo 324 participantes, 165 (50,9%) de los cuales realizaron al menos una consulta médica. Frecuencia de modalidades de consulta: teléfono, 109 (33,6%); correo electrónico, 62 (19,1%); videoconsulta, 30 (9,3%); servicio de emergencias, 23 (7,1%). Predictores de consulta: Clinical Dementia Rating ≥1 (p < 0,001); diagnóstico: Alzheimer (p = 0,017). Se encon-traron puntajes más altos del Inventario Neuropsiquiátrico (NPI) en el grupo que ha realizado consultas médicas (p < 0,001). Dicha diferencia no fue observada en el puntaje de la escala decarga del cuidador (Zarit).
ConclusiónEvidenciamos alta prevalencia de trastornos conductuales en pacientes y de sobrecarga en cuidadores durante la cuarentena. Solamente el 50% accedió a una consulta médica (52,7% por modalidad telefónica y correo electrónico). Es necesario extremar los cuidados en personas con demencia, garantizando el seguimiento de su patología.
Healthcare systems in numerous countries around the world are severely overburdened due to the COVID-19 pandemic, caused by the novel coronavirus SARS-CoV-2.1 Resources and efforts are urgently being redistributed as part of the response to the pandemic; this process will disproportionately affect countries with weak economies and vulnerable populations, including individuals with cognitive impairment or dementia. Latin American and Caribbean countries present unstable economic development, fragile healthcare systems, vast economic disparities, and high prevalence of dementia. The pandemic has had a concerning selective impact on cognitive disorders in the region, creating tensions in specialised healthcare systems and exacerbating health inequities.2
Neurology departments have changed their activities in response to the pandemic: most neurologists are currently contributing to the management of patients with COVID-19, which has frequently been prioritised over the follow-up of patients with chronic neurological conditions.3
It is important to be aware of the challenges facing elderly people and those with existing conditions, such as dementia, who are now confined to their homes and have become more vulnerable. In the early stages of development, cognitive disorders frequently present with behavioural symptoms,4 resulting in caregiver burden of variable severity.5
Since the beginning of the pandemic, news media have reported chaotic and dangerous situations, which may have caused fear among the population; this has led to delays in patients contacting healthcare systems, negatively affecting the follow-up of chronic conditions and the prevention of new comorbidities.3
Dementia, and particularly advanced dementia, is a significant risk factor for patients with COVID-19: patients with dementia present higher rates of mortality due to COVID-19 than those without the condition (62.2% vs 26.2%).6 Furthermore, the clinical presentation of COVID-19 in patients with dementia may be atypical (behavioural changes or exacerbation of dementia progression, with fever being infrequent); this hinders early detection and hospitalisation, leading to poorer outcomes in this population group. Therefore, we must ensure proper follow-up of these patients in this unprecedented situation.
In Argentina, lockdown measures were put in place on 20 March 2020, at a critical moment of the pandemic.7 At that time, the Ministry of Health ordered the cancellation of outpatient consultations at hospitals and other healthcare institutions, with care provision restricted to emergency situations; this measure was gradually eased, and in-person consultations were restored, with stricter protocols in place. Modern telemedicine was also implemented in some centres.8 This has led to a drastic renewal of the healthcare system, which is not free of difficulties for some elderly patients, many of whom live in homes without sufficient access to technology.
These developments have led to significant problems: firstly, there is a considerable risk that the follow-up of patients with dementia (who are at greater risk from COVID-19) may be interrupted; secondly, it is difficult to access healthcare resources in the event of cognitive or behavioural changes resulting from the pandemic, prolonged confinement, or stress.2
Primary objectiveThe primary objective of this study was to determine the frequency with which different methods of medical consultation were used since the beginning of lockdown by the caregivers of patients with neurocognitive disorders.
Secondary objectivesWe also aimed to define the variables associated with medical consultations and emergency consultations during the lockdown period (age, sex, level of schooling, level of caregiver burden [Zarit Burden Interview; ZBI9], type of dementia, severity of dementia [Clinical Dementia Rating; CDR10], and behavioural manifestations [Neuropsychiatric Inventory; NPI11]), as well as the variables associated with use of video consultations (age and level of schooling).
Material and methodsType of studyWe performed a cross-sectional, observational, descriptive study based on data gathered through a survey of patients’ caregivers.
Study populationAnonymised data were collected using a survey completed on a voluntary basis by formal and informal caregivers of patients with cognitive disorders or dementia of different levels of severity, who had visited Hospital Dr. César Milstein (Buenos Aires, Argentina) at some time, for a variety of reasons (referral to specialist departments, neurocognitive assessment, second opinion consultations, family counselling, outreach lectures, cognitive workshops, etc); we established no restrictions based on age or the aetiology of cognitive disorders. We also distributed the survey among relatives or caregivers who attended support groups attached to the Asociación de Lucha contra el Mal de Alzheimer y alteraciones semejantes (“Association Against Alzheimer Disease”), both in Buenos Aires and at the association’s other centres. We excluded patients who did not have caregivers older than 18 years, who could not be contacted, and/or who were unable to complete the survey for technical reasons.
Instrument: surveyWe used e-mail and mobile instant messaging applications to distribute a self-administered questionnaire to caregivers. We collected data on patients’ and caregivers’ age and sex, aetiology of the patients’ cognitive disorders, the relationship between patient and caregiver, caregivers’ level of schooling, exacerbation of behavioural symptoms (NPI symptom items) or caregiver burden (ZBI) during lockdown, and the method of consultation during lockdown (telephone, e-mail, video consultation, emergency department). Data were collected between 24 April and 1 July 2020. During this period, Buenos Aires was under phases 1, 2, and 3 of lockdown.
Statistical analysisIndependent variables in the statistical analysis were patients’ and caregivers’ sociodemographic characteristics (caregiver age, sex, level of schooling, and relationship to the patient; patient age, sex, CDR score, and diagnosis), ZBI score, and NPI score. Descriptive statistics are expressed as mean (standard deviation) or median (interquartile range [IQR]), as appropriate. In the bivariate analysis, we used the Kruskal-Wallis test and the Mann-Whitney U test for non-parametric variables and the t test, χ2 test, and analysis of variance (ANOVA) for parametric variables. Statistical analysis was conducted using the SPSS statistics software (version 25).
Ethics approvalThe study is considered a low-risk observational study according to the International Conference on Harmonization Good Clinical Practice guidelines, the latest review of the Declaration of Helsinki (1964, revised in Tokyo [1975], Venice [1983], Hong Kong [1989], and Fortaleza [2013]), and the regulations of the Buenos Aires municipal healthcare authorities on the protection of participants in healthcare research. This study was approved by the Research Ethics Committee of Hospital Dr. César Milstein.
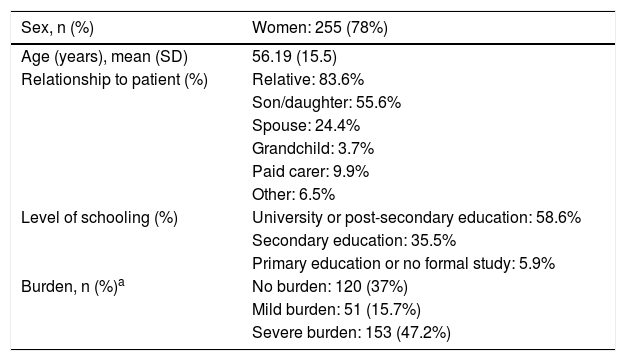
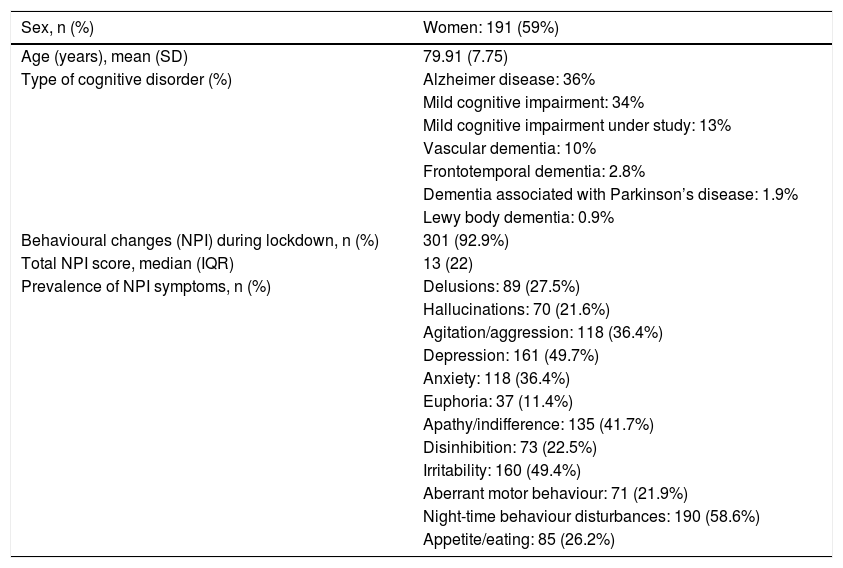
ResultsA total of 324 caregivers responded to the survey. Caregivers’ and patients’ characteristics are summarised in Tables 1 and 2, respectively.
Caregiver characteristics (N = 324).
| Sex, n (%) | Women: 255 (78%) |
|---|---|
| Age (years), mean (SD) | 56.19 (15.5) |
| Relationship to patient (%) | Relative: 83.6% |
| Son/daughter: 55.6% | |
| Spouse: 24.4% | |
| Grandchild: 3.7% | |
| Paid carer: 9.9% | |
| Other: 6.5% | |
| Level of schooling (%) | University or post-secondary education: 58.6% |
| Secondary education: 35.5% | |
| Primary education or no formal study: 5.9% | |
| Burden, n (%)a | No burden: 120 (37%) |
| Mild burden: 51 (15.7%) | |
| Severe burden: 153 (47.2%) |
Patient characteristics (N = 324).
| Sex, n (%) | Women: 191 (59%) |
|---|---|
| Age (years), mean (SD) | 79.91 (7.75) |
| Type of cognitive disorder (%) | Alzheimer disease: 36% |
| Mild cognitive impairment: 34% | |
| Mild cognitive impairment under study: 13% | |
| Vascular dementia: 10% | |
| Frontotemporal dementia: 2.8% | |
| Dementia associated with Parkinson’s disease: 1.9% | |
| Lewy body dementia: 0.9% | |
| Behavioural changes (NPI) during lockdown, n (%) | 301 (92.9%) |
| Total NPI score, median (IQR) | 13 (22) |
| Prevalence of NPI symptoms, n (%) | Delusions: 89 (27.5%) |
| Hallucinations: 70 (21.6%) | |
| Agitation/aggression: 118 (36.4%) | |
| Depression: 161 (49.7%) | |
| Anxiety: 118 (36.4%) | |
| Euphoria: 37 (11.4%) | |
| Apathy/indifference: 135 (41.7%) | |
| Disinhibition: 73 (22.5%) | |
| Irritability: 160 (49.4%) | |
| Aberrant motor behaviour: 71 (21.9%) | |
| Night-time behaviour disturbances: 190 (58.6%) | |
| Appetite/eating: 85 (26.2%) |
IQR: interquartile range; NPI: Neuropsychiatric Inventory; SD: standard deviation.
Medical consultations during lockdown: 165 respondents (50.9%) consulted healthcare professionals at least once, with 45 (13.8%) using more than one method of consultation.
Methods of consultation: 52.7% of respondents consulted via telephone (109; 33.6%) or email (62; 19.1%), 30 (9.3%) used video consultation, and 23 (7.1%) consulted through the emergency department.
Variables associated with medical consultation- 1
Disease progression (CDR score): CDR ≥ 1: 122 (57.5%) vs CDR = 0.5: 43 (38.4%); P < .001 (χ2).
- 2
Diagnosis: Alzheimer-type dementia: 71 (59%) vs non–Alzheimer-type dementia: 94 (45.9%); P = .017 (χ2).
- 3
Total NPI score: median NPI score (IQR) was 20 (34) in patients who consulted and 9 (17) in those who did not; P < .001 (Mann-Whitney U test).
- 4
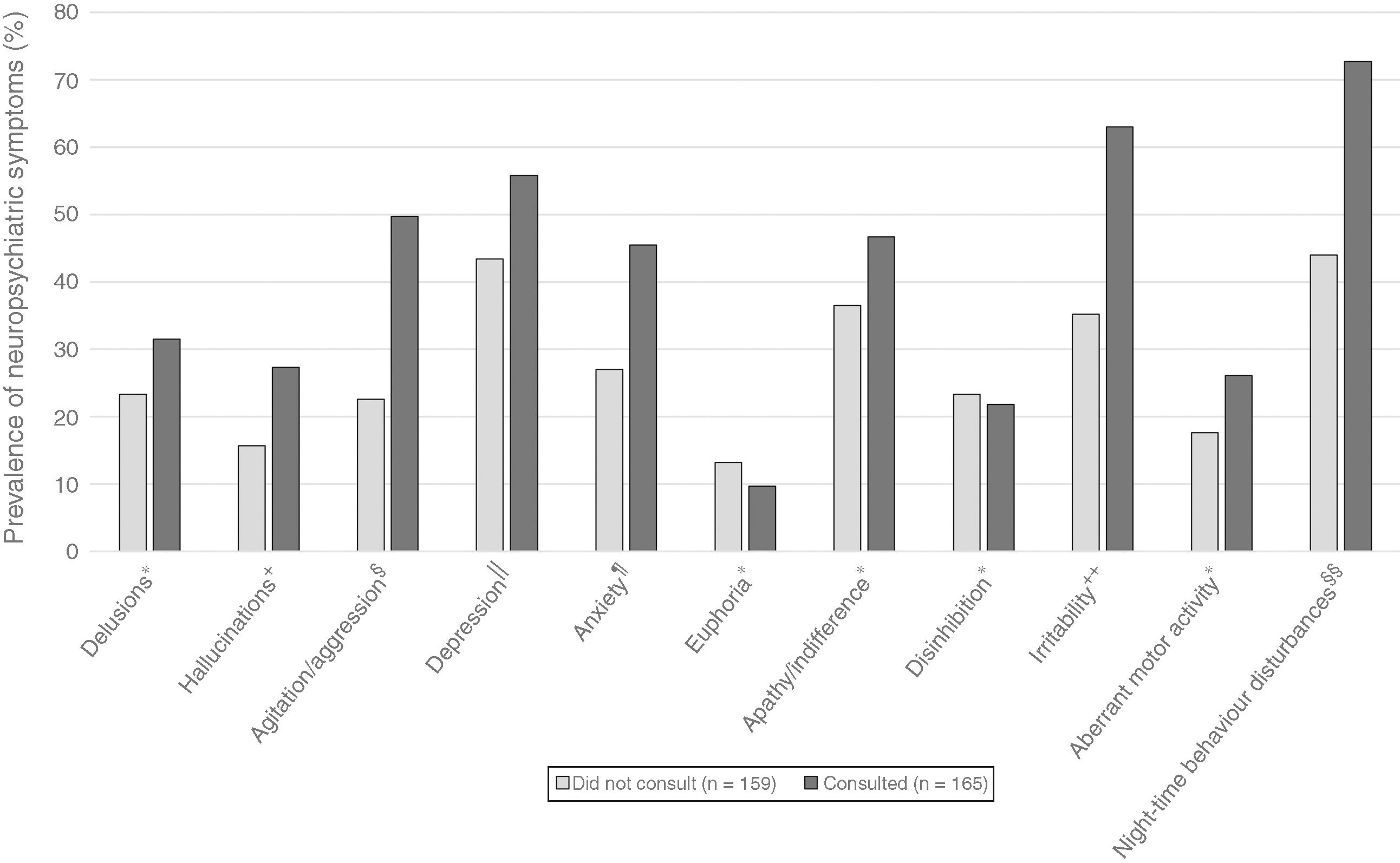
NPI symptom items: patients who consulted presented greater prevalence of hallucinations (P = .008), agitation/aggression (P < .001), depression (P = .0017), anxiety (P < .001), irritability (P < .001), and night-time behaviour disturbances (P < .001) (χ2). Data on NPI symptom items are presented in Fig. 1.
- 5
ZBI score: no statistically significant differences in caregiver burden were identified between caregivers who did and did not consult (median score [IQR]: 53 [28] vs 56 [26]; P = .37 [Mann-Whitney U test]).
- 6
Caregiver age, sex, and level of schooling: no statistically significant differences were identified (t test).
- 1
Disease progression (CDR score): CDR ≥ 1: 20 (9.4%) vs CDR = 0.5: 3 (2.7%); P = .002 (χ2).
- 2
Diagnosis: Alzheimer-type dementia: 11 (9.2%) vs non–Alzheimer-type dementia: 12 (5.9%); this difference was not statistically significant (χ2).
- 3
Total NPI score: median NPI score (IQR) was 37 (59) in patients who consulted and 12 (21) in those who did not; P < .001 (Mann-Whitney U test).
- 4
NPI symptom items: patients who consulted presented greater prevalence of hallucinations (P = .008), agitation/aggression (P = .003), anxiety (P < .001), irritability (P < .001), and aberrant motor behaviour (P = .009) (χ2).
- 5
ZBI score: no statistically significant differences in caregiver burden were identified between caregivers who did and did not consult the emergency department (median score [IQR]: 55 [17] vs 53 [28]; P = .9 [Mann-Whitney U test]).
- 6
Caregiver age, sex, and level of schooling: no statistically significant differences were identified (t test).
- 1
Caregiver age: caregivers who used video consultation were younger than those who used other methods of consultation (P = .03).
- 2
Caregiver level of schooling: no statistically significant differences were identified (t test).
The populations of numerous countries have been placed under preventive isolation (quarantine) as a result of the COVID-19 pandemic, which represents a true challenge for healthcare systems around the world,12 and particularly in Latin American countries. In Argentina, the infection was first detected on 3 March, 64 days after the first case was reported in China. Since then, the government of Argentina has introduced a range of measures to mitigate the impact of the pandemic; a multiple-phase lockdown implemented on 20 March remains in place in the Buenos Aires Metropolitan Area, which has a population of 15 million and presents a high COVID-19 incidence rate.8 In this context, our findings show the significant prevalence of neuropsychiatric symptoms during lockdown in a study population from this region (both patients and caregivers). Over 90% of patients presented neuropsychiatric alterations; 63% of caregivers showed signs of burden, with nearly half presenting severe burden. However, despite the high prevalence of behavioural alterations, only 50% of respondents consulted at least once during lockdown.
It should be noted that most studies in the literature report that confinement has negative psychological consequences, with some suggesting that these effects may be extensive, severe, and long-lasting.13 However, these conclusions are drawn from population studies; to date, no study has examined the effects of lockdown on the elderly population with cognitive impairment and dementia. According to Paola Barbarino, the executive director of Alzheimer’s Disease International, the most vulnerable population segments were overlooked when countries rushed to implement lockdown measures, exacerbating feelings of anxiety and loneliness.14
Regarding the methods of consultation, we observed that caregivers older than 60 years mainly consulted via telephone and e-mail, with only 9% of participants using the video consultation system; this small percentage corresponded to caregivers aged under 60 years.
Patients who consulted mainly had Alzheimer-type dementia; CDR scores ≥1; high prevalence of hallucinations, depression, anxiety, irritability, and night-time behaviour disturbances; and higher NPI scores than those who did not consult medical professionals.
Patients who directly consulted the emergency department (on-call service) presented higher NPI scores and greater prevalence of disruptive symptoms, and frequently presented aberrant motor behaviours and hallucinations.
Argentina is currently at a critical stage of the pandemic, with a considerable rise in COVID-19 cases and deaths, as well as secondary effects related to the pandemic and the prolonged confinement period. Elderly individuals with cognitive disorders and dementia, who are at high risk from COVID-19, must be able to continue with their treatment and have access to medical consultations, beyond the classic in-person model. The high prevalence of mental health disorders in the elderly population must be a priority in the region’s healthcare agenda.2 It is noteworthy that half of the patients and caregivers surveyed did not consult at any time, despite the high prevalence of neuropsychiatric symptoms. The digital divide and the scarcity of technological resources in patients’ homes may contribute to the social exclusion of this population with regard to the use of more technologically complex methods of consultation at this critical time.
Neurology departments must reconsider their working practices to ensure that patients with neurological disorders are able to access the care they need, and work to develop appropriate safety protocols and offer different methods of medical consultation.15 Telemedicine via video consultation may only be useful for a limited number of older patients. We propose that telephone and e-mail consultation should be considered as simple, accessible tools for the follow-up of this population group during the pandemic, enabling early interventions based on patients’ clinical condition pending the implementation of more complex telemedicine systems.
ConclusionPublic health management requires rapid decision-making and profound changes in response to the pandemic; however, we must not neglect the general management of all patients, nor underestimate the emotional impact of the pandemic and lockdown on this group of patients and their families.
Research efforts during the pandemic should contribute high-quality information that may improve the care provided to the population in times of crisis.
Conflicts of interestThe authors have no conflicts of interest to declare.
This study was made possible by the collaboration of the Argentinian Association Against Alzheimer Disease (Asociación de Lucha contra el Mal de Alzheimer y alteraciones semejantes; ALMA); Sandra Virgolini of the León Tucumán Foundation; ALMA’s Chascomús and Mar del Plata centres; Nazareno Molina, actor and writer of the play on Alzheimer disease Una espina en el zapato; Silvina Heisecke, the head research assistant at CONICET; and Marilena Mena-Palacios, social worker at the Alicia Moreau de Justo Centre for Promotion, Prevention, and Rehabilitation.
Please cite this article as: Sorbara M, Graviotto HG, Lage-Ruiz GM, Turizo-Rodriguez CM, Sotelo-López LA, Serra A, et al. COVID-19 y la pandemia olvidada: el seguimiento de las enfermedades neurocognitivas durante la cuarentena en Argentina. Neurología. 2021;36:9–15.