The autism spectrum disorders are group of conditions characterised by qualitative impairments in social communication; in the interaction and imagination; with a restricted range of interests and stereotyped repetitive behaviours. Frequently, there is a delay in the age of detection, and therefore in starting multidisciplinary evaluations and interventions, which may result in a worst prognosis and an impaired quality of life for both children and parents. The aim of our study was to describe some clinical and epidemiological data including the age of detection and main initial complaints present in children with autism disorders from a paediatric neurology centre.
Patients and methodsA total of 393 medical records of consecutive cases with a diagnosis of autism spectrum disorders were reviewed.
ResultsAutism was diagnosed in 82.1% of the cases, unspecified pervasive disorder in 9.9%, and Asperger syndrome in 4.8%. Sixty percent of autistic children presented with a language disorder as their main complaint. The average age of detection was 4 years.
ConclusionsCompared with other countries, age of detection is delayed. A Primary Care based screening and surveillance are required in order to improve prognosis and quality of life of children with an Autism Spectrum Disorder.
Los trastornos del espectro autista son un grupo de desórdenes que se caracterizan por problemas en la socialización, en la comunicación verbal y no verbal; y por patrones de conducta repetitivos e intereses restringidos. La edad en la que se identifican varía según sea la intensidad e instalación de los síntomas iniciales del padecimiento. En las mejores condiciones de atención, las primeras manifestaciones se notan alrededor de los doce meses de edad y el diagnóstico se define entre los dos y tres años. Con frecuencia la búsqueda de atención médica y el inicio de las intervenciones se retrasan por la dificultad en la identificación de signos incipientes del trastorno. Los objetivos de nuestro estudio fueron describir las manifestaciones clínicas iniciales y aspectos epidemiológicos en pacientes con sospecha diagnóstica de espectro autista referidos a un centro neuropediátrico.
Pacientes y métodosSe realizó análisis sistemático retrospectivo de 393 expedientes consecutivos con algún trastorno del espectro autista.
ResultadosEntre los casos revisados 82,1% correspondieron al diagnóstico de autismo, 9,9% trastorno inespecífico, 4,8% Asperger y 3% con síndrome de Rett. El promedio de edad a su primera evaluación fue de 4,4 años. El 62,5% de los casos con autismo fueron detectados por problemas de lenguaje.
ConclusionesLa edad de diagnóstico comparada con otros países sigue siendo tardía. Es necesario favorecer la detección temprana para mejorar el pronóstico y la calidad de vida de los niños con trastorno del espectro autista.
Pervasive developmental disorders (PDDs) or autism spectrum disorders (ASD) are groups of disorders originating in the prenatal period and caused by abnormalities in the formation and functioning of neural circuits. These disorders are clinically and aetiologically heterogeneous.1 Their main symptoms are deficiencies in the capacity for reciprocal social interaction, together with verbal and non-verbal communication deficiencies, abnormal interests, and repetitive and restrictive behavioural patterns.2,3
The Swiss psychiatrist Bleuler first used the term ‘autism’ in 1912 to refer to paediatric patients with schizophrenia.4 In 1943, Kanner and Asperger used the term independently to describe paediatric patients with communication problems.5,6 When the 3rd edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III) was published in 1980, it included PDD and its diagnostic criteria, rather than the concept of ‘infantile psychosis’ which had been included in earlier versions.7
Recently, 5 forms of PDDs were added to the 10th edition of the International Classification of Diseases (ICD-10) and the latest edition of the DSM-IV-TR. The first form is autism, characterised by severe deficiencies in the areas of social interaction, language, communication, and play, in addition to stereotyped movements, repetitiveness, and little interest in ordinary activities. The second form is Asperger syndrome, in which mental abilities and language are intact in most cases, but socialisation is notably deficient and the patient has little interest in ordinary activities. A third category is Rett syndrome, which as an X-linked dominant disorder mainly affects girls. Patients with this disorder present acquired microcephaly, regression, loss of purposeful use of hands, stereotyped hand motions, severe developmental delays, and other neurological problems. The last 2 categories are PDD-NOS (not otherwise specified), in which children display autistic behaviours without meeting the criteria for placement in one or another of the disorders in the spectrum, and childhood disintegrative disorder, in which psychomotor development is normal but regression with a loss of cognitive ability occurs between 2 and 10 years of age.8,9
Recent epidemiological studies point to a potential increase in cases of autism; for example, in 1985, studies estimated approximately 5 cases per 10 000 individuals, while new estimates report 1 case per 100 children and adolescents.10–14
Early diagnosis in a patient with PDD is particularly difficult. However, when a complete neurological screening is performed in the first year of life, doctors can identify 40% of all children with a PDD.15–17
In this study, we describe the main neurological manifestations and age of diagnosis in 393 patients with different types of PDDs. We also analysed the yearly number of new cases at a centre specialising in care for children with neurological problems.
Patients and methodsSubjectsWe reviewed all consecutive files pertaining to patients diagnosed with a PDD and examined in CENNA, the neurological centre for children and adolescents in Monterrey (Nuevo León) Mexico, between 1968 and 2009. We included all cases with at least 1 consultation with a specialist in paediatric neurology and a neuropsychological assessment confirming the diagnosis of PDD.
For cases recorded between 1980 and 1987, we applied DSM-III diagnostic criteria; for cases from 1987 to 1994, DSM-III-R; for cases from 1994 to 2000, DSM-IV criteria; and after 2000, DSM-IV-TR criteria.
AssessmentsWe began by listing the reasons why cases had been referred to our centre and recorded patients’ medical histories, age, sex, and the results of different neurological assessments. Reasons for referral were defined as follows.
- a.
Speech impairments; language problems affecting either verbal communication (echolalia, prosodic abnormality, incomprehensible language, low vocabulary for the child's age, inability to begin or follow a conversation) or non-verbal communication (problems with body language, taking turns, and understanding sarcasm or jokes).
- b.
Language regression; progressive language loss.
- c.
Complete lack of language or speech, or use of incomprehensible sounds.
- d.
Socialisation problems, including cases of avoiding eye contact, problems developing interpersonal relationships, no desire to display or share interests, and poor expression of emotions.
- e.
Behaviour problems: harm to self or others, uneasiness, or lack of obedience.
- f.
Learning problems such as poor performance at school and difficulties with reading, writing, or mathematics.
- g.
Stereotyped behaviours, whether motor (flapping, swaying, or running in circles) or verbal (repeating words, phrases, or songs).
- h.
Psychomotor delay; delay in motor or psychosocial abilities identified with or without the use of standardised tests of any type.
- i.
Convulsions of any type.
- j.
Deafness.
- k.
Suspected PDD.
The neuropsychological evaluation included an intelligence quotient (IQ) measurement using the Minnesota intelligence scale for children aged 18 months to 6 years; the Wechsler Preschool and Primary Scale of Intelligence (WPPSI) for children aged 3 years and 10 months to 6 years and 7 months; and the Wechsler Intelligence Scale for Children, revised edition (WISC-R) for children aged 6 to 16 years.
The diagnostic criteria for PDD were established based on the Childhood Autism Rating Scale (CARS, 1966), the Autism Spectrum Screening Questionnaire (ASSQ, 1981) by Lorna Wing, and the CENNA inventory of characteristics of autistic children (ICCAN-R, 1992).
We used Schopler and Reichler's psychoeducational profile (PEP, 1972) to evaluate memory, language, visuospatial and visuoperceptual abilities, and fine and gross motor skills. Lastly, we used the Vineland Social Maturity Scale (1984) to measure children's level of social adaptation.
We also analysed the age at which the child first came to the centre and the number of new cases per year. Statistical analysis was performed using the Excel® program by Microsoft® and predictive analytic software SPSS® version 18 (SPSS Inc., Chicago, IL). Data with a continuous distribution were expressed as means and standard deviations. Some categorical variables were contrasted using the chi-square test, or by using the t-test and analysis of variance (ANOVA) when examining more than 2 variables with a normal distribution. Binary logistic regression analysis was performed with presence or absence of each of the autism spectrum disorders as the dependent variable in order to detect any potentially significant associations with age at detection, sex, neuropsychological tests, or anomalies in the electroencephalogram (EEG).
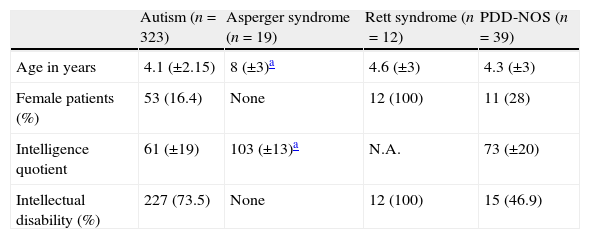
ResultsWe completed a retrospective and descriptive study of a series of 393 cases. In this study, we obtained data from the files of patients diagnosed with PDD according to the tools that were available at the time of diagnosis (Table 1).
Characteristics of pervasive developmental disorders.
| Autism (n=323) | Asperger syndrome (n=19) | Rett syndrome (n=12) | PDD-NOS (n=39) | |
| Age in years | 4.1 (±2.15) | 8 (±3)a | 4.6 (±3) | 4.3 (±3) |
| Female patients (%) | 53 (16.4) | None | 12 (100) | 11 (28) |
| Intelligence quotient | 61 (±19) | 103 (±13)a | N.A. | 73 (±20) |
| Intellectual disability (%) | 227 (73.5) | None | 12 (100) | 15 (46.9) |
N.A.: not available.
The most frequent category was autism, which accounted for 82.1% (n=323) of cases in the series, including 15 cases that were diagnosed before PDD was divided into categories. The next most common category (9.9%, n=39) was PDD-NOS; Asperger syndrome accounted for 4.8% (n=19), and Rett syndrome, 3% (n=12). There were no diagnoses of childhood disintegrative disorder.
PDD was diagnosed in 6 patients using criteria predating DSM-III; in 9 patients using DSM-III criteria; in 62 patients using DSM-III-R criteria; in 160 using DSM-IV; and in 156 using DSM-IV-TR.
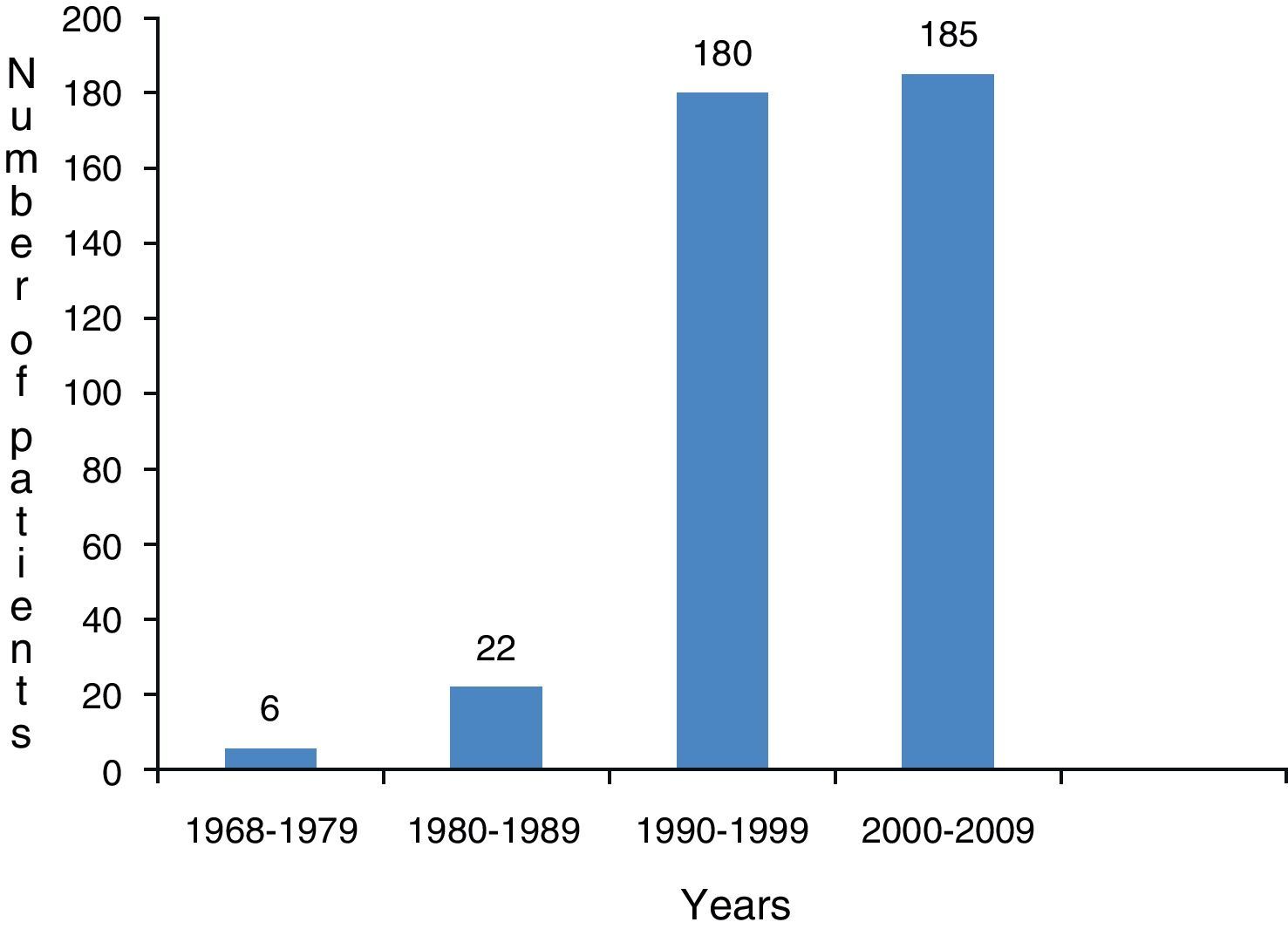
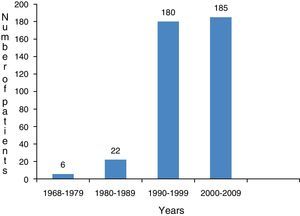
Frequency of new cases per yearThe number of new cases per year is shown in Fig. 1. One of our goals was to determine whether or not age at the time of detection of PDD has decreased. However, the mean age at which autism spectrum disorders are identified did not vary with respect to the chronological year when we compared all of the mean ages at detection for each year using ANOVA (P=.13). The analysis was performed by dividing the sample into 10-year periods and 2 groups corresponding to before and after use of DSM-IV criteria; the mean and significance level remained the same.
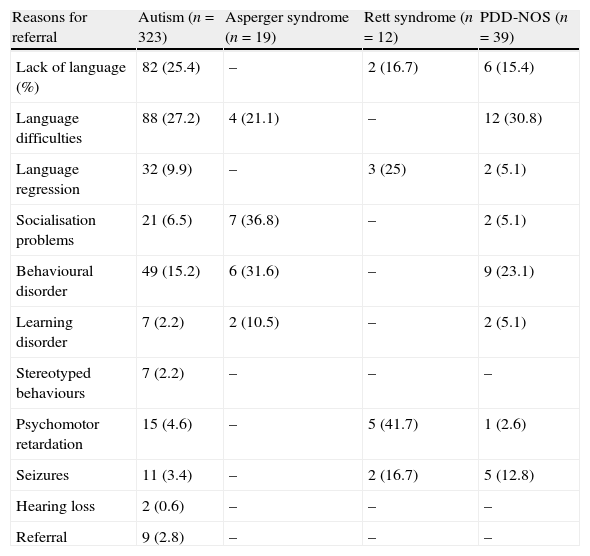
Reasons for referralThe most common reasons for referral throughout the study population were language problems (absence, disorders, or regression of language), found in 58.7% of the cases, followed by behavioural problems in 16.2% of cases and socialisation problems in 7.6%. In 62.5% of the autism cases, the initial symptom was language disorder, whereas the initial symptom was behavioural and socialisation disorder in 68.4% of the cases of Asperger syndrome. Patients with Rett syndrome were most frequently referred due to psychomotor delays (41.7%) and language regression (25%); these 2 motives for concern accounted for 8 of the 12 patients. Reasons for referral are listed in Table 2 (neuropsychological evaluations).
Reasons for referral.
| Reasons for referral | Autism (n=323) | Asperger syndrome (n=19) | Rett syndrome (n=12) | PDD-NOS (n=39) |
| Lack of language (%) | 82 (25.4) | – | 2 (16.7) | 6 (15.4) |
| Language difficulties | 88 (27.2) | 4 (21.1) | – | 12 (30.8) |
| Language regression | 32 (9.9) | – | 3 (25) | 2 (5.1) |
| Socialisation problems | 21 (6.5) | 7 (36.8) | – | 2 (5.1) |
| Behavioural disorder | 49 (15.2) | 6 (31.6) | – | 9 (23.1) |
| Learning disorder | 7 (2.2) | 2 (10.5) | – | 2 (5.1) |
| Stereotyped behaviours | 7 (2.2) | – | – | – |
| Psychomotor retardation | 15 (4.6) | – | 5 (41.7) | 1 (2.6) |
| Seizures | 11 (3.4) | – | 2 (16.7) | 5 (12.8) |
| Hearing loss | 2 (0.6) | – | – | – |
| Referral | 9 (2.8) | – | – | – |
Intelligence quotient was measured in 309 autistic patients; scores of 69 or less were found in 227, meaning that intellectual disability was present in 73.5% (95% confidence interval, 68.5%–78.4%) (Table 1). None of the patients with Asperger syndrome had intellectual disability and their mean IQ score was 103 (range, 77–118). All patients with Rett syndrome had moderate to severe intellectual disability. Intellectual disability was also present in 46.9% of the patients with PDD-NOS (95% confidence interval, 31.2–62.5).
Distribution by sex and ageAges at which PDD was detected ranged from 4 months to 15 years, with a mean of 4.4 years. The mean age in the autistic patient group was 4.1 (±2.15) years. All patients with Asperger syndrome were male, and their mean age at diagnosis was 8 years (±3) (Table 1). As would be expected, all 12 patients with Rett syndrome were female. Age at detection and sex distribution were significantly different in this category (P=.01) compared to other categories in the autism spectrum.
Other neurological findingsIn 4.5% of cases, patients were referred due to experiencing seizures and were later diagnosed with a PDD. EEG was performed on 78 of the 393 patients (19.8%); 37 EEGs (47.4%) revealed an anomaly. Other diseases in addition to the autism spectrum disorder were diagnosed in 3.8% of cases. These included 7 cases of idiopathic epilepsy, 3 cases of tuberous sclerosis, 2 cases of Lennox–Gastaut syndrome, 1 of hypomelanosis of Ito, and 1 of microcephaly.
DiscussionOur study is one of the first to analyse the distribution of patients with autistic traits. It supports existing literature in that it finds classical forms of autism to be predominant, while other categories, such as Asperger or Rett syndrome, account for less than 10% of the total cases.11
In recent decades, there has been an increase in the number of children diagnosed with PDD. This increase appears to be linked to better knowledge of the symptoms of the disorder and the development of new diagnostic tools. The gold standard evaluations for diagnosing PDD are DSM-IV, the autism diagnostic observation schedule (ADOS), and the revised autism diagnostic interview (ADI-R).14
The increase in PDD prevalence is a controversial topic worldwide. Various theories have been used to try to explain this phenomenon, including the shift toward the concept of the ‘autism spectrum’ rather than the concept of a single entity. This accounts for there being more patients with PDD.18 Increased knowledge of autism among the general population may lead to parents, family members or health professionals suspecting such a disorder in young children.19 The current study was carried out in a paediatric neurology centre of reference in northern Mexico, and shows that a significant number of patients have been diagnosed with a PDD in recent decades. However, the prevalence of autism in Mexico is unknown. The strategy for measuring it could involve using a national system of records capable of demonstrating changes in the prevalence of this disorder in an epidemiologically valid way.
Howlin et al. report that mean age of diagnosis in developed countries has dropped from 6.8 years to 2.7 years20; our study shows a mean age of 4 years at referral and diagnosis. Most of the patients suffer from lifelong disability which affects them directly and also has an impact on the dynamic of their families. Although evidence is limited in this area, the general consensus is that early intervention in PDD cases can improve multiple areas of the patient's quality of life.21
Casuistics are somewhat heterogeneous owing to the long time period spanned by the study. Conclusions regarding increases in the number of diagnoses were not easy to analyse due to diagnostic criteria having changed during the study period. This is also problematic when we make comparisons to determine whether disorders are being diagnosed earlier. Even when groups are divided up by decades, half-decades, or by diagnosis before or after publication of DSM-IV criteria, the mean age at diagnosis remains approximately 4 years.
One relevant finding from our study is that language disorders were the initial symptoms of autism in 50%–60% of the cases. This figure is lower than the 80% reported by Tuchman et al. as the percentage of parents who observe language development problems in their autistic children.22 It is possible that language problems being detected later by both parents and primary care doctors would have contributed to the children in that series being diagnosed when they were older. We should also note that language disorders are not limited to patients with PDD. They may be associated with intellectual disability, or be classified as developmental or specific language disorders.23 Differential diagnosis is clinical, and it confirms the presence of abnormalities in other cognitive and behavioural areas that would be typical of PDD. Performing a neuropsychological evaluation is extremely important if there are any doubts about the diagnosis. It also provides information about the patient's cognitive abilities.
Our study highlights the need for longitudinal studies that evaluate how diagnosing a patient before age 2 may affect the patient's quality of life. Checking developmental milestones was only added to Mexico's guidelines for childhood disease prevention and management24 a decade ago. However, it is clear that we need to develop more suitable screening methods for autism spectrum disorders and include them in the guidelines. This will enable the paediatrician, family doctor, nursing staff, and any other professionals in charge of well-child care to recognise signs of PDD and diagnose them as early as possible so that the child can come under the care of a multidisciplinary group of experts. The primary care doctor must be able to recognise suspicious behaviour or signs in order to begin the process of diagnosing and then treating the condition. Recent studies suggest that clinical signs that may point to autism in children younger than 2 years include absence of response when called by name, lack of reciprocal play, lack of motor imitation (does not copy the motor movements of others), problems interacting with others (does not point fingers or try to attract another person's attention), and responding with gestures.23,25
Psychomotor development problems are common in patients with PDDs. Identifying such problems in patients will have important repercussions for making decisions regarding treatment. We found intellectual disability in 73.5% of the cases, a similar percentage to that reported by other authors.26,27 This demonstrates the need to rule out PDD in patients initially diagnosed with mental retardation.
The prevalence of epilepsy in PDD patients ranges from 6% to 38% according to some authors.28–30 Certain forms of epilepsy such as Landau–Kleffner syndrome, West syndrome and continuous spikes and waves during slow sleep are associated with PDD. This is why EEGs should be performed, especially in patients displaying neurological regression. We must thoroughly evaluate any cases that might benefit from anticonvulsants, since the frequency of abnormal EEG readings in patients with PDD and no clinical signs of seizures is about 45.5%.31 In our series, 78 patients had an EEG and 47.4% of those cases had abnormal EEG readings. This was somewhat higher than the rate reported in the literature; also, 4.5% were epileptic. Recent evidence shows that all patients with autism are likely to present abnormal EEG findings when they are analysed under certain conditions. These include poorer integration of the anterior–posterior plane than would be expected at the child's age, and increased neural noise caused by hyperexcitability of the primary somatosensory cortex. The latter may be related to the severity of symptoms of the disorder.32
Although this is a retrospective study based on data from medical records with a moderate selection bias due to the type of institution, we believe it provides important information about the distribution of the different autism spectrum disorders, the age at which the disorder begins to be noticed by parents as a medical problem, and the main symptoms which cause parents to seek care in specialised centres.
In defining PDDs as developmental disorders of the brain that may arise during the prenatal stage due to neuronal network dysfunction, we are considering a number of different causes, such as alterations in the cellular architecture of the central nervous system and/or neurotransmitters.33,34 The most relevant task in current research on autism is searching for aetiological and/or risk factors which, in the near future, will enable us to opt for specific molecular treatments for a disease which is currently severe, disabling, and incurable.
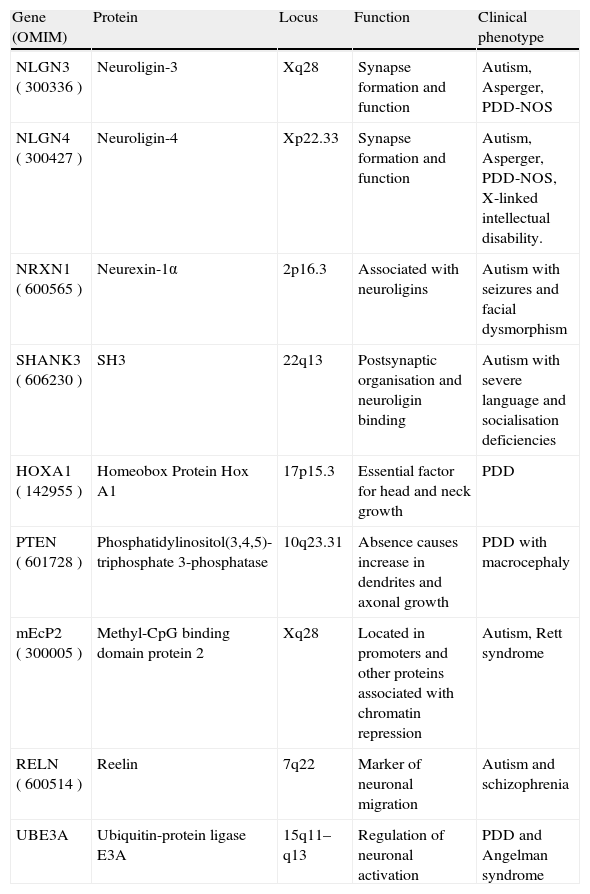
In the past decade, available studies have shown that a wide variety of genetic mechanisms are involved in the aetiology of PDDs. Examples include monogenic disorders such as Rett syndrome; microdeletion or microduplication syndromes; anomalous imprinting; variations in the number of copies; and polymorphisms susceptible to the disorder.35 The autistic behavioural phenotype has been found in more than 100 genetic syndromes, including fragile X syndrome and tuberous sclerosis. Based on these findings, it is now proposed that PDDs be categorised as syndromic or non-syndromic. Even in non-syndromic cases, scientists have identified changes in the sequence or function of various genes, including NLGN3, NLGN4, PTEN, SHANK, etc. (Table 3).35,36
Genes involved in non-syndromic autism.
| Gene (OMIM) | Protein | Locus | Function | Clinical phenotype |
| NLGN3 (300336) | Neuroligin-3 | Xq28 | Synapse formation and function | Autism, Asperger, PDD-NOS |
| NLGN4 (300427) | Neuroligin-4 | Xp22.33 | Synapse formation and function | Autism, Asperger, PDD-NOS, X-linked intellectual disability. |
| NRXN1 (600565) | Neurexin-1α | 2p16.3 | Associated with neuroligins | Autism with seizures and facial dysmorphism |
| SHANK3 (606230) | SH3 | 22q13 | Postsynaptic organisation and neuroligin binding | Autism with severe language and socialisation deficiencies |
| HOXA1 (142955) | Homeobox Protein Hox A1 | 17p15.3 | Essential factor for head and neck growth | PDD |
| PTEN (601728) | Phosphatidylinositol(3,4,5)-triphosphate 3-phosphatase | 10q23.31 | Absence causes increase in dendrites and axonal growth | PDD with macrocephaly |
| mEcP2 (300005) | Methyl-CpG binding domain protein 2 | Xq28 | Located in promoters and other proteins associated with chromatin repression | Autism, Rett syndrome |
| RELN (600514) | Reelin | 7q22 | Marker of neuronal migration | Autism and schizophrenia |
| UBE3A | Ubiquitin-protein ligase E3A | 15q11–q13 | Regulation of neuronal activation | PDD and Angelman syndrome |
The syndromic component of autism may be found in up to 40% of cases when diagnostic methods such as microarray-based comparative genomic hybridisation are used to identify small losses or gains in genetic material.37
The cases in our study include 5 patients with hereditary diseases, highlighting the importance of genetic evaluation in cases with PDD. Recent guidelines for studying the genetic causes of PDDs are available. The American College of Medical Genetics published its recommendations in 2008, and the American Academy of Pediatrics published its own statement in 2010. Since they are so recent, these recommendations were not completely integrated in our study cases. Despite the fact that genetic studies are being developed and made available in many areas of the world, many countries, including Mexico, face both technological and economic barriers that prevent their routine use. In fact, the capacity to study the genetic causes of autism is even limited in highly specialised neurology centres.38,39 Our group decided to evaluate each PDD case in order to determine what type of study to request, rather than subjecting patients to full diagnostic panels that most of those treated in our centre would be unable to afford.
PDDs are frequently seen in neurology centres. The aetiological perception of these entities has changed, and so have our means of diagnosing and treating them. The solution to providing total care for children with PDDs is twofold. In addition to promoting training for health professionals so as to improve their diagnostic accuracy, we also need infrastructure and staff trained to provide specialised care using the best resources at their disposal.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Bravo Oro A. et al. Manifestaciones iniciales de los trastornos del espectro autista. Experiencia en 393 casos atendidos en un centro neurológico infantil. Neurología. 2012;27:414–20.