Deep brain stimulation (DBS) has represented a qualitative leap in the management of a number of neurological and psychiatric diseases. One of the associated complications is delayed-onset oedema in the parenchyma surrounding the electrodes.
We present the cases of 2 patients with essential tremor who underwent electrode implantation in the ventral intermediate nucleus (VIM) of the thalamus and subsequently developed peri-electrode idiopathic delayed-onset oedema.
Patient 1 was a 67-year-old man with history of recurrent facial angioedema who underwent bilateral implantation of a directional electrode in the VIM. The procedure was completed with no complications. A head CT scan revealed no alterations.
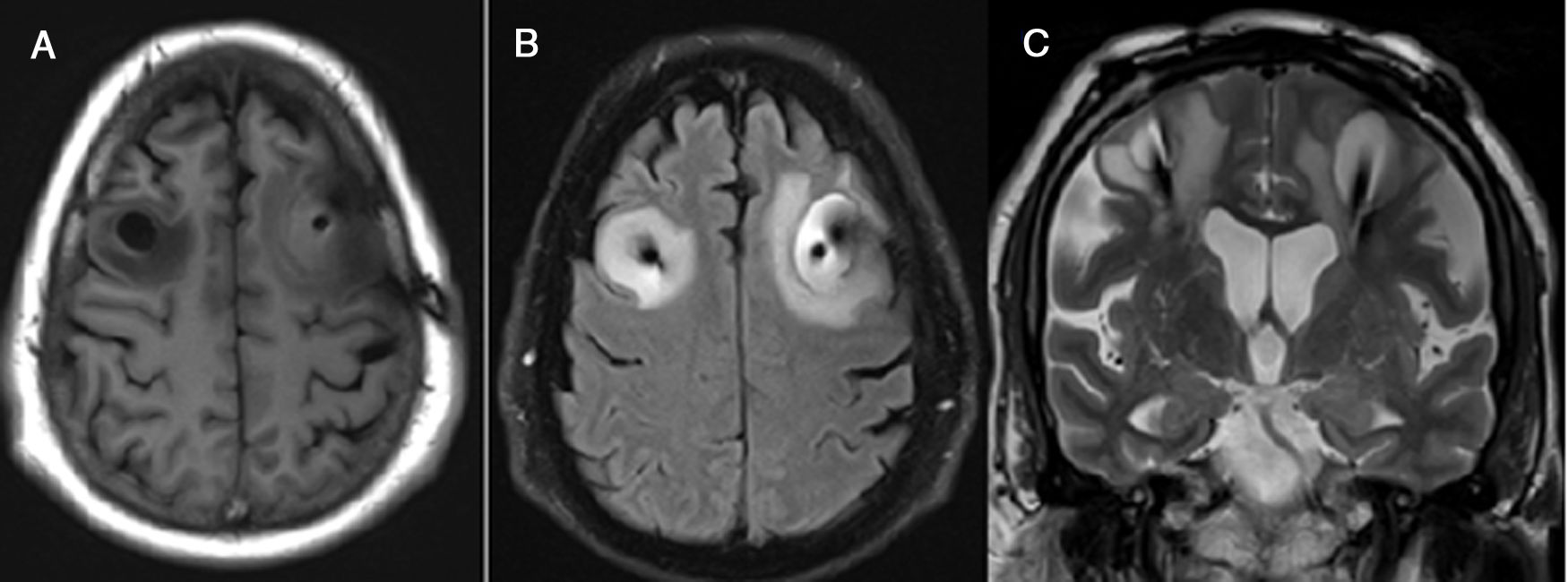
He progressed favourably and was discharged 72hours after the procedure. Two days later, he presented sleepiness, headache, dysarthria, and language impairment. No changes were observed in the intensity of tremor. A CT scan revealed vasogenic oedema around the trajectory of both electrodes; we started empirical treatment with meropenem and dexamethasone. A subsequent MRI scan also revealed vasogenic oedema, with no diffusion restriction and mild open ring contrast enhancement (Fig. 1). These findings are suggestive of inflammation of non-infectious cause; antibiotic therapy was therefore discontinued. The patient progressively improved, with symptoms disappearing on week 5. One year later, he remains asymptomatic, with follow-up neuroimaging studies showing complete resolution of the oedema.
Patient 1: MRI scan revealing cerebral oedema. (A) T1-weighted sequence (axial plane) showing signal hypointensity around the electrodes. (B) FLAIR sequence (axial plane) showing peri-electrode hyperintensity, corresponding to vasogenic oedema. (C) T2-weighted sequence (coronal plane) revealing oval-shaped hyperintensity around the electrodes, compatible with vasogenic oedema.
Patient 2 was a 59-year-old man diagnosed with disabling essential tremor and no other relevant medical history who underwent bilateral implantation of a directional electrode in the VIM. The procedure was uneventful, and a follow-up CT scan yielded normal findings.
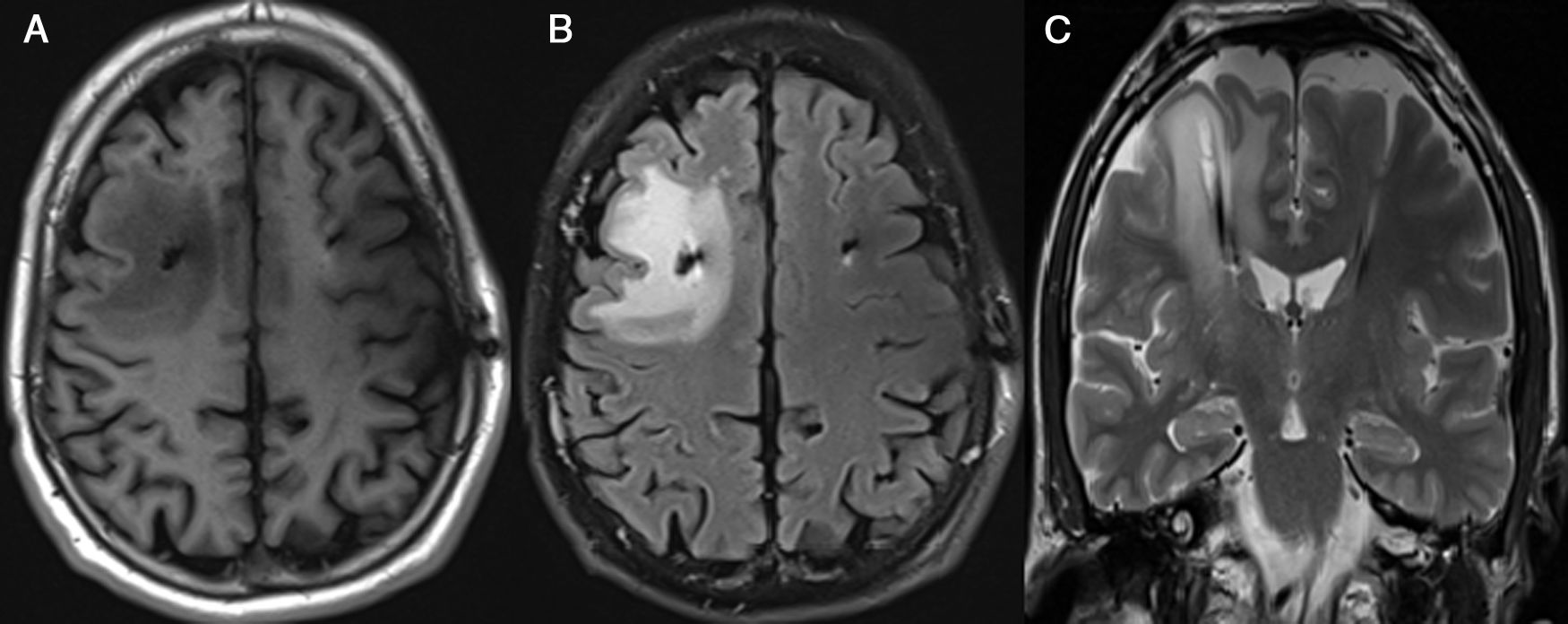
A week after the intervention, the patient presented sleepiness and dysarthria. Tremor, which had improved during the immediate postoperative period, increased slightly in intensity. A CT scan revealed oedema around the right electrode. This was interpreted as an abscess, and antibiotic therapy with vancomycin and ceftazidime was started. A subsequent MRI scan confirmed the presence of vasogenic oedema, showing a hyperintense lesion on T2-weighted sequences and no gadolinium uptake or diffusion restriction (Fig. 2). Antibiotic therapy was discontinued and treatment with dexamethasone was started. Symptoms resolved 10 days later. A 6-month follow-up CT scan showed disappearance of the oedema. A year later, the patient remains asymptomatic.
Patient 2: MRI scan revealing cerebral oedema. (A) T1-weighted sequence (axial plane) showing frontal white matter hypointensity around the right electrode. (B) FLAIR sequence (axial plane) revealing hyperintense signal secondary to vasogenic oedema around the right electrode. (C) T2-weighted sequence (coronal plane) showing a hyperintense area in the right hemisphere.
DBS has led to a paradigm shift in the treatment of disabling essential tremor.1,2 The most frequent adverse reactions include dysarthria, ataxia, and paraesthesia.3 Severe complications are associated with a mortality rate of 0.4%, and leave permanent sequelae in 1% of cases.4,5
Our patients underwent bilateral electrode implantation in the VIM. Both presented subacute neurological deficits several days after the procedure. They received dexamethasone and antibiotic therapy, which were discontinued after infection was ruled out. Symptoms persisted for 34 days in patient 1 and 10 days in patient 2.
Idiopathic delayed-onset oedema secondary to DBS develops in the area surrounding the electrodes and usually appears 72hours after the intervention, in the absence of trauma, vascular complications, or infection. However, it occasionally appears earlier.6,7 Incidence rates range from 0.4% to 39% of all procedures.4 A recently published study of a prospective cohort reports incidence of symptomatic oedema of 31.7%, reaching 100% when asymptomatic patients were included.8
The most common symptom is confusion, with headache and seizures also being frequent.9 Symptoms resolve within 3 months in nearly all published cases. Neuroimaging studies reveal oedema around one or both electrodes; these studies are essential in establishing a correct diagnosis and ruling out other complications. Images rarely display contrast uptake, although mild enhancement may be observed in some cases, as in our first patient.4,10
The series published to date have not found an association between delayed-onset oedema and the surgical technique used or patient history. The most widely accepted hypothesis suggests that delayed-onset oedema is caused by a cytokine-mediated immune response to a foreign body.4 Other authors have suggested that oedema may be secondary to local trauma during electrode implantation.11 History of recurrent angioedema may have played a pathogenic role in our first patient. In this case, increased vascular permeability may have promoted the accumulation of interstitial fluid around the electrode.
This entity should be considered in patients presenting neurological impairment following implantation of electrodes for DBS. Although no specific treatment has been established for the condition, prognosis is good. The use of corticosteroids is controversial. Once diagnosis is confirmed, antimicrobial agents must be avoided.
Please cite this article as: Siso García P, Suárez San Martín E, Saiz Ayala A, Blázquez Estrada M. Edema cerebral idiopático de inicio tardío asociado a estimulación cerebral profunda. Neurología. 2021;36:84–86.