Preeclampsia is a pregnancy complication of unknown aetiology with an estimated frequency of 2%–8%. It is characterised by hypertension after week 20 of gestation in women with previously normal blood pressure, together with proteinuria, or in the absence of proteinuria but with presence of thrombocytopaenia, kidney failure, altered liver function, pulmonary oedema, or neurological symptoms.1 The most frequent neurological symptoms include headache and visual alterations, with isolated oculomotor palsy being exceptional.2 We present the case of a primiparous woman (37 weeks pregnant) whose first neurological symptom of preeclampsia was sixth nerve palsy; we also assess the possible action mechanisms.
Our patient was a 31-year-old woman assessed in the emergency department due to progressive onset of binocular diplopia in the horizontal plane, with no headache, fever, or other focal neurological signs. The neuro-ophthalmological evaluation revealed 20/20 Snellen visual acuity in both eyes, and the eye fundus examination showed well-defined papillae and spontaneous venous pulsation; the confrontation visual field test yielded normal results; esotropia was observed in the primary gaze position with slightly impaired adduction of the left eye. No other neurological alterations were observed. The general examination detected no fever, blood pressure values of 150/90mm Hg, and distal oedema in both lower limbs; a blood analysis revealed thrombocytopaenia with 100000platelets/μL, increased LDH levels (418IU/L), and proteinuria (Table 1). In view of these symptoms, and considering the diagnosis of preeclampsia and findings suggestive of isolated sixth nerve palsy, we requested an MRI study before labour was induced. The MRI study ruled out an underlying intracranial lesion, and labour was induced 24hours after the patient's admission to hospital; a healthy baby was born with no complications. After delivery, the patient presented normal blood pressure values and diplopia progressively improved, fully resolving in 48hours.
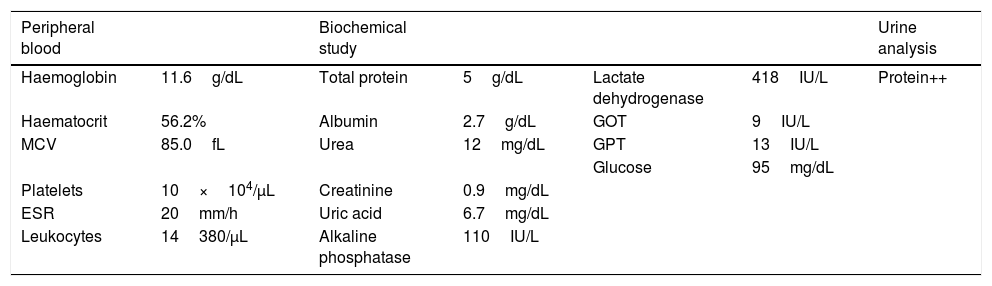
Blood test at admission.
| Peripheral blood | Biochemical study | Urine analysis | ||||
|---|---|---|---|---|---|---|
| Haemoglobin | 11.6g/dL | Total protein | 5g/dL | Lactate dehydrogenase | 418IU/L | Protein++ |
| Haematocrit | 56.2% | Albumin | 2.7g/dL | GOT | 9IU/L | |
| MCV | 85.0fL | Urea | 12mg/dL | GPT | 13IU/L | |
| Glucose | 95mg/dL | |||||
| Platelets | 10×104/μL | Creatinine | 0.9mg/dL | |||
| ESR | 20mm/h | Uric acid | 6.7mg/dL | |||
| Leukocytes | 14380/μL | Alkaline phosphatase | 110IU/L |
ESR: erythrocyte sedimentation rate; GOT: glutamic oxaloacetic transaminase; GPT: glutamate-pyruvate transaminase; MCV: mean corpuscular volume.
Isolated sixth nerve or abducens nerve palsy during pregnancy is exceptional, although isolated cases have been reported.3–6 The action mechanism by which preeclampsia causes neuropathy remains unknown, although the absence of other findings and previous published data in the literature suggest that it may cause vasospasm of the vasa nervorum, causing transient ischaemia that would lead to nerve palsy.6 In our patient, who had no history suggesting an underlying systemic disease, presenting preeclampsia and no fever, intracranial hypertension, or underlying intracranial lesion on MR images, together with the complete resolution of symptoms postpartum, suggest preeclampsia-related sixth nerve palsy.
Please cite this article as: Baidez Guerrero AE, García Lax N, Hernández Clares R, Martín Fernández JJ. Neuropatía aislada del sexto nervio craneal. Una manifestación inusual de preeclampsia. Neurología. 2019;34:620–621.