Cerebral microbleeds are one of the most significant manifestations of cerebral small vessel disease. However, this phenomenon may also be related with less common processes or conditions. For instance, cerebral microbleeds have been described as a complication of sepsis in patients presenting a combination of trigger factors, such as coagulation alterations or hypoxia.1 MRI can be useful for the characterisation and differential diagnosis of these lesions. We present an atypical case of multiple cerebral microbleeds secondary to disseminated intravascular coagulation (DIC) in the context of cardiac arrest.
Clinical caseThe patient was a 76-year-old woman diagnosed with atrial fibrillation, who was hospitalised to undergo ablation. As a complication of the procedure, she developed a cardiac tamponade, which required emergency surgery. During the operation, the patient presented cardiac arrest; pulse was recovered after 5minutes of cardiopulmonary resuscitation and extracorporeal life support. A neurological examination performed 12hours later revealed confusional state, spontaneous eye opening, normal pupillary reactivity, preserved brainstem reflexes, and mild paresis of the left arm, with no other focal neurological deficits. Blood analysis findings were compatible with DIC, with elevated d-dimer levels (7900ng/mL), prolonged prothrombin time (19.1s), a platelet count of 81×103 platelets/μL, and fibrinogen level of 0.84g/L. No significant alterations had been detected in the blood analysis performed at admission.
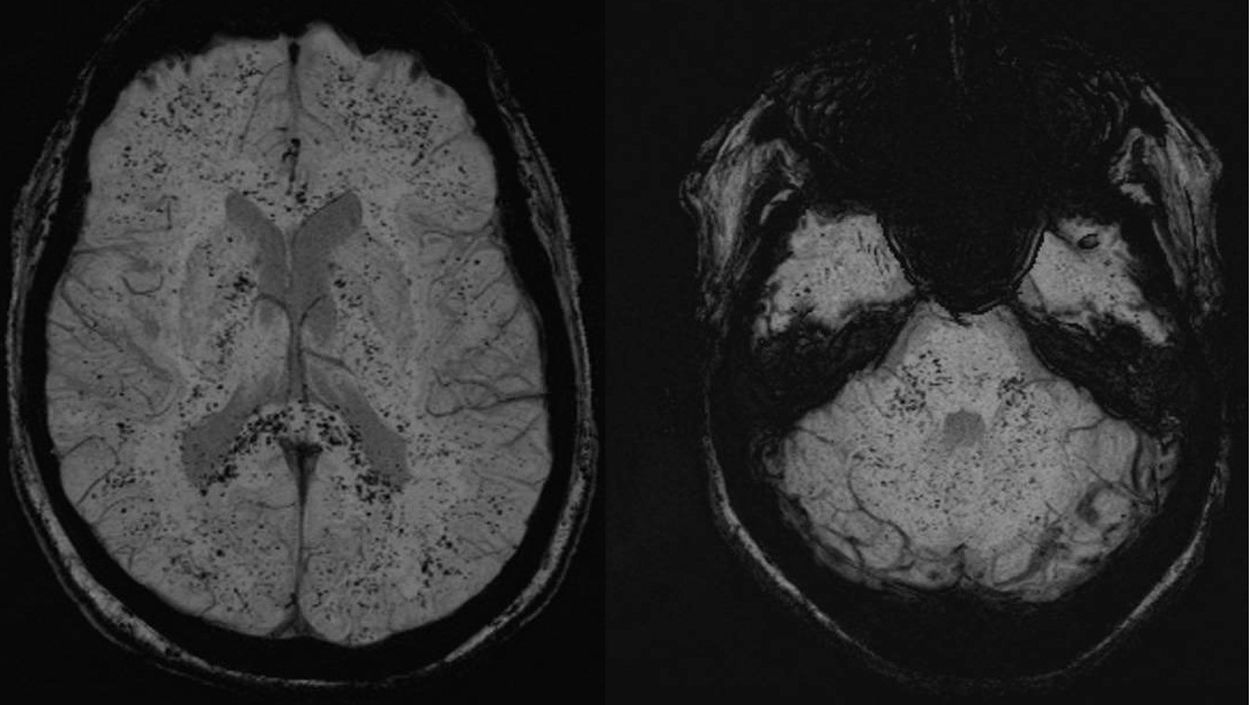
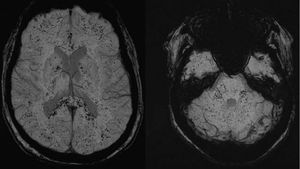
Curiously, brain MRI (Fig. 1) revealed multiple punctiform hypointensities on susceptibility-weighted imaging (SWI) sequences, distributed across both hemispheres, the cerebellum, and the brainstem. These findings are suggestive of diffuse parenchymal microbleeds. No alterations were detected on other imaging sequences. These punctiform haemorrhages had minimal clinical impact, and the patient completely recovered after 4 days. A follow-up MRI study performed a week later revealed persistence of the parenchymal microbleeds, with no changes with respect to the previous study. Three weeks prior to the procedure, a head CT scan had also identified no relevant alterations.
DiscussionThe peculiar imaging findings in this case are compatible with the development of multiple generalised cerebral microbleeds, with the underlying mechanism probably being DIC in the context of cardiac tamponade and subsequent cardiac arrest.
The processes most commonly associated with appearance of cerebral microbleeds are small-vessel diseases, including hypertensive arteriopathy and cerebral amyloid angiopathy.2,3 Less frequent scenarios include moyamoya disease, cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy, posterior reversible encephalopathy syndrome, and radiotherapy-induced lesions.3 All these causes were ruled out in this case due to the patient's clinical characteristics and the normal findings from previous studies, including a head CT scan and blood analysis. Air and fat embolisms share some radiological characteristics.4 However, fat embolism typically presents with diffusion restriction on brain MRI studies, which was not observed in our patient; in the case of air embolism, the associated imaging alterations would have resolved by the time the second MRI study was performed, a week later. Other, rarer entities may also show similar images on SWI sequences; examples include cavernous malformations, haemorrhagic metastases, and partial volume artefacts.5
Some studies have reported similar brain lesions associated with critical illness, such as respiratory insufficiency, infectious encephalitis, and sickle cell disease.6 However, in most cases laboratory findings indicate DIC, which suggests a shared underlying mechanism. It should be noted that hypoxaemia is also common in these situations, and may be involved in the development of bleeding. Hypoxia triggers a cascade of chemical effects in the blood-brain barrier, potentially increasing its permeability, leading to blood extravasation.4
In conclusion, systemic processes liable to cause DIC may occasionally be associated with presence of cerebral microbleeds. SWI sequences are an appropriate tool for detecting and correctly evaluating blood products in this broad differential diagnosis. The patient's clinical characteristics and medical history should guide differential diagnosis.
Please cite this article as: Valenti-Azcarate R, Irimia Sieira P, Esparragosa Vazquez I, Riverol Fernandez M. Microhemorragias cerebrales múltiples asociadas con el desarrollo de coagulación intravascular diseminada. Neurología. 2021;36:88–89.