Lateral-medullary syndrome is often found in patients with vertebrobasilar vascular lesions. On rare occasions, the syndrome is associated with ipsilateral hemiparesis; this is known as Opalski syndrome.1
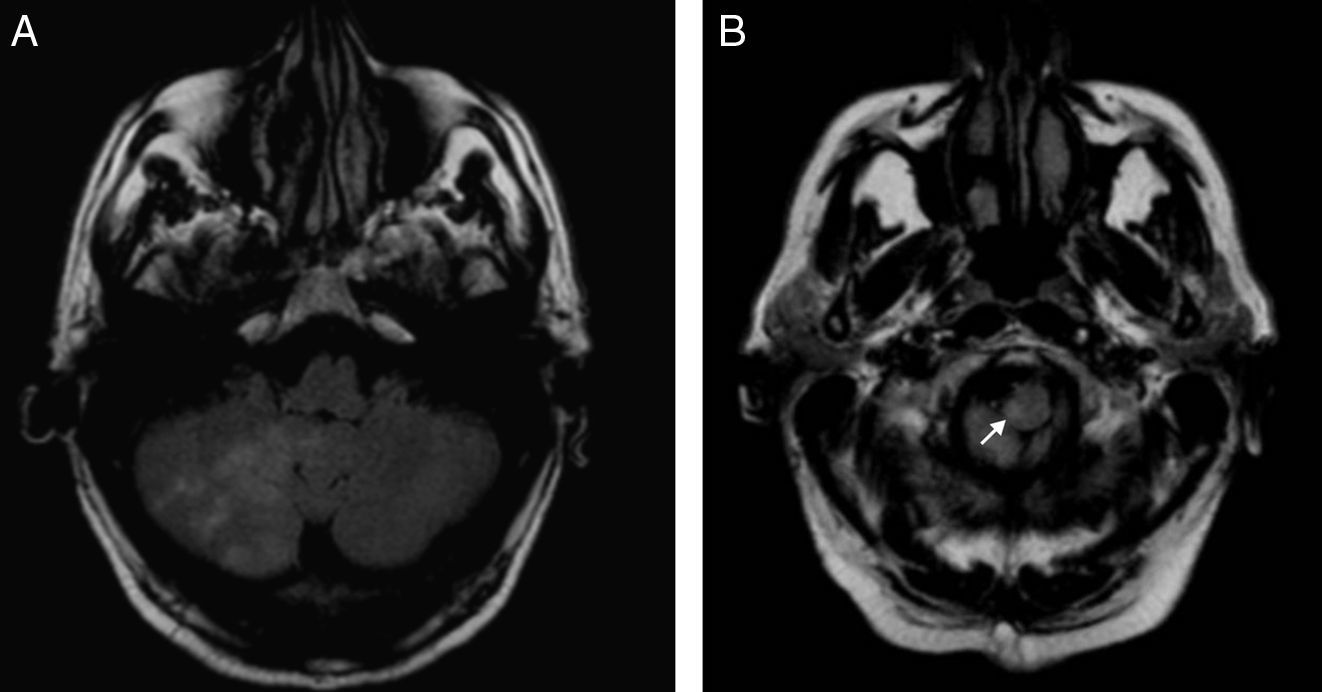
We present the case of a male smoker aged 67 with a history of arterial hypertension, peripheral artery disease, and trigeminal neuralgia. He was undergoing treatment with enalapril, carbamazepine, and baclofen. He was examined following a 12-hour episode of dizziness, nausea, vomiting, and difficulty walking. The initial assessment showed right-sided facial paralysis, mild paresis, dysmetria of the right upper limb, and ataxic gait with lateropulsion. Blood tests (including serum levels of carbamazepine) and cranial CT yielded normal results. The patient was admitted with a diagnosis of cerebral infarct in the vertebrobasilar region which was probably atherothrombotic in origin. Cardioembolic origin was ruled out, and the patient began treatment with antiplatelet drugs. The patient's clinical condition worsened in the first 24h after admission. The examination revealed horizontal-rotary nystagmus, right-sided Horner syndrome, hemiparesis and dysmetria in right upper limbs, and hemihypaesthesia affecting the trunk and left extremities. Arthrokinetic reflex remained intact. Doctors performed a cranial CT that ruled out the presence of haemorrhagic lesions. The patient began anticoagulant treatment, which gradually improved his symptoms. Upon discharge, he still presented right-sided mild nuclear facial paralysis, slight paresis of the right upper limb, left hemihypaesthesia, and ataxic gait. Cranial MRI and MR angiography of the supra-aortic trunks were also performed. Cranial MRI showed acute ischaemic infarct in the bulbar region and right cerebellum, reaching the right cervical region of the spinal cord (Fig. 1A and B). MR angiography of the supra-aortic trunks revealed asymmetries in the diameter of the vertebral arteries. The left vertebral artery was thinner (asymptomatic), especially at its origin and the distal end. The right vertebral artery presented fewer irregularities.
Opalski syndrome is a rare variation of lateral medullary syndrome (Wallenberg syndrome) in which the lesion is associated with ipsilateral hemiparesis.1 An infarct in this region may result from any of several causes, including differences in the diameter of the vertebral arteries,2,3 dissection of the vertebral artery,4 and atherosclerosis, which is the most frequent cause1 and the suspected aetiology in our case.
Based on neuroradiology and autopsy findings, we determined that the lesion was located caudal to the pyramidal decussation.1–3,5,6 Impairment of that structure may explain the ipsilateral paresis, but this causal mechanism is not universally accepted because it is not always accompanied by abnormal reflexes such as the Babinski sign. Some researchers therefore believe that infarct may result from hypotonia secondary to spinocerebellar tract injury, and not from a pyramidal lesion.7 Doctors also disagree as to which artery causes this disorder because of anatomic variability,4 but the vertebral arteries are the ones most frequently involved.3
We present a patient who suffered lateral spinal infarct with paresis ipsilateral to the lesion. This profile suggests Opalski syndrome, a rare presentation of a spinal infarct with a characteristic radiological profile that correlates to the clinical symptoms. Since Opalski syndrome was first described in 1946,8 there have been 15 cases published in the English- and Spanish-language literature.1–10 Nine include cranial MR imaging studies that show lateral medulla oblongata impairment; only 3 also present cerebellar impairment, as in the case of our patient.1,3,6 MR angiography studies are available from 6 cases; vertebral artery involvement was the most frequent finding in these studies.1–5,10
Please cite this article as: Gil Polo C., et al. Síndrome de Opalski: una variante del síndrome medular lateral. Neurología. 2013;28:382–4