Anaesthetic blockade of pericranial nerves is frequently used to treat headache disorders. There is no evidence on indication of this treatment for migraine. We aim to evaluate its effectiveness as a preventive treatment for migraine using specific indication criteria.
MethodsBetween January 2009 and May 2013 we offered pericranial nerve blockade to migraine patients with a history of preventive drug intolerance or failure. We selected patients with tenderness to palpation of at least one greater occipital nerve (GON) or supraorbital nerve (SON). Responses at 3 months were categorised as complete response (no pain), partial response (reduction of at least 50% in severity or frequency of headache episodes), or no response.
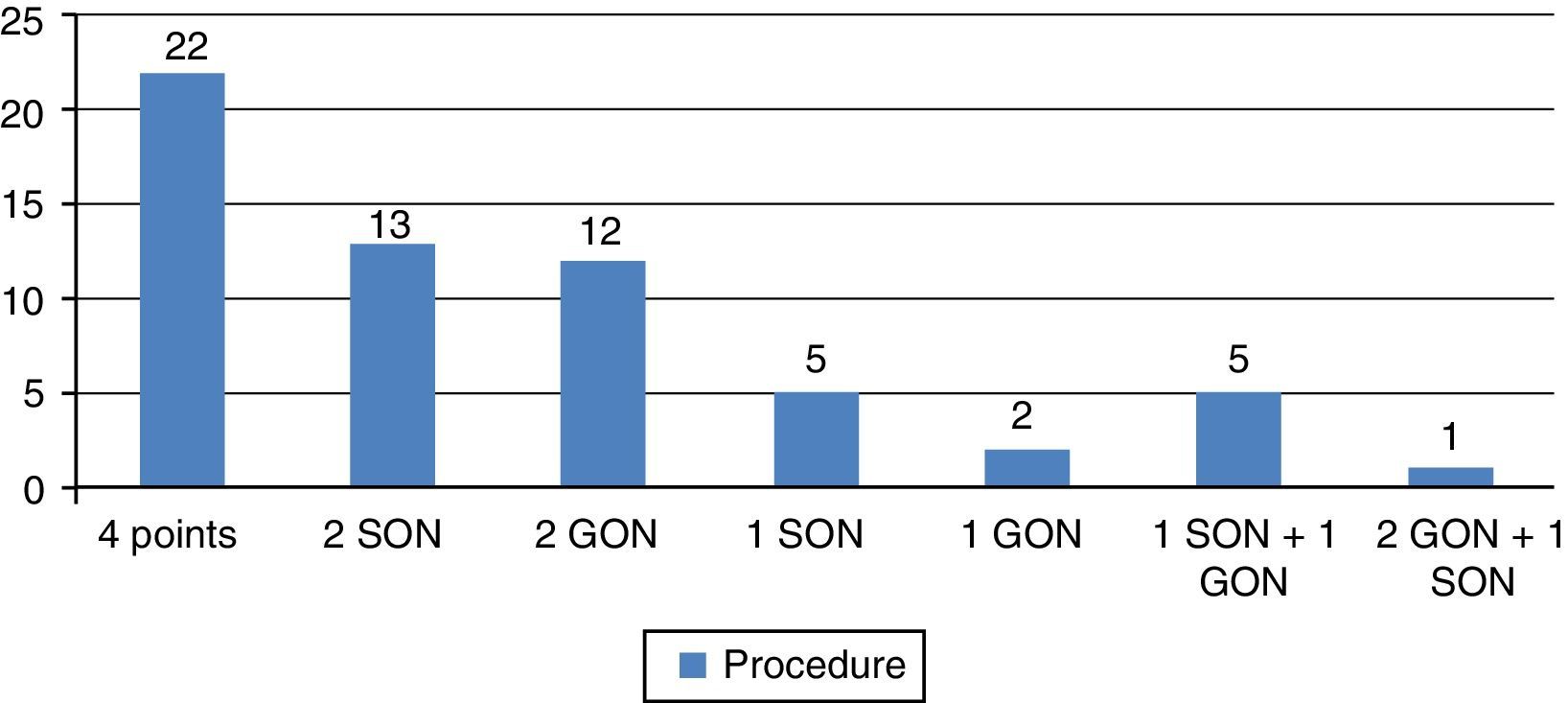
ResultsAnaesthetic blockade was performed in 60 patients (52 females, 8 males; mean age 40.6±12.4 years, range 19-76). The most common procedure was blockade of GON and SON on both sides. Complete response lasting at least 2 weeks was recorded in 23 patients (38.3%), with partial response in 24 patients (40%), and no response in 13 (21.7%). In the group presenting complete response, age and length of history of migraine were significantly lower. No severe side effects were detected. Response time ranged from 2 weeks to 3 months.
ConclusionsPericranial nerves blockade using tenderness to palpation as an inclusion criterion is safe and potentially effective as prophylactic treatment for migraine. The best responses in our series were observed in younger patients with shorter histories of migraine.
El bloqueo anestésico de nervios pericraneales es utilizado con frecuencia en el tratamiento de diferentes cefaleas. No hay evidencia acerca de su indicación en pacientes migrañosos. Pretendemos evaluar su eficacia como tratamiento preventivo de migraña con criterios determinados.
MétodosEntre enero del 2009 y mayo del 2013 se ofreció este tratamiento a migrañosos con fracaso o intolerancia de fármacos preventivos. Seleccionamos a aquellos con sensibilidad a la palpación en al menos un nervio supraorbitario u occipital mayor. A los 3 meses, consideramos la respuesta completa (sin dolor), parcial (reducción al menos de un 50% en severidad y/o frecuencia de episodios) o ausente.
ResultadosSe practicó un bloqueo anestésico en 60 pacientes (52 mujeres, 8 varones, edad media±desviación estándar: 40,6±12,4 años, rango 19-76). El procedimiento más habitual fue el bloqueo de ambos nervios occipitales y supraorbitarios. Hubo respuesta completa de al menos 2 semanas en 23 (38,3%), parcial en 24 (40%) y ausente en 13 (21,7%). En el grupo con respuesta completa, la edad y el tiempo de evolución de la migraña eran significativamente inferiores. Sin efectos adversos significativos. Tiempo de respuesta entre 2 semanas y 3 meses.
ConclusionesEl bloqueo anestésico de nervios pericraneales utilizando la sensibilidad a la palpación como criterio de selección es un procedimiento seguro y potencialmente eficaz como tratamiento preventivo de migraña. Las mayores respuestas en nuestra serie se observan en pacientes jóvenes con menos tiempo de evolución de la migraña.
Migraine is a primary headache with the well-defined clinical characteristics described in the International Classification of Headache Disorders, third edition (ICHD-3).1 It affects 11.5% of the adult population worldwide2 and is responsible for 1.3% of all years of life lost due to disability.3 Migraine generates substantial costs for society, especially those resulting from reduced productivity and work absenteeism; the annual cost per person is estimated at €1200.4 This cost is 1.5 to 3.6 times greater for chronic migraine than in episodic migraine.5 It therefore seems obvious that controlling symptoms may reduce the associated disability and the social consequences of migraine.
Unfortunately, current therapeutic tools (meaning lifestyle and dietary recommendations, symptomatic treatment, and preventive treatment) fail to achieve satisfactory pain management in some patients. In the past years, there have been many advances in the study, development, and standardisation of new treatment options for patients with refractory migraine. Examples include the onabotulinum toxin A injection, which has proven to be effective as a preventive treatment for chronic migraine in the PREEMPT study,6 several neurostimulation systems, and local anaesthetic nerve block.
Pericranial nerve block, especially occipital nerve block, is increasingly used for treating different types of primary and secondary headaches and neuralgia. However, available evidence does not conclusively show this treatment to be effective for migraine, although several descriptive studies and expert consensus statements support it.
Our purpose is to evaluate the effectiveness and safety of anaesthetic blockade of pericranial nerves as a preventive treatment for migraine by applying a specific protocol for selecting both patients and injection sites.
Patients and methodsPatients were recruited prospectively from the headache unit at a tertiary hospital between January 2009 and March 2013. Migraine was diagnosed according to the criteria listed in the second edition of the ICHD7; chronic migraine and medication-overuse headache were diagnosed based on the revised version published in 2006.8 We selected consecutive patients who had received preventive treatment (at least one beta-blocker or a neuromodulator) without experiencing relief or who had shown poor tolerance of that treatment. We examined the exit points of the greater occipital nerves (GON) and supraorbital nerves (SON) in all patients. To be included in the study, patients had to show sensitivity to pressure at the exit point of at least one of the 4 nerves; anaesthetic block was performed on sensitive nerves only.
All patients with migraine in our unit were instructed to complete a migraine diary to record the number of days with pain, pain intensity, days when they needed symptomatic treatment (including triptans), and whether they had to visit the emergency department to manage an episode. We recorded the variables age, sex, age at migraine onset, and disease progression in years for each patient. We determined whether patients had episodic or chronic migraine, and whether they met the criteria for medication-overuse headache. We also recorded the type of preventive treatment used when the first injection was performed (beta-blocker, neuromodulator, antidepressant, or calcium channel blocker).
Sensitivity to pressure was defined as pain resulting from pressing on the exit point of the nerves being assessed. The local anaesthetic consisted of a 1:1 mixture of bupivacaine 0.5% and mepivacaine 2%.
The GON were assessed by pressing on the occipital region, above the imaginary line that joins the mastoid process and the occipital protuberance. We injected a dose of 2mL into the point showing sensitivity to pressure along the imaginary line; this point was usually located between the middle third and the proximal third of this line. GON injections were performed with at least 2 changes of direction to cover an area of about 60°, and we subsequently compressed the area to aid in drug infiltration.
For the SON, we palpated the area near the supraorbital notch. We injected a dose of 0.5mL by introducing the needle into the subcutaneous tissue near the supraorbital notch; the needle was directed towards the forehead at an angle of 45°. Again, the area was compressed after the injection. No changes in preventive treatment were made at the time of the procedure.
Three months after the procedure, patients were followed up at the headache unit to assess clinical response. Complete response was achieved when the patient experienced no pain for at least 2 weeks; a reduction of at least 50% in the number of days with pain or a reduction in pain intensity for a minimum of 2 weeks were considered partial responses.
When no response was achieved after the first intervention, patients were given the option of repeating the procedure. The patients showing partial or complete response after the first anaesthetic blockade underwent additional interventions according to their clinical situation and own preferences.
We analysed whether age, time of disease progression, episodic vs chronic presentation, or even medication overuse had an impact on patients’ response to the first anaesthetic blockade. We used the t test or the chi-square test according to the data distribution; statistical analysis was performed with SPSS software version 20.0.
ResultsDuring the study period (4 years and 3 months), we included a total of 60 patients (52 women, 8 men) with a mean age±SD of 40.6±12.3 years (range, 19-76). Mean time from migraine onset was 16.1±11.5 years (range, 1-44). Forty-three patients (71.7%) had chronic migraine and 24 of these (55.8%) also demonstrated symptomatic medication overuse. During the month before the anaesthetic blockade, the number of days with pain in our sample was 19.6±10.6 (range, 3-30); symptomatic treatment was necessary a mean of 14.3±9.2 days (range, 0-30), and triptans, 2.8±4.1 days (range, 0-20). Migraine severity was measured with the Headache Impact Test (HIT-6). At the time of the anaesthetic nerve block, migraine severity was 65.8±6.5 (range, 52-76); in 86.6% of the patients it was at least moderate (HIT-6 score>55).
All patients had received at least one type of preventive treatment dosed appropriately for at least 3 months, except in cases of intolerance. This treatment included at least one beta-blocker or a neuromodulator. At the time of the anaesthetic blockade, 44 patients (73.3%) were receiving at least one preventive drug: 33 (55%) neuromodulators, 14 (23.3%) beta-blockers, 7 (11.6%) calcium channel blockers, and 6 (10%) antidepressants.
The most frequently used technique was blockade of both occipital and supraorbital nerves. Fig. 1 summarises the procedures.
Twenty-three patients (38.3%) showed complete response for at least 15 days, 24 patients (40%) displayed partial response, and 13 patients (21.7%) showed no response. Response lasted up to 3 months in some cases.
No adverse effects were reported besides occasional vasovagal episodes that resolved with rest, and discomfort near the injection sites that resolved in a few hours.
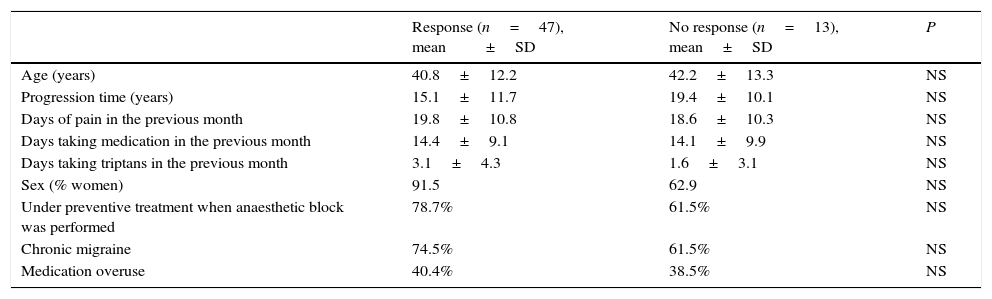
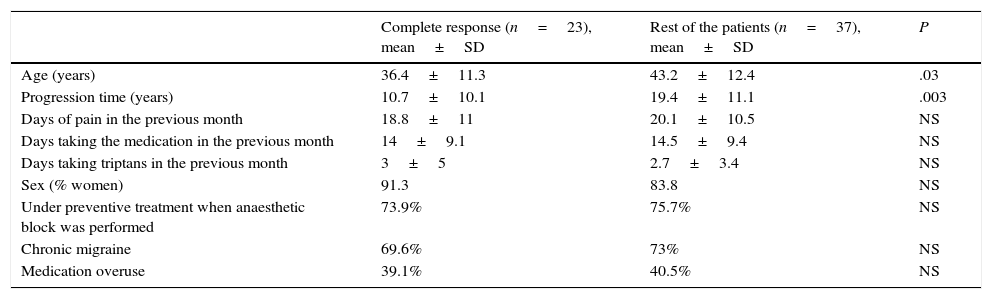
First of all, we compared the clinical and demographic variables between the patients with response (either complete or partial) and those showing no response. No significant differences were detected for any of these variables (Table 1). In contrast, age and time of migraine progression were significantly lower in the patients with complete response than in the rest of the patients (Table 2).
Comparison between the group showing response to anaesthetic block and the group showing no response.
| Response (n=47), mean±SD | No response (n=13), mean±SD | P | |
|---|---|---|---|
| Age (years) | 40.8±12.2 | 42.2±13.3 | NS |
| Progression time (years) | 15.1±11.7 | 19.4±10.1 | NS |
| Days of pain in the previous month | 19.8±10.8 | 18.6±10.3 | NS |
| Days taking medication in the previous month | 14.4±9.1 | 14.1±9.9 | NS |
| Days taking triptans in the previous month | 3.1±4.3 | 1.6±3.1 | NS |
| Sex (% women) | 91.5 | 62.9 | NS |
| Under preventive treatment when anaesthetic block was performed | 78.7% | 61.5% | NS |
| Chronic migraine | 74.5% | 61.5% | NS |
| Medication overuse | 40.4% | 38.5% | NS |
Group showing complete response to anaesthetic block vs rest of the patients.
| Complete response (n=23), mean±SD | Rest of the patients (n=37), mean±SD | P | |
|---|---|---|---|
| Age (years) | 36.4±11.3 | 43.2±12.4 | .03 |
| Progression time (years) | 10.7±10.1 | 19.4±11.1 | .003 |
| Days of pain in the previous month | 18.8±11 | 20.1±10.5 | NS |
| Days taking the medication in the previous month | 14±9.1 | 14.5±9.4 | NS |
| Days taking triptans in the previous month | 3±5 | 2.7±3.4 | NS |
| Sex (% women) | 91.3 | 83.8 | NS |
| Under preventive treatment when anaesthetic block was performed | 73.9% | 75.7% | NS |
| Chronic migraine | 69.6% | 73% | NS |
| Medication overuse | 39.1% | 40.5% | NS |
In addition to the results from the first anaesthetic blockade, we have continued to analyse results from a total of 128 procedures conducted in our 60 patients during the study period. Complete response was achieved in 44 procedures (34.4%), partial response in 59 (46.1%), and no response in 25 (19.5%).
Twenty-seven patients (45%) underwent a single anaesthetic blockade, 16 (26.7%) underwent 2 interventions, and the remaining patients had 3 to 8 interventions, with a global mean of 2.12 nerve blocks per patient. Three of the 13 patients who did not respond to the first procedure, showed a response in subsequent interventions. Likewise, several patients showing response in the first procedure did not respond to subsequent anaesthetic blockades.
DiscussionUse of pericranial anaesthetic nerve block for headache patients is on the rise in clinical practice. However, evidence that it is effective is scarce and usage patterns vary greatly among professionals. Expert groups are currently working to reach a consensus on the best techniques and indications based on the data available to date. Some studies support peripheral nerve block as an effective and safe technique. This intervention should therefore be considered as treatment for different types of headache.9
Local anaesthetics reversibly inhibit voltage-gated sodium channels. When used at low doses, these drugs act selectively on sensory nerve fibres. However, their action mechanism as migraine treatment is yet to be fully understood. Pain in migraine and other primary headaches seems to be associated with the activation of nociceptors in the dura mater and intracranial blood vessels, which are innervated by fibres from the first branch of the trigeminal nerve. Several studies support the convergence of trigeminal afferents with the upper cervical roots at the level of the trigeminal nucleus caudalis, in the brainstem.10 Inhibition of some nociceptive fibres of the trigeminocervical complex (for example, anaesthetic block of cervical fibres due to infiltration at the level of the occipital nerve [C2]) is likely to inhibit the whole system, affecting sensory areas of other nerves.11 It is not clearly understood how the effects of the drug only last a few hours whereas its benefits may last up to several months. One explanation might be a break in the pain cycle that is thought to be present in central sensitisation in migraine.12 In our study, we decided to use an anaesthetic with an average duration of action (mepivacaine) combined with an anaesthetic with more long-lasting effects (bupivacaine).
As stated previously, anaesthetic nerve block has been used in many patients with drug-resistant headache. This type of intervention has shown its usefulness in association with corticosteroids in patients with cluster headache: in a study including 14 patients with chronic (CCH) or episodic cluster headache (ECH), 64% showed partial or complete response to injection of lidocaine plus triamcinolone into the GON for ipsilateral pain.13 Similar results were reported in another recently published open study: 57% of 83 patients with CCH responded to lidocaine plus methylprednisolone.14 Two clinical trials for this procedure have been published to date: the first of these15 compared the effects of lidocaine plus corticosteroids (n=13) to those of lidocaine plus a placebo (n=10) in 23 patients (16 with ECH, 7 with CCH); after one week, complete response was achieved by 85% of the patients in the corticosteroid group, but none of the patients in the placebo group. The second clinical trial16 included 43 patients (28 with ECH, 15 CCH) who were administered either cortivazol (n=21) or a placebo (n=22); the cortivazol group displayed a sharper decrease in the number of daily episodes during the first 2 weeks.
Anaesthetic nerve blockade may also be useful in patients with hemicrania continua (HC) and poor tolerance to indometacin. In a previous study,17 we performed anaesthetic blockade on 13 patients with HC who were intolerant to indometacin by injecting a mixture of bupivacaine and mepivacaine into the GON and SON ipsilateral to pain (plus a trochlear injection of triamcinolone in cases of trochlear pain). Twelve of our patients (92.3%) showed at least a partial response to treatment.
One of the diagnostic criteria for occipital neuralgia (ON) is pain relief after local anaesthetic block of the affected nerve.1 According to one ON study, corticosteroids successfully controlled pain for at least one week in 90% of patient population (at least one month in 30%).18 Another study of ON reported a good response to local anaesthetics for more than one month in 36% of its 23 participants.19 Our research group performed anaesthetic nerve blockade with a mixture of bupivacaine and mepivacaine in 14 patients diagnosed with ON, all of whom achieved a complete response for 2 to 6 months.20 Anaesthetic blockade has been proved effective for cervicogenic headache, post-traumatic headache, the different types of headaches previously known as daily chronic headache, and such other neuralgias as supraorbital neuralgia or auriculotemporal neuralgia.9,12,21
But returning to our topic, this procedure has been proved effective for acute-phase migraine. Blocking the GON with lidocaine has been reported to halt migraine episodes in 88% of one patient group22; 82% of another patient population experienced relief 15minutes after GON and SON block with adrenaline and lidocaine.23 It has also been found to reduce pain in 90% of a patient group 20minutes after lidocaine injection into the GON,24 and decreased pain intensity and associated allodynia and photophobia were achieved only 5minutes after injecting lidocaine and bupivacaine.25
However, as in our case, other studies have focused on evaluating the benefits of anaesthetic blockade of pericranial nerves as a preventive treatment for migraine. In 1992, Gawel and Rothbart published results from a retrospective study on patients diagnosed with either migraine (n=97) or post-traumatic headache with clinical features of migraine (n=87) and who showed no response to standard medical treatment. These patients received injections of lidocaine plus methylprednisolone in both GON; 53.6% of the patients with migraine and 72.4% of those with post-traumatic headache reported less pain at the 6-month follow-up visit.26 A 1996 study including 27 patients with refractory migraine assessed the effectiveness of bupivacaine injection at the pressure-sensitive emergence points of both GON and SON. Patients underwent 5 to 10 sessions on alternate days, and their Total Pain Index decreased (from 347.1 at baseline to 106.8 at one month and 60.9 at 6 months; this index expresses the number of hours of pain per month and pain intensity). They also experienced decreases in number of attacks per month (from 12.8 at baseline to 7.1 at one month and 5.1 at 6 months), and in monthly analgesic consumption (from 12.4 at baseline to 5.6 at one month and 3.8 at 6 months).27 In addition to occipital nerves, supraorbital and infraorbital nerves (ION) have also been targeted for migraine treatment. According to a recent study of 26 patients with migraine, lidocaine infiltration in both SON and ION, given in 3 doses spaced 3 days apart, substantially reduced the number of attacks per month (from 9.9 to 2), pain intensity (from 9 to 3.5), and disability according to the MIDAS scale (from 3.2 to 1.4) at 6 months.28 In 2008, a study of 37 patients with what was then known as transformed migraine compared the use of lidocaine plus bupivacaine in combination with either triamcinolone or a placebo in both GON, as well as the effects of an injection of the same mixture into different trigger points of both trapezius muscles. Both groups displayed similar reductions in pain intensity 20minutes after injection. Severity of photophobia, neck pain, and to a lesser extent phonophobia decreased similarly in the 2 groups. There were no statistically significant differences in headache-free time, duration of response, or analgesic use between the placebo and corticosteroid groups.29 The only double-blind placebo-controlled clinical trial that has been conducted to assess anaesthetic block as a preventive treatment for migraine was published in 2001. In this crossover study, participants received 2 infiltrations in the GON bilaterally, administered one month apart, of either bupivacaine 0.5% or a saline solution. Of the 63 patients included in the study, only 37 were included in the final analysis. No statistically significant differences were found in either the number or the duration of episodes. It should be noted that this study included patients with low monthly frequencies of migraines, which may have minimised the beneficial effects of anaesthetic block.30
Comparing our data to those from the literature is extremely difficult. First of all, target nerves are not the same: options included SON and ION,28 GON bilaterally,26,29 and GON and/or SON when sensitive to pressure.27 We chose sensitivity to pressure as the selection criterion, and on this basis, the technique we performed the most was blockade of all 4 nerves. This may represent the technique to be standardised in the future. At present, the small sample size of the studies does not allow us to analyse each of the studied nerves individually. Previous studies have shown that identifying sensitivity to pressure at the exit point of the GON may predict a better response to anaesthetic infiltration in that nerve.31
Another factor making comparison between studies difficult is the different local anaesthetics used, although they are supposed to have similar effects. Lidocaine is the second most widely-used drug for migraine23–25,28,31 after bupivacaine27,32; some studies have used a combination of these 2 drugs.25 The comparison of these studies yields no data favouring one drug over another. We chose mepivacaine and bupivacaine to combine a fast-acting anaesthetic with another with a longer half-life. However, this option is open to debate. In fact, we have been administering lidocaine 1% to our patients since the end of the recruitment phase.
Some years ago, corticosteroids were thought to maximise the benefits of anaesthetics and were therefore used in combination with the latter as a prophylactic26 or symptomatic treatment24,31 in patients with migraine. However, a subsequent placebo-controlled clinical trial showed that combined treatment with corticosteroids is not superior to anaesthetic treatment alone.29 Today, corticosteroids are not recommended for patients with migraine except in cases where local anaesthetics are contraindicated.22 Repeated corticosteroid use can cause trophic changes that may be tolerated in the occipital region, but corticosteroid use is not recommended in the facial region. Since our study design included the possibility of blocking the SON, we decided not to use these drugs.
It is very difficult to exclude the placebo effect in an open study of the effectiveness of an instrumental procedure. Nevertheless, we find it encouraging that nearly 80% of the treated patients experienced a decrease of at least 50% in days with pain for long periods whereas preventive treatment showed no effects.
Except for pericranial nerve sensitivity to pressure (an inclusion criterion in our study), no other clinical or demographic variables have been shown to predict response to anaesthetic nerve block in previous studies. More specifically, sensation of anaesthesia after injection in the sensory territory of the GON,31 medication overuse,31 and presence of cervical or occipital pain26 were not shown to be predictors of good response. In our study, the patients experiencing complete response to nerve block were younger and had shorter histories of migraine. The degree of central sensitisation in young patients and those with a shorter history of the disease may be different, less established, and therefore easier to alter than in patients with a greater disease burden.
Previous studies and our own experience suggest that anaesthetic blockade of pericranial nerves is a safe technique when performed by expert doctors. We have completed over 600 interventions for different indications in our headache unit since January 2009 without observing any significant adverse effects. Nonetheless, we should always take the necessary precautions22 and never forget that this procedure is strictly contraindicated in patients with a history of posterior fossa craniotomy due to the risk of CNS depression.33 The most frequently described complications are vasovagal episodes,31,34 dizziness, and pain at the site of the injection.31 Other local secondary effects, including cutaneous atrophy, hyperpigmentation, and alopecia, have only been linked to infiltration with corticosteroids.35 The technique itself is associated with a number a complications that should be considered and prevented as follows: adopting basic aseptic measures to prevent local infections that may result from disruption of the skin barrier, using a diluted mixture and minimising the number of injections in elderly patients (in whom treatment may alter blood pressure) or those patients with a history of vasovagal syncope (increasing the resting time in these patients is also important), and increasing compression time (5-10minutes) in patients taking anticoagulant or antiplatelet drugs.
Our study shows pericranial nerve block to be a safe and effective preventive treatment for migraine. However, it does have a number of limitations. Since it is an open study including patients with different types of migraine, we cannot draw definitive conclusions on the use of this technique. In addition, we could not establish criteria for predicting response to anaesthetic block due to the small sample size. However, in a standard clinical situation, anaesthetic blockade of pericranial nerves may be an inexpensive and safe option for managing patients with refractory migraine.
In view of the heterogeneous methods of using pericranial anaesthetic blockade to prevent migraine, and based on expert recommendations,9 we call for further placebo-controlled multicentre clinical trials, including different types of migraine, to gather evidence sufficient to list this technique as a potential means of migraine prevention.
In conclusion, pericranial nerve block was beneficial as a preventive treatment for migraine in 81.7% of a group of patients with a history of preventive drug intolerance or failure to respond and who were sensitive to pressure at the exit points of pericranial nerves. None of our patients experienced substantial secondary effects. In our experience, anaesthetic blockade of pericranial nerves using sensitivity to pressure as a selection criterion is safe, affordable, and effective as a preventive treatment for migraine, and may even be used as a second-line treatment.
FundingThis study has received no funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Ruiz Piñero M, Mulero Carrillo P, Pedraza Hueso MI, de la Cruz Rodríguez C, López Mesonero L, Guerrero Peral AL. Bloqueo anestésico de nervios pericraneales como tratamiento preventivo de migraña: experiencia en una serie de 60 pacientes. Neurología. 2016;31:445–451.