Neurofibromatosis type 1 (NF1) is frequently associated with neurological disorders unrelated to neurofibromas, including sleep disorders.
ObjectivesThis article reviews the prevalence of sleep disorders in patients with NF1, compares rates to data reported in the literature, and analyses the relationship between cognitive disorder and attention deficit hyperactivity disorder (ADHD) in these patients.
Material and methodsComparative retrospective study reviewing data collected between January 2010 and January 2012 from patients diagnosed with NF1 in a tertiary hospital.
ResultsWe included 95 paediatric patients with NF1 who completed the Bruni Sleep Disturbance Scale in Children (SDSC). The overall prevalence of sleep disorders was 6.3%, which was lower than in the general paediatric population. Patients with NF1 and ADHD had a higher prevalence of sleep onset and maintenance disorders (18% vs 6.3%), sleep-wake transition disorders (12.5% vs 6.3%), and daytime sleepiness (12.5% vs 7.9%); differences were not statistically significant. A statistically significant difference was found in the subdomain of nocturnal hyperhidrosis (21.9% vs 6.3%, P<.05). Patients with NF1 and IQ<85 showed higher prevalence rates of daytime sleepiness (20% vs 6.7%) and of sleep hyperhidrosis (11% vs 0%).
ConclusionsThe prevalence of sleep disorders in our cohort of patients with NF1 was no higher than in the general paediatric population, although some of these disorders are more common in cases with cognitive disorders or ADHD.
La neurofibromatosis tipo 1 (NF1) asocia frecuentemente alteraciones neurológicas no relacionadas con neurofibromas, entre las que se encuentran los trastornos del sueño.
ObjetivosRevisión de la prevalencia de trastornos de sueño en pacientes con NF1 y compararla con los datos descritos en la literatura, así como analizar la relación con el trastorno cognitivo y el trastorno por déficit de atención e hiperactividad (TDAH) en estos pacientes.
Material y métodosEstudio comparativo, retrospectivo, mediante la revisión de los datos recogidos entre enero de 2010 y enero de 2012 de pacientes diagnosticados de NF1 en un hospital de tercer nivel.
ResultadosSe incluyeron 95 pacientes con NF1 pediátricos que respondieron correctamente a la Escala de alteraciones del sueño en la infancia de Bruni, encontrando una prevalencia de trastorno global del sueño del 6,3%, inferior al de la población pediátrica general. Aquellos pacientes con NF1 y TDAH presentaron mayor prevalencia de trastorno de inicio-mantenimiento del sueño (18 vs 6,3%), de transición sueño-vigilia (12,5 vs 6,3%) y somnolencia diurna (12,5 vs 7,9%) sin alcanzar significación estadística, sí encontrándose diferencia estadísticamente significativa en la subescala de hiperhidrosis nocturna (21,9 vs 6,3%; p<0,05). Los pacientes con NF1 y cociente intelectual<85 presentaron mayor prevalencia de somnolencia diurna (20 vs 6,7%) y mayor hiperhidrosis nocturna (11 vs 0%).
ConclusionesEn nuestra cohorte de pacientes con NF1 no hemos encontrado aumento de la prevalencia de trastornos de sueño con respecto a la población pediátrica general, aunque algunos de estos trastornos son más frecuentes en caso de alteraciones cognitivas o TDAH.
Neurofibromatosis type 1 (NF1), also known as von Recklinghausen disease, is a progressive multisystem genetic disorder predominantly affecting the skin and the central nervous system. With an approximate incidence rate of 1 case per 2500 to 3500 live births,1 NF1 is considered one of the most frequent autosomal dominant genetic conditions. While it shows complete penetrance, its clinical phenotype is variable and unpredictable.1 Approximately 50% of patients with NF1 present mild forms of the disease, and about a third develop severe complications arising when plexiform neurofibromas affect organs; these neurofibromas present a high risk of malignant transformation.2 NF1 is frequently associated with neurological and vascular changes which are unrelated to neurofibromas but whose aetiology remains unclear. Some of the neurological diseases described in patients with NF1 include learning disorders, sleep disorders, epilepsy, macrocephaly, and neuroimaging abnormalities.2
Sleep is very important as it occupies about one-third of a person's life, and while sleep disorders are frequent during childhood, they may go unnoticed.
In view of the low number of studies reporting an increased incidence of sleep disorders in patients with NF1, we decided to analyse the prevalence of sleep disorders in a cohort of patients with NF1 and compare our results to data provided in the literature. Our study also analyses co-presence of mental retardation and attention deficit hyperactivity disorder (ADHD) in these patients.
Materials and methodsWe conducted a retrospective cross-sectional comparative study by reviewing the data gathered between January 2010 and January 2012 from patients diagnosed with NF1 in a paediatric neurology department at a tertiary hospital. Data were collected using a standardised clinical interview, a psychometric assessment, and sleep questionnaires that were completed by the patients’ parents.
Sleep disorders were assessed with the Sleep Disturbance Scale for Children (SDSC),3 which consists of 27 items scored using a Likert-type scale. The SDSC classifies sleep disorders in six categories: disorders of initiating and maintaining sleep, sleep breathing disorders, disorders of arousal/nightmares, sleep-wake transition disorders, disorders of excessive daytime somnolence, and sleep hyperhidrosis. The SDSC evaluates the preceding 6 months and has been validated in children aged 6 to 15 years. Subsequent studies also support use of this scale in preschool-aged children.4 The cut-off point for global sleep disorder is 39, with a sensitivity of 89% and a specificity of 74%. Additionally, this scale establishes normal ranges for the subscales of specific sleep disorders.
The NF1 database lists a total of 215 patients, 102 of whom had been assessed with the SDSC. Seven patients were excluded from the study: 2 had reached the age of 18 and the remaining 5 had filled in the questionnaire incompletely or incorrectly. A total of 95 patients were included in the study. We analysed the following variables: age, sex, IQ scores, presence and subtype of ADHD, the presence of other neurocognitive disorders or other associated diseases, scores on the SDSC (both global sleep disorder and the subscales for specific sleep disorders), and whether those scores were indicative of a sleep disorder.
For all cases, neurofibromatosis was diagnosed according to consensus-based clinical criteria published by the National Institutes of Health.5
ADHD was diagnosed following the clinical criteria listed in the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV).
In some patients, the neuropsychological and IQ assessments were performed as part of a protocol. IQ was not evaluated in children showing good academic performance, as these patients were not suspected to have below-average scores.
Within the group with NF1, we compared global prevalence data for sleep disorders and published data on sleep disorders in paediatric patients. We also compared the groups of NF1 children with and without ADHD, and NF1 patients with normal IQ scores, to those with borderline intellectual functioning or intellectual disability.
ResultsThe study included 95 patients with NF1 whose information had been recorded in the database; all of them were younger than 18, and they all had completed the SDSC correctly.
The patients’ ages ranged from 3 years and 10 months to 17 years and 10 months; 53.5% were boys and 46.5% were girls. Regarding IQ, 79% had normal scores, 14% had borderline intellectual functioning, 2 patients presented mild intellectual disability, and another patient had moderate intellectual disability. A total of 43 patients underwent IQ testing; the mean score was 92.58 (range, 51-128). A total of 34% of patients were diagnosed with ADHD: 34.4% presented the inattentive subtype, 50% the combined subtype, and the ADHD subtype was unknown in the remaining patients. Additionally, 15.8% of the patients presented a non-specified learning disorder, 2 patients had dyscalculia, 5 had language disorders, 2 had psychomotor retardation, 1 had non-verbal learning disabilities, and 1 had a behavioural disorder.
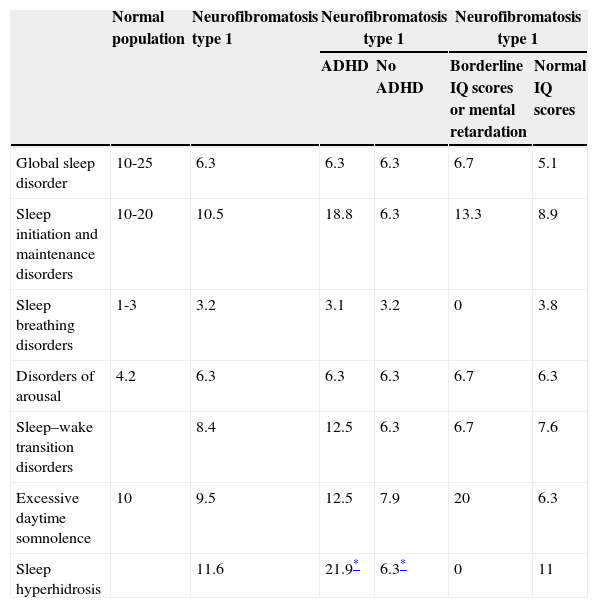
The mean score for sleep disorders was 17 points (range, 2-83). Six patients scored higher than 39 on the SDSC; this score is compatible with the presence of global sleep disorder. This corresponds to a prevalence of 6.3%, which is lower than the prevalence estimated for the general paediatric population (15%-37%)6 and agrees with prior data from children with NF1. A breakdown by sleep disorder types revealed 10 patients (10.5%) with disorders of initiating and maintaining sleep, 3 (3.2%) exhibiting sleep breathing disorders, 6 (6.3%) with disorders of arousal/nightmares, 8 (8.4%) with sleep-wake transition disorders, 9 (9.5%) presenting disorders of excessive daytime somnolence, and 11 (11.6%) with sleep hyperhidrosis. These prevalence rates are similar to those reported in the general population (Table 1).6
Prevalence rate (%) of sleep disorders by population subgroups.
| Normal population | Neurofibromatosis type 1 | Neurofibromatosis type 1 | Neurofibromatosis type 1 | |||
|---|---|---|---|---|---|---|
| ADHD | No ADHD | Borderline IQ scores or mental retardation | Normal IQ scores | |||
| Global sleep disorder | 10-25 | 6.3 | 6.3 | 6.3 | 6.7 | 5.1 |
| Sleep initiation and maintenance disorders | 10-20 | 10.5 | 18.8 | 6.3 | 13.3 | 8.9 |
| Sleep breathing disorders | 1-3 | 3.2 | 3.1 | 3.2 | 0 | 3.8 |
| Disorders of arousal | 4.2 | 6.3 | 6.3 | 6.3 | 6.7 | 6.3 |
| Sleep–wake transition disorders | 8.4 | 12.5 | 6.3 | 6.7 | 7.6 | |
| Excessive daytime somnolence | 10 | 9.5 | 12.5 | 7.9 | 20 | 6.3 |
| Sleep hyperhidrosis | 11.6 | 21.9* | 6.3* | 0 | 11 | |
The comparative analysis of sleep disorders in children with NF1 with and without ADHD found no significant differences in terms of prevalence of global sleep disorder (6.3% for both groups). We did find, however, a statistically significant difference in the prevalence of sleep hyperhidrosis: 21.9% of the children with NF1 and ADHD vs 6.3% of children without ADHD (P<.05). We also found differences in the prevalence of disorders of initiating and maintaining sleep (18% of the children with ADHD vs 6.3% without ADHD), sleep-wake transition disorders (12.5% vs 6.3%), and excessive daytime somnolence (12.5% vs 7.9%), but these differences were statistically non-significant.
The prevalence of global sleep disorder was 6.7% in the group of patients with NF1 and borderline intellectual functioning or mild intellectual disability, and 5.1% among patients with normal IQ scores. Regarding specific sleep disorders, differences were only found for excessive daytime somnolence, with a prevalence of 20% in patients with NF1 and borderline intellectual functioning or mild intellectual disability vs 6.7% in patients with normal IQ scores, and in sleep hyperhidrosis, with prevalence rates of 0% vs 11%, respectively. These differences were not statistically significant.
DiscussionSleep, which takes up about one-third of a person's life, alternates with periods of wakefulness. This sleep-wake cycle, or circadian rhythm, lasts about 24hours. The amount of sleep a person needs varies with age, ranging from 16 to 18hours in infants or neonates to 12 to 15hours in school and preschool-aged children.2
Sleep disorders, although very frequent during childhood, are usually underdiagnosed. Their consequences in paediatric patients are a source of anxiety and distress for parents and carers as well as for the children themselves.
Sleep disorders can be classified into difficulties falling asleep (dyssomnia), disorders of arousal (parasomnia), and excessive daytime somnolence. Difficulties falling asleep and disorders of arousal usually occur concomitantly. There are also other minor sleep disorders, such as sleep initiation and maintenance disorders, sleep breathing disorders, disorders of arousal, sleep-wake transition disorders, excessive daytime somnolence, and sleep hyperhidrosis; all of these are included in the SDSC.
The epidemiology of sleep disorders in paediatric patients has been examined by a number of studies with varying results for global prevalence: some series show a prevalence of 10%,7 while other series report prevalences of 25%8 or even 60.4%.9 These discrepancies result from the type of questionnaire used in the study and the patients’ ages.
Prevalence rates for sleep disorders also differ according to the disorder subtype. In some series, the most frequent sleep disorders are parasomnias during childhood and delayed sleep phase disorder in adolescents.10 Other series report a high prevalence of night terrors and sleepwalking.11
The connection between sleep disorders and neurological disorders in paediatric patients is complex and may be approached in a number of ways. Primary sleep disorders may cause symptoms similar to those associated with ADHD and disruptive behaviours. On the other hand, sleep disorders are more prevalent and may exacerbate the symptoms of other neurodevelopmental disorders such as autism spectrum disorders, cognitive disorders, and ADHD. Central nervous system alterations may affect a child's sleep architecture, especially the establishment of an appropriate sleep-wake cycle. Likewise, pharmacological treatments used in these patients may exacerbate and/or cause sleep disturbances.12
The purpose of our study was to analyse the presence of sleep disorders in a cohort of patients with NF1. The prevalence of global sleep disorder in our study (6.3%) was lower than that found in the general paediatric population. This result is in line with the prevalence rates reported by Johnson et al.13 in 2005 in a group of 64 paediatric patients with NF1, and by Leschziner et al.14 in 114 adult patients with NF1. However, our data differ from the results reported by Licis et al.15 in a recently published article analysing sleep disorders in 129 patients with NF1 and 89 children without the disease. This study found a greater prevalence of sleep disorders among patients with NF1.
Our results for the different subscales are similar to those described in the literature: hyperhidrosis (11%), disorders of initiating and maintaining sleep (10%), excessive daytime somnolence (9%), sleep-wake transition disorders (8%), disorders of arousal (6%), and sleep breathing disorders (3%). We found no significant age or sex differences.
According to numerous studies, ADHD and sleep-wake transition disorders have common pathophysiological mechanisms, hence the importance of sleep research in patients with ADHD.16 No differences were found between prevalence of global sleep disorder for patients with NF1 and ADHD and for those without ADHD (6.3% for both groups). However, we did find statistically significant differences in the prevalence rate of sleep hyperhidrosis, which was 21.9% in patients with NF1 and ADHD, and 6.3% in children without ADHD (P<.05). Greater prevalence rates were also found for some sleep disorders in patients with ADHD: sleep initiation and maintenance disorders (18.8% vs 6.3%), sleep-wake transition disorders (12.5% vs 6.3%), and excessive daytime somnolence (12.5% vs 6.3%). These differences were non-significant.
Statistically significant differences in IQ scores were only detected in the subscale of excessive daytime somnolence; prevalence was 20% in patients with borderline intellectual functioning or mental retardation vs 6.7% in children with normal IQ scores. Non-significant differences were found in prevalence rates for sleep hyperhidrosis: 11% for patients with normal IQ scores vs 0% in patients with borderline intellectual functioning or mental retardation.
One limitation of our study is that we used a subjective scale (the SDSC), which may have skewed the results. Performing at-home polysomnography or actigraphy studies might have yielded more objective results for sleep and sleep disorders in our patients.
The prevalence of sleep disorders in our cohort of children with NF1, which is the largest cohort in any of the studies mentioned here, was similar to that in the general paediatric population. Some subtypes, however, were more frequent in patients with cognitive disorders or ADHD. Further systematic analyses of children with NF1 are necessary to evaluate the exact nature and aetiology of anomalies in these patients. This will help identify their needs so as to provide comprehensive care and carry out appropriate preventive actions.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Maraña Pérez AI, Duat Rodríguez A, Soto Insuga V, Domínguez Carral J, Puertas Martín V, González Gutiérrez Solana L. Prevalencia de trastornos del sueño en pacientes con neurofibromatosis tipo 1. Neurología. 2015;30:561–565.