Based on the 2 main frameworks for evaluating scientific evidence (SEC and GRADE) European cardiovascular prevention guidelines recommend interventions across all life stages using a combination of population-based and high-risk strategies with diet as the cornerstone of prevention. The evaluation of cardiovascular risk (CVR) incorporates HDL levels and psychosocial factors, a very high risk category, and the concept of age-risk. They also recommend cognitive-behavioural methods (e.g., motivational interviewing, psychological interventions) led by health professionals and with the participation of the patient's family, to counterbalance psychosocial stress and reduce CVR through the institution of positive habits such as a healthy diet, physical activity, smoking cessation, and adherence to treatment. Additionally, public health interventions—such as smoking ban in public areas or the elimination of trans fatty acids from the food chain—are also essential. Other innovations include abandoning antiplatelet therapy in primary prevention and the recommendation of maintaining blood pressure within the 130-139/80-85mmHg range in diabetic patients and individuals with high CVR. Finally, due to the significant impact on patient progress and medical costs, special emphasis is given to the low therapeutic adherence levels observed. In sum, improving cardiovascular prevention requires a true partnership among the political class, public administrations, scientific and professional associations, health foundations, consumer associations, patients and their families. Such partnership would promote population-based and individual strategies by taking advantage of the broad spectrum of scientific evidence available, from clinical trials to observational studies and mathematical models to evaluate population-based interventions, including cost-effectiveness analyses.
Las guías europeas de prevención cardiovascular contemplan 2 sistemas de evaluación de la evidencia (SEC y GRADE) y recomiendan combinar las estrategias poblacional y de alto riesgo, interviniendo en todas las etapas de la vida, con la dieta como piedra angular de la prevención. La valoración del riesgo cardiovascular (RCV) incorpora los niveles de HDL y los factores psicosociales, una categoría de muy alto riesgo y el concepto edad-riesgo. Se recomienda el uso de métodos cognitivo-conductuales (entrevista motivadora, intervenciones psicológicas), aplicados por profesionales sanitarios, con la participación de familiares de los pacientes, para contrarrestar el estrés psicosocial y reducir el RCV mediante dietas saludables, entrenamiento físico, abandono del tabaco y cumplimiento terapéutico. También se requieren medidas de salud pública, como la prohibición de fumar en lugares públicos o eliminar los ácidos grasos trans de la cadena alimentaria. Otras novedades consisten en desestimar el tratamiento antiagregante en prevención primaria y la recomendación de mantener la presión arterial dentro del rango 130-139/80-85mmHg en pacientes diabéticos o con RCV alto. Se destaca el bajo cumplimiento terapéutico observado, porque influye en el pronóstico de los pacientes y en los costes sanitarios. Para mejorar la prevención cardiovascular se precisa una verdadera alianza entre políticos, administraciones, asociaciones científicas y profesionales de la salud, fundaciones de salud, asociaciones de consumidores, pacientes y sus familias, que impulse la estrategia tanto poblacional como individual mediante el uso de toda la evidencia científica disponible, desde ensayos clínicos hasta estudios observacionales y modelos matemáticos para evaluar intervenciones a nivel poblacional, incluyendo análisis de coste-efectividad.
The European Guidelines on cardiovascular disease prevention in clinical practice (version 2012)1 stress that while numerous cardiovascular disease prevention guidelines have been published, few are based on high-quality evidence.2 Reading and applying such a large body of recommendations, some of which are contradictory, may not be possible for general practitioners whose schedules are typically overloaded. As a result, the European guidelines have gone largely unimplemented.3
The Spanish Interdisciplinary Cardiovascular Prevention Committee (CEIPC in Spanish), which consists of 15 medical societies and various government representatives, was created in 2000 to review scientific information on the prevention of cardiovascular disease (CVD), present a homogeneous approach for use in clinical practice by both doctors and nurses, and promote implementation of the guidelines. In its first decade, the committee published a Spanish-language adaptation of the 2003 version4 and the 2008 version5 of the European guidelines. As a result, doctors had access to a single consensus document supported by the Spanish Ministry of Health, rather than a long list of guidelines with dissimilar recommendations. Even so, a 2011 survey of a nationally representative sample of 1390 general practitioners showed that 16.4% of the respondents were not familiar with the CEIPC guidelines and 60% did not assess cardiovascular risks. The main obstacle they cited was limited time.6 Furthermore, the most common reason for scepticism about recommendations was the excessive number of published guidelines (cited by 70%). These observations point to a need to strengthen the CEIPC's activities aimed at increasing the circulation and implementation of the guidelines, and at editing them in easy-to-use formats (pocket guides, summary documents, and slides), hosting lectures and conferences, leading courses and workshops, and setting up cooperative networks.
In line with the above objectives, we present here a summarised, annotated adaptation of the European Guidelines for Cardiovascular Disease Prevention.1 We have preserved the document's original structure in 5 sections answering the following key questions: what is CVD prevention, why is it needed, who should benefit from it, how can CVD prevention be applied and when is the right moment to act, and where prevention programmes should be provided.
What is CVD prevention?The purpose of the European Guidelines is to provide up-to-date information on CVD prevention, meaning a coordinated array of actions intended to eradicate or minimise the impact of CVD on both the population and the individual level. The major change in the new guidelines is the introduction of combined systems for evaluating the quality of evidence (SEC and GRADE).7 These systems help make implementing guidelines easier and better adapted to clinical practice.8 SEC proposes various classes of recommendations (I, IIa, IIb, and III) whereas GRADE refers only to strong and weak classifications.7
Pharmacological treatments are more likely to be evaluated in clinical trials than are lifestyle modification interventions, whether designed for individuals or for entire populations. For that reason, the indiscriminate application of systems for evaluating evidence, which rank clinical trials above all other studies, may give rise to guidelines promoting excessive reliance on prescribing drugs rather than promoting smoking cessation, physical exercise, and healthy eating choices. We at the CEIPC address this issue, also mentioned in the guidelines, and emphasise the importance of population-wide interventions on lifestyle.
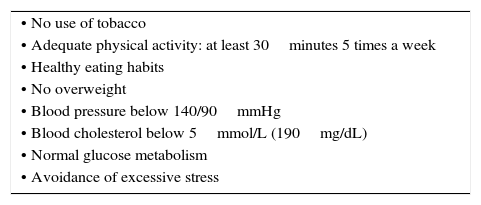
Implementing CVD prevention measures was included in the European political agenda in 2007, when the European Heart Health Charter was signed in the European Parliament.9 This public health declaration defines the parameters for maintaining an optimal level of health (Table 1) and it was adopted by most European Member States.
Profile of healthy or low CVR individuals (European Heart Health Charter).
| • No use of tobacco |
| • Adequate physical activity: at least 30minutes 5 times a week |
| • Healthy eating habits |
| • No overweight |
| • Blood pressure below 140/90mmHg |
| • Blood cholesterol below 5mmol/L (190mg/dL) |
| • Normal glucose metabolism |
| • Avoidance of excessive stress |
From O’Kelly and Ryden.9
The foundations of cardiovascular disease prevention, as established by the guidelines, can be expressed in 5 statements.
- 1.
CVD is the main cause of early death worldwide.
- 2.
Underlying atherosclerosis follows an insidious, gradual course over many years, and it is usually in an advanced stage when clinical symptoms appear.
- 3.
About 50% of all reductions in cardiovascular mortality are due to improving control over the main CVD risk factors.
- 4.
Much can still be done in the area of improving control over risk factors.
- 5.
A large body of evidence justifies implementing preventive interventions on both the individual and public health levels.
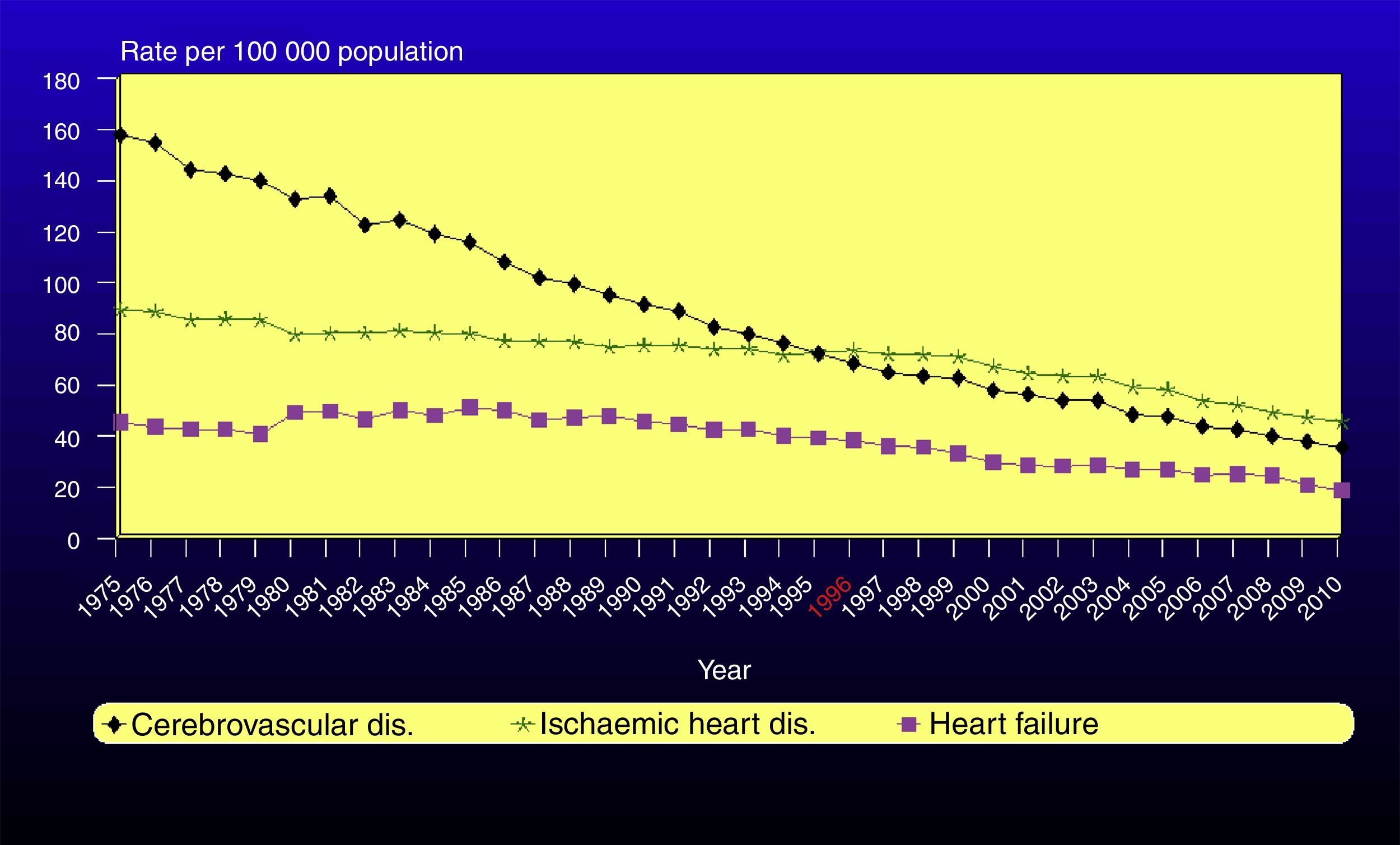
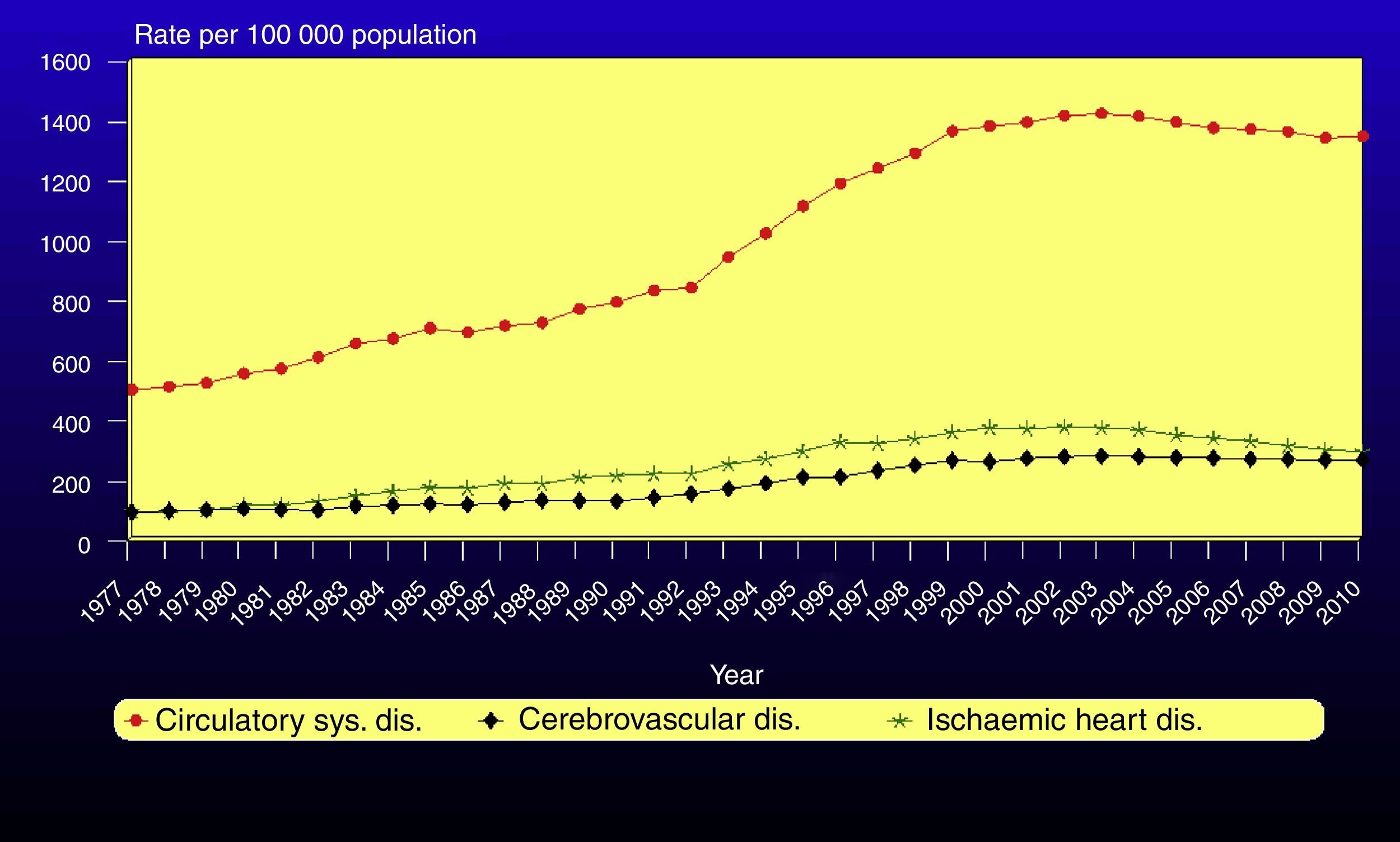
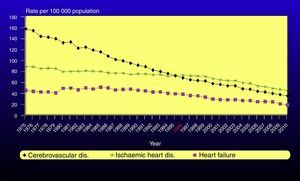
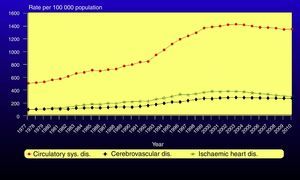
In Spain, where one in 3 deaths is caused by CVD, age-adjusted mortality rates for these diseases have been decreasing 3.1% yearly since 1975 (Fig. 1).10 Fifty per cent of this decrease is due to reducing such risk factors as high cholesterol, high blood pressure, and smoking.11 In contrast, rising obesity and diabetes, added to better survival rates among patients and overall population ageing, have increased the impact of CVD in Spain in absolute terms; hospital morbidity figures have tripled since 1980 (Fig. 2).10 Nevertheless, this tendency seems to have stabilised in the last 10 years.
The ENRICA study, carried out from 2008 to 2010 in a sample of 11957 individuals representing the Spanish population aged 18 and older, shows that population-wide control over the main cardiovascular risk factors has yet to be achieved. Only 22.7% of patients with arterial hypertension12 and 13.2% of those with high cholesterol13 have control over their conditions. This consideration, added to territorial variations in prevalence and the degree of control over risk factors,14 reveals that increasing preventive interventions could still be beneficial in Spain.
Early development of atherosclerosis could have to do with intrauterine conditions.15 Ideally, prevention of CVD would begin during fetal development and continue until the end of life. Nevertheless, preventive efforts focus on high-risk patients or those with CVD, at the expense of younger or elderly individuals and adults with moderate levels of risk. Early childhood is an especially important stage since it involves the development of dietary habits; once these habits are in place, they are highly resistant to change.16 In fact, most young patients exhibiting more extreme nutrient intakes (high or low), or those with other risk factors such as AHT, will remain in the same relative position for years.17,18
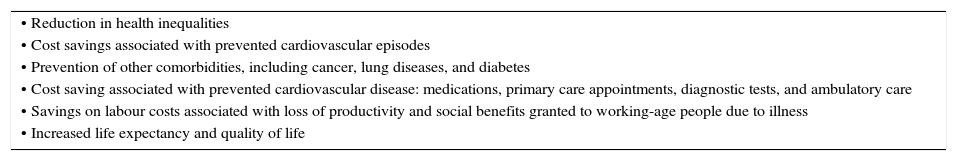
Prevention distinguishes between 2 strategies: population-wide and individual (high-risk). The first strategy aims at reducing CVD incidence by means of population-wide interventions intended to modify people's environments and living habits; an example would be prohibiting tobacco use in public places.19 The potential impact of these interventions is very high, given that most cardiovascular events occur in individuals with moderate risk levels. However, since better and more effective medical treatments have become more widespread, the consensus is that the best results are delivered by combining both population-wide and individual strategies. A NICE report estimates that the human and economic benefits of cardiovascular prevention initiatives are enormous and highlights many advantages of adopting a population-wide approach (Table 2).20
Benefits of a population-based approach to CVD prevention (NICE).
| • Reduction in health inequalities |
| • Cost savings associated with prevented cardiovascular episodes |
| • Prevention of other comorbidities, including cancer, lung diseases, and diabetes |
| • Cost saving associated with prevented cardiovascular disease: medications, primary care appointments, diagnostic tests, and ambulatory care |
| • Savings on labour costs associated with loss of productivity and social benefits granted to working-age people due to illness |
| • Increased life expectancy and quality of life |
National Institute for Health and Clinical Excellence.20
And yet despite recognising the advantages of population strategies and the importance of political commitment to CVD prevention, guidelines tend to gloss over recommendations for action at this level, with the exception of prohibiting tobacco use. Regarding the individual strategy, the EUROACTION project has shown that, in daily clinical practice and for both primary and secondary prevention, achieving lasting lifestyle changes and meeting treatment objectives recommended by guidelines is possible, thanks to integral, multidisciplinary programmes for patients and their families.21
Who should benefit from CVD prevention?Strategies and estimating riskThe risk of experiencing atherosclerotic CVD is determined by multiple factors and the way they interact. For this reason, guidelines stress the importance of evaluating the clinical intervention based on the total cardiovascular risk (CVR) or probability of experiencing a cardiovascular episode within a set time frame. They do recognise, however, that there is not enough direct evidence to affirm that this approach would be more effective than treating each of the patient's risk factors separately.
The SCORE system is used to measure CVR (www.heartscore.org); it includes levels of HDL cholesterol and it has been calibrated for the Spanish population.22 Some have criticised the system for only taking fatal episodes into account. The decision may be justified, however, by the valid, stable diagnostic criteria it provides and because it permits easy recalibration for changes in CVD mortality. Most Spanish regions use SCORE, but some apply Framingham or REGICOR,23 a method that has been validated for estimating 10-year risk of coronary heart disease in the Spanish population.24 Regardless of the method used to calculate risk, the most important step is estimating CVR as a cardiovascular disease prevention strategy for clinical practice; this is followed by applying guideline recommendations based on best judgement.
When should risk level be estimated?Screening for risk factors is recommended for men over 40 and for women over 50, if they have one or more known risk factors, a family history of early CVD, if requested by the patient, or if symptoms suggest CVD and that disease would have to be ruled out. Furthermore, doctors should increase their efforts to calculate CVR in socioeconomically disfavoured individuals, who have a larger probability of presenting multiple associated risk factors.
CVR functions are simple instruments that should be used with the patient's electronic medical record. However, their characteristics, uses, and limitations should also be known in daily clinical practice.
- •
CVR is a continuum, and there is therefore no clear threshold for when to start drug treatment. Doctors have established 4 risk categories: very high, high, moderate, and low.
- •
Other risk factors that are not contemplated by this function should also be considered (sedentary lifestyle, diabetes, socioeconomic stratum, family history, and numerous biomarkers), especially in patients with moderate CVR. Measuring heart rate is recommendable since an elevated resting rate is a risk factor, but no drug treatments are recommended for reducing heart rate as primary prevention.
- •
The guidelines present the concept of vascular age25,26: age adjusted by one or more risk factors to reflect the same level of risk shown by a person without risk factors. This is an intuitive, easy-to-use method of illustrating the probable decrease in life expectancy of a young individual with a low absolute risk but a high relative risk of CVD. The method is useful for informing the patient of his/her risk level, but not for making treatment decisions.
- •
Being aware that age is the main determinant of risk helps doctors avoid inappropriate treatment in the elderly; evidence in this population may be limited or non-existent.27
Risk functions display low sensitivity, since most cardiovascular episodes occur in people with moderate risk levels.28,29 This being the case, new biomarkers have been proposed, including high-sensitivity C-reactive protein, fibrinogen, homocysteine, and lipoprotein-associated phospholipase A2. Their ability to increase the predictive capacity of classic functions has not yet been demonstrated.30 These biomarkers could be included in daily clinical practice for individual assessments, rather than as tests offered directly to the patient, as is currently the case with certain genetic tests.
Psychosocial risk factorsThe guidelines recommend assessing the following psychosocial risk factors: low socioeconomic level, social isolation and lack of support, stress in the workplace and in family life, depression, anxiety, hostility, and type-D personality. In a study conducted in Girona, prevalence of classic risk factors was higher among the most disadvantaged social classes.31 Although social inequalities with regard to awareness of, treatment for, and control over those risk factors disappeared between 1995 and 2005, probably thanks to Spain's universal healthcare system, differences in commitment to healthy lifestyles are rising, and further efforts to reduce those differences will be needed.
Imaging techniquesUsing non-invasive imaging techniques to detect atherosclerosis is not supported by prospective randomised studies. These techniques are only useful for increasing predictive power, and possibly also to indicate a higher level of treatment in subjects at moderate risk. Measuring coronary artery calcification on the Agatston scale has a high negative predictive value. However, the radiation involved, the lack of a precise functional analysis of lesions, and the cost-benefit ratio are all obstacles to recommending this technique. Magnetic resonance imaging is a promising line of research, although it has yet to demonstrate its value as a screening tool for asymptomatic coronary lesions. On the other hand, ultrasound imaging measurement of intimal-medial thickness (an accepted non-invasive method of detecting asymptomatic carotid stenosis) and the ankle-brachial index are correlated with presence of coronary lesions, the total atherosclerosis load, and the cardiovascular prognosis. These are the 2 most widespread techniques according to recommendations in the guidelines. The ankle-brachial index may be unreliable (false positives) where arterial calcifications are present; this is a common scenario in patients with diabetes and AHT.
Other diseases with an increased risk of cardiovascular diseaseCertain diseases contribute to arteriosclerosis and thereby increase CVD risk, but evidence is insufficient to determine how preventive measures affect the prognosis of CVD. These diseases include the following:
- •
Flu: yearly flu vaccines are recommended for patients with CVD, and this measure is cost effective.32
- •
Obstructive sleep apnoea: hypoxia will trigger an increase in sympathetic activity with a rise in blood pressure (BP), which accelerates the atherosclerotic process. Apnoea screening and treatment is recommended for patients with AHT and ischaemic heart disease.
- •
Erectile dysfunction: while this condition is a marker and a predictor of CVD, it is not more precise than traditional risk scales.
- •
Periodontitis: debatable association with CVR. It should be treated alongside any classic risk factors.
- •
Complications of radiation therapy: radiotherapy is associated with arteriosclerotic lesions and a higher incidence of cardiovascular episodes. Guidelines recommend strict control over risk factors in these cases.
The guidelines propose improving nutritional and exercise habits, tolerance for stress, and treatment compliance through cognitive-behavioural methods such as motivational interviews.33,34 These can be undertaken by the patient's doctor or by family members. The methods respect the patient's autonomy by promoting shared decision-making using stepwise therapy. Motivational sessions may be individual or group-based. The approach to high-risk patients will ideally involve multiple professionals, including doctors, nurses, psychologists, physical therapists, nutritionists, and dietitians.
SmokingSmokers must be urged to stop smoking and offered assistance with that task. Public health initiatives, such as banning smoking in public places, are shown to be effective for decreasing the smoking habit. As such, they should be maintained in all of Spain's regions with no exceptions.
The most important predictor of smoking cessation is motivation,35,36 which increases with the help of group or individual sessions and family support. Systematic monitoring by doctors and nursing staff,37 together with pharmacological support,38 will increase the likelihood of success. Nicotine substitution therapy, varenicicline, and bupropion are effective in the first months of cessation. Nortriptyline and clonidine are effective, but considered second-line treatments due to their side effects. There is no evidence regarding the efficacy of acupuncture, acupressure, laser treatment, hypnotherapy, or electrostimulation therapy, or cystine, a partial nicotine receptor agonist.
NutritionThe guidelines list healthy eating as the key to preventing cardiovascular disease and provide updated recommendations. They highlight the controversial impact of saturated fat on CVD incidence and recognise that the type of fat is more important than the total amount. Unsaturated fatty acids exert a protective effect, while trans fatty acids are associated with a marked increase in risk (up to 23%) with consumption of only 5 grammes, the amount we might find in a portion of chips or chicken from a fast-food restaurant.39 Other updated sections refer to the effectiveness of phytosterol-enriched foods to reduce cholesterol, although their potential effect on CVR has not been demonstrated; the 20% increase in CVR associated with consuming one sugared beverage daily40; and emphasis on eating habits using the Mediterranean diet as the reference model for CVD prevention.41
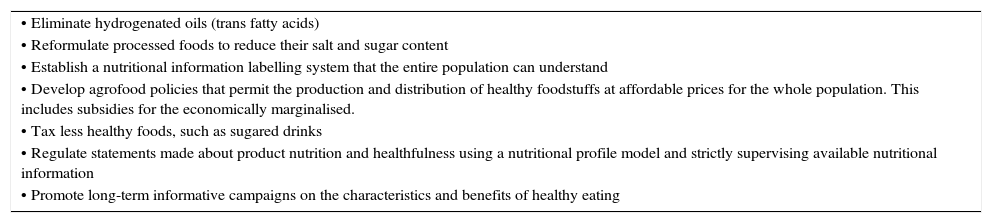
The guidelines emphasise establishing personalised recommendations, and, in general, the importance of using cognitive methods to help people adopt healthier lifestyles, while not entering into potential population-wide prevention activities. Eating habits are strongly conditioned by the person's social, political, physical, economic, and cultural environment. As such, population-based educational, regulatory, or economic measures intended to foster an environment that will facilitate following a healthy diet are essential for CVD prevention. Some of the most cost-effective interventions are listed in Table 3.42
Population-based CVD prevention measures.
| • Eliminate hydrogenated oils (trans fatty acids) |
| • Reformulate processed foods to reduce their salt and sugar content |
| • Establish a nutritional information labelling system that the entire population can understand |
| • Develop agrofood policies that permit the production and distribution of healthy foodstuffs at affordable prices for the whole population. This includes subsidies for the economically marginalised. |
| • Tax less healthy foods, such as sugared drinks |
| • Regulate statements made about product nutrition and healthfulness using a nutritional profile model and strictly supervising available nutritional information |
| • Promote long-term informative campaigns on the characteristics and benefits of healthy eating |
The guidelines stress the importance of physical activity for reducing cardiovascular morbidity and mortality.43 In addition to improving the patient's physical condition, myocardial perfusion, and endothelial function, exercise has antithrombotic and anti-arrhythmic effects. It is able to generate myocardial ischaemic conditioning, which will increase myocardial tolerance for longer subsequent ischaemic episodes, thus reducing myocardial damage and risk of ventricular fibrillation.
The minimum amount of physical activity recommended for a healthy adult is 2.5 to 5hours weekly for moderate exercise, or 1 to 2.5hours weekly for vigorous exercise, distributed in intermittent periods of more than 10minutes on most days of the week.44
Physical activity may reduce mortality by as much as 30% among patients with CVD45; recommendations must be adapted to each patient's clinical characteristics. The most limited patients must also engage in light exercise under safe and supervised conditions; this will allow them to remain independent as well as improving mood. Several studies show that high-intensity interval training is more effective than moderate-intensity continuous exercise, especially in patients with chronic heart failure.46
Management of psychosocial factorsInterviews or adapted questionnaires assessing psychosocial factors are recommended for use in clinical practice.47 Low socioeconomic level, social isolation, stress, anxiety, depression, hostility, and type-D personality characterised by negative affectivity and social inhibition are cardiovascular risk factors that predict a poorer clinical course and prognosis. In addition to the biological mechanisms linking them to CVD pathogenesis, these characteristics are obstacles to treatment compliance and lifestyle modification.
Another novelty is the evidence that personalised psychological interventions are effective for diminishing psychosocial stress and promoting healthy lifestyles.48 The guidelines stress individual or group education on psychosocial risk factors and disease management, cognitive-behavioural therapy, stress management programmes, and relaxation techniques (meditation, autogenous training, breathing, yoga, muscle relaxation). Patients with symptoms of depression, anxiety, and hostility should be treated with psychotherapy or medication.
Stress control programmes and group therapy (especially in women) are shown to be effective at controlling CVD development and risk factors. They are also associated with improved prognosis.49
Body weightObesity and overweight are independently linked to risk of death due to CVD. There is a positive linear association between body mass index (BMI) and all causes of death. The lowest association is with BMIs between 20 and 25kg/m2. BMIs below this range have not been shown to offer protection against CVD, or to increase cardiovascular morbidity and mortality. Furthermore, overweight has adverse effects for multiple risk factors: dyslipidaemia, ATH, increased insulin resistance and pro-inflammatory/prothrombotic states, albuminuria, increased sympathetic activity, endothelial dysfunction, and vascular alterations (atrial fibrillation, heart failure, etc.).
Weight loss is recommended for individuals with overweight and obesity, since it is associated with favourable effects on BP and the lipid profile that contribute to CVD prevention. The guidelines propose 2 levels of action:
- 1.
Avoid weight gain with waist circumference ≥94cm in men or ≥80cm in women.
- 2.
Recommend weight loss with waist circumference ≥102cm in men or ≥88cm in women.
Although the association between central obesity indicators and diabetes and cardiovascular mortality/overall mortality may be greater than the association with BMI, evidence remains limited.50
Every region in Spain includes anthropometric data (height and weight) in each patient's medical history to calculate BMI. Nevertheless, and despite recent and unfavourable developments in overweight indicators,51 none of Spain's regional health systems lists the level of control over obesity, diet, or physical activity among its care quality indicators.23
Arterial blood pressureIndividuals with hypertension may present associated cardiovascular risk factors along with impairment of target organs or subclinical CVD. This must be considered when estimating CVR and making treatment decisions. Urinary excretion of albumin must be monitored due to its continuous relationship with CVD and non-cardiovascular mortality. BP measurements must be repeated and the patient should be encouraged to record BP at home or undergo 24-hour ambulatory BP monitoring for more accurate diagnosis and treatment. Doctors must also be aware that subclinical injury to target organs predicts cardiovascular death independently from the SCORE rating, especially in subjects at low or moderate risk.52
Combining 2 antihypertensive drugs is necessary for BP control in a large percentage of patients with AHT, since this approach is clearly more effective than raising the dosage of a single drug. Combination therapy with beta-blockers and diuretics should be avoided because it promotes development of diabetes. Antihypertensive treatment is beneficial in subjects older than 80 with a target systolic BP<150mmHg.53
The classic recommendation of lowering BP below 130/80mmHg in patients with diabetes or high CVR does not have solid support from current evidence except in stroke patients; a J-curve has been described in CVD, especially in coronary disease. In this patient group, it seems to be prudent to lower BP to 130-139/80-85mmHg, and possibly to levels in the lower limits of this range, but not below 130/80mmHg.
DiabetesSCORE should only be used to estimate risk in patients with type 1 diabetes with no injury to target organs. Patients with type 2 diabetes have a high to very high CVR, although not all of them will have the same risk, especially those with a shorter history of the disease.54 The American Diabetes Association guidelines recommend identifying patients with lower risk levels by selecting those without metabolic syndrome, other risk factors, or complications.55
These guidelines promote intensive, coordinated interventions targeting all modifiable CVR factors associated with diabetes as the most effective strategy for reducing CVR in these patients. Nevertheless, the aggressiveness of the treatment and the therapeutic objectives for each risk factor will vary according to the risk/benefit ratio of that treatment. For example, intensive treatment is employed in the case of dyslipidaemia, since it offers the best risk/benefit ratio and allows for more flexible BP and glycaemia targets, but aspirin is not recommended in patients with no clinical evidence of CVD.
LipidsThe approach described in the guidelines is based on the need to improve the percentage of patients meeting their treatment objectives for LDL cholesterol.56 Therapeutic action is distributed according to 5 ranges of LDL cholesterol values and 4 CVR levels. Guidelines recommend reaching and maintaining an LDL cholesterol level below 70mg/dL when very high risk conditions are present, including chronic kidney disease (glomerular filtration rate<30mL/min/1.73m2), or decreasing LDL by more than 50% with respect to baseline if the above target cannot be reached. High doses of potent statins and combination treatment (statins with bile acid sequestrants or statins with ezetimibe) are indicated whenever they are necessary to reach objectives.
Triglyceride and HDL cholesterol levels are recognised as independent risk factors, and the latter lipid fraction is used in estimating CVR. Although no treatment objectives have been established for HDL cholesterol, treatment may be considered for levels below 1mmol/L (∼40mg/dL) in men and 1.2mmol/L (∼45mg/dL) in women. We must not overlook that inhibitors of cholesteryl ester transfer protein (CETP) have been proved effective for increasing levels of HDL cholesterol. However, rather than decreasing cardiovascular mortality, they seem to have the opposite effect.57
In the section on dyslipidaemia treatment, the guidelines do not contemplate other, non-atherothrombotic types of ischaemia. Nevertheless, most patients who have experienced a transient ischaemic attack (TIA) or cerebral infarct of another aetiology can be treated with statins. Treatment is indicated in these patients because of their associated CVD and high CVR (ischaemic heart disease, peripheral artery disease, diabetes mellitus),58 and statins will not increase their risk of brain haemorrhage.59 A recent recommendation calls for including non-atherothrombotic cerebral ischaemia as an equivalent coronary risk, although the level of evidence is lower than in the case of the atherothrombotic type.60
Anti-platelet treatmentAspirin treatment for primary prevention reduces vascular episodes, but not cardiovascular or overall mortality.61 Furthermore, the increased risk of haemorrhage detracts from its possible benefits. Based on the above, aspirin treatment is not recommended for patients without established CVD, including diabetic patients or those with chronic kidney disease. The guidelines do not establish a threshold of risk at which prophylaxis should be considered, in contrast with the 2007 guidelines.
In patients with CVD, aspirin dosed at 75 to 150mg/day decreases vascular episodes, cardiovascular mortality, and total mortality.61 Its indication is class I/A for ischaemic heart disease, ischaemic stroke or TIA, and symptomatic peripheral artery disease. In patients with an aspirin allergy or intolerance, clopidogrel is the alternative of choice.62
Dual antiplatelet therapy (aspirin plus clopidogrel or another P2Y12 inhibitor) is indicated during one year in patients with acute coronary syndrome (ACS). An initial loading dose is given regardless of the type of ACS (with or without ST segment elevation) and whether or not a coronary intervention was performed. In patients at high risk for bleeding (on anticoagulants), the duration of dual therapy can be shortened to 4 to 6 weeks, especially in patients without a percutaneous coronary invention or those with a bare metal stent. It is preferable to avoid using covered or drug-eluting stents (DES) in such cases, since they require a long course (1 year) of dual antiplatelet therapy. This problem, which arises frequently in clinical practice, is not addressed in the guidelines.
One controversial recommendation calls for using the new P2Y12 receptor antagonists prasugrel and ticagrelor in association with aspirin after ACS. These drugs would take precedence over clopidogrel, which doctors have experience using. Although clinical trials of each of these drugs in patients with ACS show either one to be somewhat superior to clopidogrel,63,64 patients in the prasugrel trial had had percutaneous coronary intervention, and positive results were accompanied by an increase in the rate of severe haemorrhages.63 These events were more frequent in specific patient subgroups (prior stroke, older than 75 years, and low body weight). Considering that the level of evidence is the same (I/B), it is surprising to find that new antiplatelet drugs are recommended over clopidogrel for all ACS cases, whether or not they have undergone an intervention; this is doubly surprising considering the direct costs of both alternatives. Furthermore, the greatest benefit of prasugrel and ticagrelor is observed in patients with acute myocardial infarction and ST segment elevation treated with percutaneous coronary intervention; most local protocols prioritise use of new antiplatelet drugs in this patient subgroup almost exclusively.
The ACC/AHA guidelines for the management of patients with ST-elevation rank all 3 drugs at the same evidence/recommendation level (I/B), which seems to be more reasonable. They also recommend a year of treatment after percutaneous revascularisation, while listing exceptions and contraindications.65 Early withdrawal of dual antiplatelet therapy is to be avoided since it is accompanied by increased risk of repeat infarct and death; bleeding should also be prevented (including gastric protection). Maintaining dual antiplatelet drugs for more than a year is associated with no benefits and a higher risk of bleeding.66 In patients with chronic, stable CVD, dual antiplatelet therapy is not more effective than aspirin alone for reducing new cardiovascular episodes.67 Likewise, there are no demonstrated benefits of dual antiplatelet drugs compared to clopidogrel in patients with TIA or ischaemic stroke, while the risk of bleeding remains higher.68
Treatment complianceThe guidelines attach considerable importance to the low level of treatment compliance that has been observed, especially in elderly and low-income populations, since it impacts patient prognosis and healthcare costs. Poor treatment compliance has multiple causes, including the health system, the disease, patient, treatment, and socioeconomic context. The text indicates that compliance with lipid-lowering treatment decreases as patient copays increase, even in patients at high risk for ischaemic heart disease.69 Doctors must be mindful of this when prescribing treatment. Lastly, we provide a series of recommendations for promoting treatment adherence; reducing the number of doses daily is the single most effective strategy. This being the case, nursing staff should play a more active role as a means of improving treatment compliance.
Where should CVD prevention strategies be employed?Cardiovascular disease prevention in primary care: the role of nursing staffCompared to the usual care model, multidisciplinary CVD prevention programmes coordinated by a nurse effectively improve control over risk factors, glycaemia, willingness to exercise, and treatment adherence. They also decrease the number of cardiovascular episodes, while improving the patient's perception of his/her state of health, especially in secondary prevention programmes.70 Also compared to typical care for patients with coronary heart disease or high CVR, the individual and family-based approaches in the EUROACTION study also delivered lifestyle improvements (diet and physical activity) and better control over risk factors in both hospitals and primary care.21
The most appropriate model seems to be that of the nurse-case manager including the following strategies: intensive management of the number of individual and family consultations, protocol-based interventions, group and individual health education, motivational sessions promoting shared decision-making, and establishing goals with patients and families. Nevertheless, further studies are needed to establish the number, type, and duration of the consultations needed in order to achieve lifestyle changes, acceptable control of risk factors, and long-term treatment compliance. Research must also determine what knowledge and skills are necessary to effectively implement CVD prevention programmes.
Cardiovascular disease prevention in primary care: the general practitioner's roleThe guidelines highlight the importance of general practitioners in cardiovascular disease prevention: they identify high-risk patients, make treatment decisions, and provide long-term follow-up. Tools such as SCORE are recommended for classifying risk, since intuitive evaluations based on personal experience underestimate the risk level.
The EUROASPIRE III study, carried out in 12 European countries, reports that Spain needs better monitoring of high-risk patients without CVD. This is especially true for the factors BMI (15% vs 19.2% on average in non-diabetic patients; 8.9% vs 11.1% in diabetic patients) and BP (27.0% vs 36.1% in non-diabetics; 11.2% vs 13.4% in diabetic patients). Nevertheless, lipid control is reported as better than the mean (40.5% vs 33.7% in non-diabetic patients; 36.8% vs 33.0% in diabetic patients).71
In one study carried out in a sample of 1390 general practitioners representing the entire territory of Spain, 60% of the respondents did not evaluate CVR; the main obstacle cited by 81% of these doctors was lack of time in consultations.6 General practitioners in the Region of Madrid apply risk tables to 45% of their patients with hypertension and 52% of those with dyslipidaemia, despite conceding that evaluating CVR is a better strategy than assessing risk factors one by one.72 The main obstacles cited for applying tables were lack of time, poor consensus, and lack of a computer programme to do so. Different proposals address how to eliminate these difficulties: clear and easy-to-use guidelines, incentives, educational material for patients, and computerised medical records complete with tools for automatically calculating CVR.73
Cardiovascular disease prevention in primary care: the cardiologist's roleHospital cardiology departments should periodically verify proper implementation of treatments after patients are discharged following CVD episodes, and cardiologists should be available to answer questions about treatment for special cases.
Cardiovascular disease prevention in primary care: self-help programmesAlthough the evidence about the efficacy of self-help groups for reducing CVR is limited, these groups may increase independence and quality of life among CVD patients. They do so by increasing awareness of the need for good management and monitoring of risk factors and the importance of physical exercise.
Cardiovascular disease prevention in primary care: hospital programmesOptimal treatment when the patient is discharged after a cardiovascular episode is fundamental for the final outcome, and both pharmacological treatment and lifestyle changes should be prescribed. One effective and innovative strategy involves using programmes that evaluate improvement of the quality of preventive measures by means of internal audits or check-lists.74
Structured cardiac rehabilitation and secondary prevention programmes in a specialist centre improve clinical stability and symptom control, reduce CVR, and deliver better treatment compliance, which in turn improves the patient's quality of life and prognosis.45 Furthermore, cardiac rehabilitation is considered cost-effective after an acute coronary episode since it improves outcomes and reduces medical costs and the number of hospitalisations.75 Some researchers stress the importance of reinforcing and maintaining these interventions, since the number of rehabilitation sessions (session duration and intensity) and the motivation of the participant are linked to better prognosis.76
Despite the beneficial effects of cardiac rehabilitation programmes, the participation rate after a cardiac episode is much lower than we would like. In Europe, only 30% of all eligible patients participate in these programmes, with significant differences between countries (in Spain, 1.5% to 3%).77 Participation is especially low among women, the elderly, and patients with comorbidities, and these groups should be encouraged to use these programmes.75
Political action at the European levelThe European Heart Network is a consortium of heart associations and non-governmental organisations with similar interests; half the members of the participating bodies are cardiovascular patients. This network and the Spanish Society of Cardiology worked in close cooperation to pave the way for the 2007 presentation of the European Heart Health Charter before the European Parliament. It was adopted by the European Commission, WHO/Europe, and more than 30 European countries. In 2009, the Spanish Society of Cardiology joined efforts with other medical societies to establish the European Alliance for Chronic Diseases, representing more than 100000 healthcare professionals. The Alliance aims to monitor the 4 common risk factors identified on the population level: tobacco, nutrition, alcohol, and a sedentary lifestyle.
In conclusion, better CVD prevention will require a true alliance between politicians, government agencies, medical and professional associations, health foundations, consumer groups, patients, and families. Such an alliance must foster population-wide and individual strategies by using the entire spectrum of available scientific evidence, from clinical trials in patients to observational studies and mathematical models for evaluating interventions at the population level, including analyses of their cost-effectiveness.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Royo-Bordonada MA, Lobos Bejarano JM, Villar Alvarez F, Sans S, Pérez A, Pedro-Botet J, et al. Comentarios del Comité Español Interdisciplinario de Prevención Cardiovascular (CEIPC) a las Guías Europeas de Prevención Cardiovascular 2012. Neurología. 2016;31:195–207.
This statement has been published simultaneously, in paper or online format, in each of the official journals of the 15 medical societies participating in the Spanish Interdisciplinary Cardiovascular Prevention Committee (CEIPC), and by the Directorate General of Public Health, a division of the Spanish Ministry of Health, Social Services, and Equality.