Virtual reality (VR) is used in the field of rehabilitation/physical therapy to improve patients’ functional abilities.
The last 5 years have yielded numerous publications on the use of VR in patients with neurological disease which aim to establish whether this therapeutic resource contributes to the recovery of motor function.
DevelopmentThe following databases were reviewed: Cochrane Original, Joanna Briggs Connect, Medline/Pubmed, Cinahl, Scopus, Isi Web of Science, and Sport-Discus.
We included articles published in the last 5 years in English and/or Spanish, focusing on using RV to improve motor function in patients with stroke.
From this pool, we selected 4 systematic reviews and 21 controlled and/or randomised trials. Most studies focused on increasing motor function in the upper limbs, and/or improving performance of activities of daily living. An additional article examines use of the same technique to increase motor function in the lower limb and/or improve walking and static-dynamic balance.
Discussion and conclusionsStrong scientific evidence supports the beneficial effects of VR on upper limb motor recovery in stroke patients. Further studies are needed to fully determine which changes are generated in cortical reorganisation, what type of VR system is the most appropriate, whether benefits are maintained in the long term, and which frequencies and intensities of treatment are the most suitable.
La realidad virtual (RV) se utiliza en rehabilitación con el objetivo de mejorar las capacidades funcionales.
Es en estos últimos 5 años cuando aparece el mayor número de publicaciones sobre la utilización de RV en pacientes con patología neurológica, con el objetivo de determinar si este recurso terapéutico aporta mejoras en la recuperación de la función motora.
DesarrolloSe ha realizado una revisión sistemática consultando las bases de datos Cochrane Original, Joanna Briggs Connect, Medline/Pubmed, Cinahl, Scopus, Isi Web of Science y Sport-Discus.
Se han incluido artículos publicados en los últimos 5 años, publicados en inglés y/o español, realizados en pacientes con ictus, y que utilicen la RV para mejorar la función motora.
Finalmente, se han seleccionado 4 revisiones sistemáticas y 21 ensayos clínicos controlados y/o aleatorizados.
La mayoría de los estudios tienen como objetivo mejorar la función motora del miembro superior, y/o mejorar la realización de las actividades de la vida diaria, aunque también hay algún artículo cuyo objetivo es mejorar la función motora del miembro inferior-mejorar la marcha, así como mejorar el equilibrio estático-dinámico.
Discusión y conclusionesHay fuertes evidencias científicas de los efectos beneficiosos de la RV en la recuperación motora del miembro superior en pacientes con ictus. Se necesitan estudios que profundicen en cuáles son los cambios generados en la reorganización cortical, qué tipo de sistema de RV es mejor utilizar, determinar si los resultados se mantienen a largo plazo, y definir qué frecuencias e intensidades de tratamiento son las más adecuadas.
Since J. Lamier first used the term ‘virtual reality’ (VR) in 1986, its definition has changed considerably as new 3-dimensional (3D) technologies have developed.1–3 One of the most widely accepted definitions today states that VR is the computer-generated simulation of a real environment which enables the user to interact with certain elements in the simulated setting via a man-machine interface.3
When VR is used, virtual environments and objects provide the user with visual information (which can be viewed in a head-mounted display, on a projection system, or on a flat screen), as well as auditory, tactile, olfactory, and motion information.3 There is a great variety of interfaces for interacting with the virtual environment, ranging from common devices (mouse, keyboard, joystick) to more complex ones with motion capture systems or even haptic devices, which provide tactile feedback and make users feel as though they are manipulating real objects.3 The type of VR environment generated will depend on the equipment and software used.4
Virtual environments may vary in terms of the degree of immersion of the user. The term ‘immersion’ refers to the extent to which the user perceives that they are in the virtual environment rather than the real world and is related to the design of both the software and the hardware.3,5–8 Based on this concept, we can classify VR systems and devices into 2 categories:
- -
Immersive VR systems fully integrate the user into the virtual environment. The user only sees computer-generated images, typically by means of a device which blocks out perception of the real world.7,8 The most widely used immersive systems at present are Glasstrom, IREX, and PlayStation EyeMotion.9
- -
Semi-immersive or non-immersive VR systems are those in which the user perceives both the real world and part of the virtual environment. With these systems, the user is not fully immersed in the virtual environment.7,8 The most widely used non-immersive systems at present are Virtual Teacher, Cyberglobe, Virtual Reality Motion, Pneumoglobe, and Nintendo-Wii.9
Some clinicians have started to include virtual reality in rehabilitation and physical therapy to improve motor function. Today, this technology is being increasingly used in the treatment of neurological disorders (stroke, Parkinson's disease [PD], spinal cord lesions, cerebral palsy). This has had an unquestionably positive impact on assessments, interventions, and patients’ motivation to achieve the highest possible level of functional improvement.7,9–11
In the last few years, a large number of studies have addressed the use of VR in stroke patients with the aim of evaluating the validity and ease of use of these devices.12–17 However, most of the articles analysing how this therapeutic resource improves motor rehabilitation in these patients have been published in the past 5 years.18–20
In this systematic review, we aimed to identify the VR systems and devices used with therapeutic purposes in stroke patients, and define the motor symptoms most frequently treated with VR (the effects and benefits of VR).
MethodsInclusion criteria- -
We included all articles meeting the following criteria:
- –
Meta-analyses, systematic reviews (SR), controlled clinical trials (CCT), and randomised controlled clinical trials (RCT)
- –
Articles published in the past 5 years (2009-2014) in either English, Spanish, or Portuguese
- –
Studies on patients with stroke regardless of age or stage of disease
- –
Studies using any type of VR intervention or therapy (immersive or non-immersive), either isolated or in combination with other therapies, and including either a placebo group, a non-intervention group, or a group receiving other therapies
- –
Studies using VR with the aim of improving motor function
- –
Studies that define study variables and measure results with specific and validated tools
We conducted a literature search (June 2014) in the main healthcare databases.
We first investigated 2 databases specific for SR (the Cochrane Database of Systematic Reviews, the Joanna Briggs) to determine whether the topic of our study had already been addressed by other authors.
We found a total of 4 SR meeting our inclusion criteria. After analysing them, we concluded that these SR did not provide sufficient scientific evidence on the efficacy and effectiveness of VR in the treatment of motor dysfunction in patients with a diagnosis of stroke.
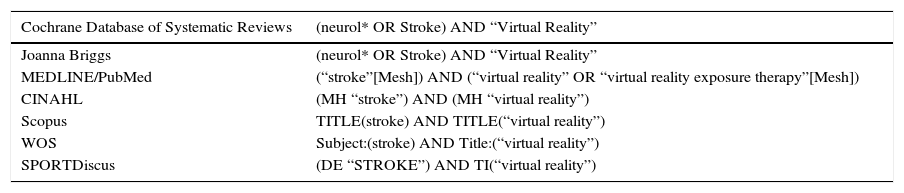
We later conducted a literature search in other more general scientific databases (PubMed, CINAHL, Scopus, ISI WEB of Science, and SPORTDiscus). We used the following search strategy, (“stroke” AND [“virtual reality” OR “virtual reality exposure therapy”]), modified slightly depending on the database (Table 1).
Search strategy.
| Cochrane Database of Systematic Reviews | (neurol* OR Stroke) AND “Virtual Reality” |
|---|---|
| Joanna Briggs | (neurol* OR Stroke) AND “Virtual Reality” |
| MEDLINE/PubMed | (“stroke”[Mesh]) AND (“virtual reality” OR “virtual reality exposure therapy”[Mesh]) |
| CINAHL | (MH “stroke”) AND (MH “virtual reality”) |
| Scopus | TITLE(stroke) AND TITLE(“virtual reality”) |
| WOS | Subject:(stroke) AND Title:(“virtual reality”) |
| SPORTDiscus | (DE “STROKE”) AND TI(“virtual reality”) |
Using ZOTERO reference management software, we downloaded all the results and removed duplicate references. After that, 2 authors of this review article independently read the titles and abstracts of all the remaining articles and handpicked those meeting our inclusion criteria. These 2 authors subsequently compared their selections. In case of discrepancy, those studies were included or excluded by consensus.
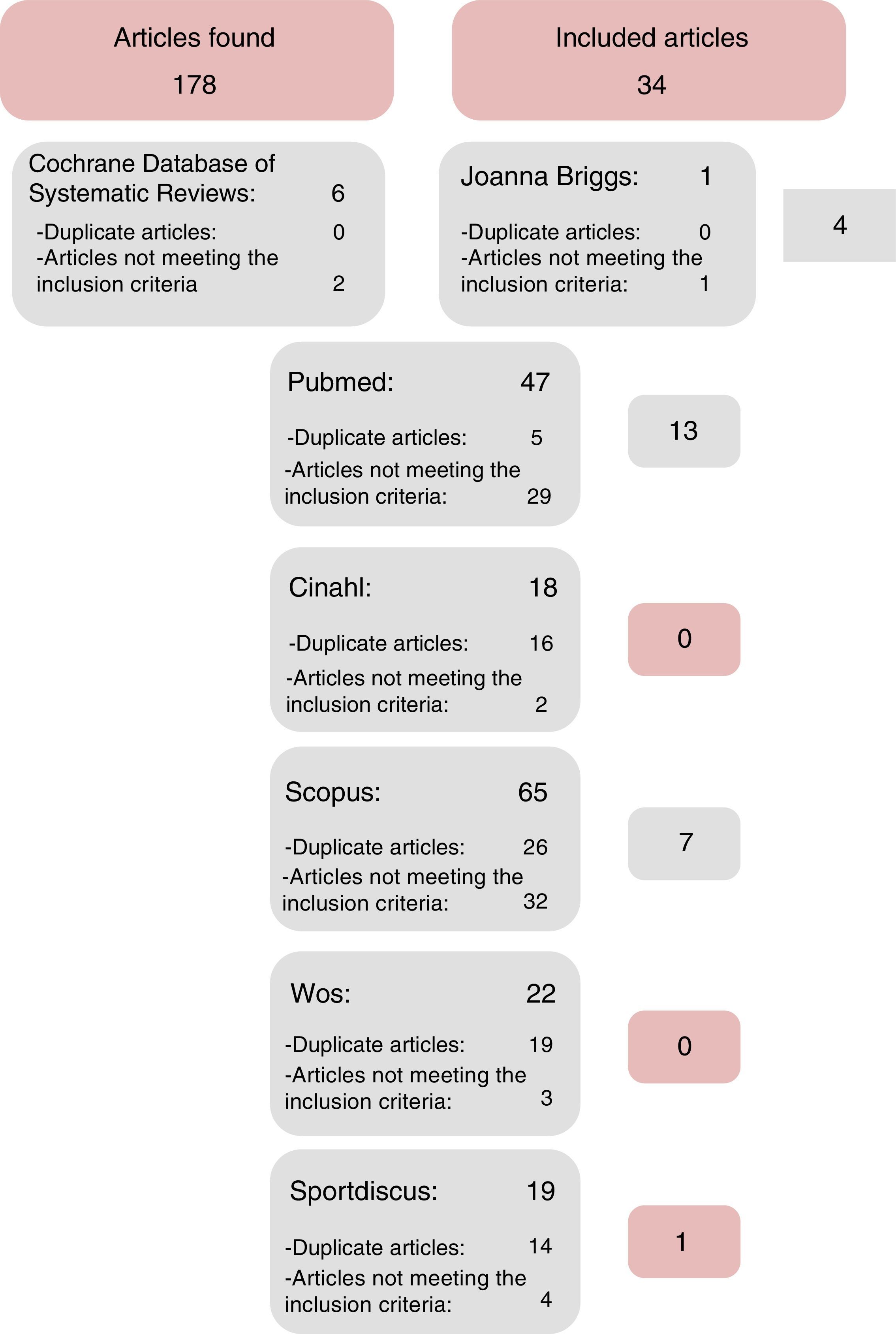
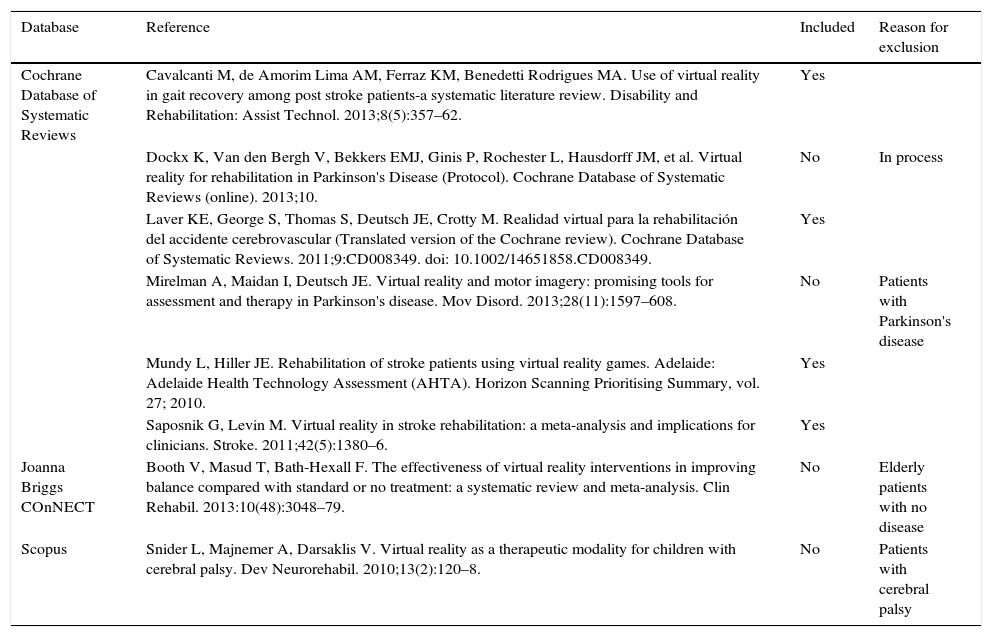
Search resultsWe found a total of 178 references; of these 80 were duplicates and 73 did not meet our criteria and were therefore excluded (Table 2), leaving 25 references which did meet our inclusion criteria (1 meta-analysis, 3 SR, and 21 CCT and/or RCT) (Fig. 1).
Selected articles from databases specialised in systematic reviews.
| Database | Reference | Included | Reason for exclusion |
|---|---|---|---|
| Cochrane Database of Systematic Reviews | Cavalcanti M, de Amorim Lima AM, Ferraz KM, Benedetti Rodrigues MA. Use of virtual reality in gait recovery among post stroke patients-a systematic literature review. Disability and Rehabilitation: Assist Technol. 2013;8(5):357–62. | Yes | |
| Dockx K, Van den Bergh V, Bekkers EMJ, Ginis P, Rochester L, Hausdorff JM, et al. Virtual reality for rehabilitation in Parkinson's Disease (Protocol). Cochrane Database of Systematic Reviews (online). 2013;10. | No | In process | |
| Laver KE, George S, Thomas S, Deutsch JE, Crotty M. Realidad virtual para la rehabilitación del accidente cerebrovascular (Translated version of the Cochrane review). Cochrane Database of Systematic Reviews. 2011;9:CD008349. doi: 10.1002/14651858.CD008349. | Yes | ||
| Mirelman A, Maidan I, Deutsch JE. Virtual reality and motor imagery: promising tools for assessment and therapy in Parkinson's disease. Mov Disord. 2013;28(11):1597–608. | No | Patients with Parkinson's disease | |
| Mundy L, Hiller JE. Rehabilitation of stroke patients using virtual reality games. Adelaide: Adelaide Health Technology Assessment (AHTA). Horizon Scanning Prioritising Summary, vol. 27; 2010. | Yes | ||
| Saposnik G, Levin M. Virtual reality in stroke rehabilitation: a meta-analysis and implications for clinicians. Stroke. 2011;42(5):1380–6. | Yes | ||
| Joanna Briggs COnNECT | Booth V, Masud T, Bath-Hexall F. The effectiveness of virtual reality interventions in improving balance compared with standard or no treatment: a systematic review and meta-analysis. Clin Rehabil. 2013:10(48):3048–79. | No | Elderly patients with no disease |
| Scopus | Snider L, Majnemer A, Darsaklis V. Virtual reality as a therapeutic modality for children with cerebral palsy. Dev Neurorehabil. 2010;13(2):120–8. | No | Patients with cerebral palsy |
| Articles selected from general content databases | |||
|---|---|---|---|
| Database | Reference | Included | Reason for exclusion |
| MEDLINE-PubMed | Bowler M, Amirabdollahian F, Dautenhahn K. Using an embedded reality approach to improve test reliability for NHPT tasks. IEEE Int Conf Rehabil Robot. 2011;2011:5975343. | No | Improving motor function with VR was not the study aim |
| Cameirão MS, Badia SB i, Duarte E, Frisoli A, Verschure PFMJ. The combined impact of virtual reality neurorehabilitation and its interfaces on upper extremity functional recovery in patients with chronic stroke. Stroke. 2012;43(10):2720–8. | Yes | ||
| Carlozzi NE, Gade V, Rizzo AS, Tulsky DS. Using virtual reality driving simulators in persons with spinal cord injury: three screen display versus head mounted display. Disabil Rehabil Assist Technol. 2013;8(2):176–80. | No | Improving motor function with VR was not the study aim | |
| Casadio M, Pressman A, Acosta S, Danzinger Z, Fishbach A, Mussa-Ivaldi FA, et al. Body machine interface: remapping motor skills after spinal cord injury. IEEE Int Conf Rehabil Robot. 2011;2011:5975384. | No | No control group | |
| Chen C-L, Chen C-Y, Liaw M-Y, Chung C-Y, Wang C-J, Hong W-H. Efficacy of home-based virtual cycling training on bone mineral density in ambulatory children with cerebral palsy. Osteoporos Int. 2013;24(4):1399–406. | No | Study topic: home-based therapy | |
| Chen C-H, Jeng M-C, Fung C-P, Doong J-L, Chuang T-Y. Psychological benefits of virtual reality for patients in rehabilitation therapy. J Sport Rehabil. 2009;18(2):258–68. | No | Improving motor function with VR was not the study aim | |
| Cherniack EP. Not just fun and games: applications of virtual reality in the identification and rehabilitation of cognitive disorders of the elderly. Disabil Rehabil Assist Technol. 2011;6(4):283–9. | No | Improving motor function with VR was not the study aim | |
| Cho KH, Lee KJ, Song CH. Virtual-reality balance training with a video-game system improves dynamic balance in chronic stroke patients. Tohoku J Exp Med. 2012;228(1):69–74. | Yes | ||
| Cho KH, Lee WH. Virtual walking training program using a real-world video recording for patients with chronic stroke: a pilot study. Am J Phys Med Rehabil. 2013;92(5):371–80. | Yes | ||
| Crosbie JH, Lennon S, McGoldrick MC, McNeill MDJ, McDonough SM. Virtual reality in the rehabilitation of the arm after hemiplegic stroke: a randomised controlled pilot study. Clin Rehabil. 2012;26(9):798–806. | Yes | ||
| Da Silva Cameirão M, Bermúdez I, Badia S, Duarte E, Verschure PFMJ. Virtual reality based rehabilitation speeds up functional recovery of the upper extremities after stroke: a randomised controlled pilot study in the acute phase of stroke using the rehabilitation gaming system. Restor Neurol Neurosci. 2011;29(5):287–98. | Yes | ||
| Dos Santos Mendes FA, Pompeu JE, Modenesi-Lobo A, Guedes da Silva K, Oliveira TP, Peterson-Zomignani A, et al. Motor learning, retention and transfer after virtual-reality-based training in Parkinson's disease-effect of motor and cognitive demands of games: a longitudinal, controlled clinical study. Physiotherapy. 2012;98(3):217–23. | No | Patients with Parkinson's disease | |
| Galvin J, McDonald R, Catroppa C, Anderson V. Does intervention using virtual reality improve upper limb function in children with neurological impairment: a systematic review of the evidence. Brain Inj. 2011;25(5):435–42. | No | Patients with neurological impairment other than cerebral palsy | |
| Griffin HJ, Greenlaw R, Limousin P, Bhatia K, Quinn NP, Jahanshahi M. The effect of real and virtual visual cues on walking in Parkinson's disease. J Neurol. 2011;258(6):991–1000. | No | Patients with Parkinson's disease | |
| Hoffmann U, Deinhofer M, Keller T. Automatic determination of parameters for multipad functional electrical stimulation: application to hand opening and closing. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:1859–63. | No | No VR use | |
| Housman SJ, Scott KM, Reinkensmeyer DJ. A randomised controlled trial of gravity-supported, computer-enhanced arm exercise for individuals with severe hemiparesis. Neurorehabil Neural Repair. 2009;23(5):505–14. | Yes | ||
| Kim JH, Jang SH, Kim CS, Jung JH, You JH. Use of virtual reality to enhance balance and ambulation in chronic stroke: a double-blind, randomised controlled study. Am J Phys Med Rehabil. 2009;88(9):693–701. | Yes | ||
| King CE, Wang PT, Chui LA, Do AH, Nenadic Z. Operation of a brain-computer interface walking simulator for individuals with spinal cord injury. J Neuroeng Rehabil. 2013;10:77. | No | – Improving motor function with VR was not the study aim – No control group | |
| Kobashi N, Holper L, Scholkmann F, Kiper D, Eng K. Enhancement of motor imagery-related cortical activation during first-person observation measured by functional near-infrared spectroscopy. Eur J Neurosci. 2012;35(9):1513–21. | No | Improving motor function with VR was not the study aim | |
| Kwon JS, Park MJ, Yoon IJ, Park SH. Effects of virtual reality on upper extremity function and activities of daily living performance in acute stroke: a double-blind randomised clinical trial. NeuroRehabilitation. 2012;31(4):379–85. | Yes | ||
| Liepert J. Evidence-based therapies for upper extremity dysfunction. Curr Opin Neurol. 2010;23(6):678–82. | No | No VR use | |
| Ma HI, Hwang WJ, Fang JJ, Kuo JK, Wang CY, Leong IF, et al. Effects of virtual reality training on functional reaching movements in people with Parkinson's disease: a randomised controlled pilot study. Clin Rehabil. 2011;25(10):892–902. | No | Patients with Parkinson's disease | |
| Masiero S, Carraro E, Ferraro C, Gallina P, Rossi A, Rosati G. Upper limb rehabilitation robotics after stroke: a perspective from the University of Padua, Italy. J Rehabil Med. 2009;41(12):981–5. | No | Improving motor function with VR was not the study aim | |
| Mirelman A, Maidan I, Herman T, Deutsch JE, Giladi N, Hausdorff JM. Virtual reality for gait training: can it induce motor learning to enhance complex walking and reduce fall risk in patients with Parkinson's disease? J Gerontol A Biol Sci Med Sci. 2011;66(2):234–40. | No | No control group | |
| Mirelman A, Patritti BL, Bonato P, Deutsch JE. Effects of virtual reality training on gait biomechanics of individuals post-stroke. Gait Posture. 2010;31(4):433–7. | Yes | ||
| Mirelman A, Rochester L, Reelick M, Nieuwhof F, Pelosin E, Abbruzzese G, et al. V-TIME: a treadmill training program augmented by virtual reality to decrease fall risk in older adults: study design of a randomised controlled trial. BMC Neurol. 2013;13:15. | No | Elderly patients with no disease | |
| Orihuela-Espina F, Fernández del Castillo I, Palafox L, Pasaye E, Sánchez-Villavicencio I, Leder R, et al. Neural reorganisation accompanying upper limb motor rehabilitation from stroke with virtual reality-based gesture therapy. Top Stroke Rehabil. 2013;20(3):197–209. | No | Improving motor function with VR was not the study aim | |
| Park HS, Yoon JW, Kim J, Iseki K, Hallett M. Development of a VR-based treadmill control interface for gait assessment of patients with Parkinson's disease. IEEE Int Conf Rehabil Robot 2011;2011:5975463. | No | Improving motor function with VR was not the study aim | |
| Piron L, Turolla A, Agostini M, Zucconi C, Cortese F, Zampolini M, et al. Exercises for paretic upper limb after stroke: a combined virtual-reality and telemedicine approach. J Rehabil Med. 2009;41(12):1016–20. | No | Study topic: telemedicine | |
| Qiu Q, Ramirez DA, Saleh S, Fluet GG, Parikh HD, Kelly D, et al. The New Jersey Institute of Technology Robot-Assisted Virtual Rehabilitation (NJIT-RAVR) system for children with cerebral palsy: a feasibility study. J Neuroeng Rehabil. 2009;6:40. | No | Improving motor function with VR was not the study aim | |
| Rostami HR, Arastoo AA, Nejad SJ, Mahany MK, Malamiri RA, Goharpey S. Effects of modified constraint-induced movement therapy in virtual environment on upper-limb function in children with spastic hemiparetic cerebral palsy: a randomised controlled trial. NeuroRehabilitation. 2012;31(4):357–65. | No | Patients with cerebral palsy | |
| Saposnik G, Mamdani M, Bayley M, Thorpe KE, Hall J, Cohen LG, et al. Effectiveness of Virtual Reality Exercises in STroke Rehabilitation (EVREST): rationale, design, and protocol of a pilot randomised clinical trial assessing the Wii gaming system. Int J Stroke. 2010;5(1):47–51. | No | Only study design has been published; no results available | |
| Saposnik G, Teasell R, Mamdani M, Hall J, McIlroy W, Cheung D, et al. Effectiveness of virtual reality using Wii gaming technology in stroke rehabilitation: a pilot randomised clinical trial and proof of principle. Stroke. 2010;41(7):1477–84. | Yes | ||
| Sharan D, Ajeesh PS, Rameshkumar R, Mathankumar M, Paulina RJ, Manjula M. Virtual reality based therapy for post operative rehabilitation of children with cerebral palsy. Work. 2012;41 Suppl 1:3612–5. | No | Patients with cerebral palsy | |
| Shine JM, Matar E, Ward PB, Bolitho SJ, Gilat M, Pearson M, et al. Exploring the cortical and subcortical functional magnetic resonance imaging changes associated with freezing in Parkinson's disease. Brain. 2013;136 (Pt 4):1204–5. | No | No VR use | |
| Subramanian SK, Lourenço CB, Chilingaryan G, Sveistrup H, Levin MF. Arm motor recovery using a virtual reality intervention in chronic stroke: randomised control trial. Neurorehabil Neural Repair. 2013;27(1):13–23. | Yes | ||
| Tatla SK, Sauve K, Virji-Babul N, Holsti L, Butler C, Van Der Loos HFM. Evidence for outcomes of motivational rehabilitation interventions for children and adolescents with cerebral palsy: an American Academy for Cerebral Palsy and Developmental Medicine systematic review. Dev Med Child Neurol. 2013;55(7):593–601. | No | Improving motor function with VR was not the study aim | |
| Turolla A, Dam M, Ventura L, Tonin P, Agostini M, Zucconi C, et al. Virtual reality for the rehabilitation of the upper limb motor function after stroke: a prospective controlled trial. J Neuroeng Rehabil. 2013;10:85. | Yes | ||
| Voss S, Page M, Benger J. Methods for evaluating cervical range of motion in trauma settings. Scand J Trauma Resusc Emerg Med. 2012;20:50. | No | No VR use | |
| Wade E, Winstein CJ. Virtual reality and robotics for stroke rehabilitation: where do we go from here? Top Stroke Rehabil. 2011;18(6):685–700. | No | Improving motor function with VR was not the study aim | |
| Yang S, Hwang WH, Tsai YC, Liu FK, Hsieh LF, Chern JS. Improving balance skills in patients who had stroke through virtual reality treadmill training. Am J Phys Med Rehabil. 2011;90(12):969–78. | Yes | ||
| Yen CY, Lin KH, Hu MH, Wu RM, Lu TW, Lin CH. Effects of virtual reality-augmented balance training on sensory organisation and attentional demand for postural control in people with Parkinson disease: a randomised controlled trial. Phys Ther. 2011;91(6):862–74. | No | It studies patients with Parkinson's disease | |
| CINAHL | Abdollahi F, Case Lazarro ED, Listenberger M, Kenyon RV, Kovic M, Bogey R A, et al. Error augmentation enhancing arm recovery in individuals with chronic stroke: a randomised crossover design. Neurorehabil & Neural Repair. 2014;28(2):120–8. | No | It does not use VR |
| In-Chul K, Byoung-Hee L. Effects of augmented reality with functional electric stimulation on muscle strength, balance and gait of stroke patients. J Phys Ther Sci. 2012;24(8):755–62. | No | Improving motor function with VR was not the study aim | |
| Scopus | Arias P, Robles-García V, Sanmartín G, Flores J, Cudeiro J. Virtual reality as a tool for evaluation of repetitive rhythmic movements in the elderly and Parkinson's disease patients. PLoS ONE. 2012;7(1):e30021. | No | Improving motor function with VR was not the study aim |
| Barton GJ, Hawken MB, Foster RJ, Holmes G, Butler PB. The effects of virtual reality game training on trunk to pelvis coupling in a child with cerebral palsy. J Neuroeng Rehabil. 2013;10(1). | No | Case report | |
| Cho S, Ku J, Cho YK, Kim IY, Kang YJ, Jang DP, et al. Development of virtual reality proprioceptive rehabilitation system for stroke patients. Comput Methods Programs Biomed. 2014;113(1):258–65. | No | Improving motor function with VR was not the study aim | |
| Cikajlo I, Matjačić Z. The use of virtual reality-based dynamometer training to enhance selective joint torque control in a child with cerebral palsy. J Med Biol Eng. 2010;30(5):329–34. | No | Case report | |
| Cikajlo I, Rudolf M, Goljar N, Matjacic Z. Continuation of balance training for stroke subjects in home environment using virtual reality. Int J Disabil Hum Dev. 2011;10(4):317–20. | No | Study topic: home-based therapy | |
| Cikajlo I, Rudolf M, Goljar N, Burger H, Matjačić Z. Telerehabilitation using virtual reality task can improve balance in patients with stroke. Disabil Rehabil. 2012;34(1):13–8. | No | Study topic: telerehabilitation | |
| Connelly L, Jia Y, Toro ML, Stoykov ME, Kenyon RV, Kamper DG. A pneumatic glove and immersive virtual reality environment for hand rehabilitative training after stroke. IEEE Trans Neural Syst Rehabil Eng. 2010;18(5):551–9. | Yes | ||
| Dinomais M, Veaux F, Yamaguchi T, Richard P, Richard I, Nguyen S. A new virtual reality tool for unilateral cerebral palsy rehabilitation: two single-case studies. Dev Neurorehabil. 2013;16(6):418–22. | No | – No control group – Series of 2 cases | |
| Gilat M, Shine JM, Bolitho SJ, Matar E, Kamsma YPT, Naismith SL, et al. Variability of stepping during a virtual reality paradigm in Parkinson's disease patients with and without freezing of gait. PLoS ONE. 2013;8(6):e66718. | No | Improving motor function with VR was not the study aim | |
| Golomb MR, Warden SJ, Fess E, Rabin B, Yonkman J, Shirley B, et al. Maintained hand function and forearm bone health 14 months after an in-home virtual-reality videogame hand telerehabilitation intervention in an adolescent with hemiplegic cerebral palsy. J Child Neurol. 2011;26(3):389–93. | No | Study topic: telerehabilitation | |
| Holmes JD, Gu ML, Johnson AM, Jenkins ME. The effects of a home-based virtual reality rehabilitation program on balance among individuals with Parkinson's disease. Phys Occup Ther Geriatr. 2013;31(3):241–53. | No | Study topic: home-based therapy | |
| In TS, Jung KS, Lee SW, Song CH. Virtual reality reflection therapy improves motor recovery and motor function in the upper extremities of people with chronic stroke. J Phys Ther Sci. 2012;24(4):339–43. | Yes | ||
| Jannink MJA, Aznar M, de Kort AC, van de Vis W, Veltink P, van der Kooij H. Assessment of visuospatial neglect in stroke patients using virtual reality: a pilot study. Int J Rehabil Res. 2009;32(4):280–6. | No | Improving motor function with VR was not the study aim | |
| Jo K, Yu J, Jung J. Effects of virtual reality-based rehabilitation on upper extremity function and visual perception in stroke patients: a randomised control trial. J Phys Ther Sci. 2012;24(11):1205–8. | Yes | ||
| Jung J, Yu J, Kang H. Effects of virtual reality treadmill training on balance and balance self-efficacy in stroke patients with a history of falling. J Phys Ther Sci. 2012;24(11):1133–6. | Yes | ||
| Kott K, Lesher K, DeLeo G. Combining a virtual reality system with treadmill training for children with cerebral palsy. J Cyber Ther Rehabil. 2009;2(1):35–42. | No | There is no control group | |
| Laver K, George S, Ratcliffe J, Crotty M. Virtual reality stroke rehabilitation – hype or hope? Aust Occup Ther J. 2011;58(3):215–9. | No | Improving motor function with VR was not the study aim | |
| Lee SJ, Chun MH. Combination transcranial direct current stimulation and virtual reality therapy for upper extremity training in patients with subacute stroke. Arch Phys Med Rehabil. 2014;95(3):431–8. | Yes | ||
| Lewis GN, Woods C, Rosie JA, Mcpherson KM. Virtual reality games for rehabilitation of people with stroke: perspectives from the users. Disabil Rehabil Assist Technol. 2011;6(5):453–63. | No | – Improving motor function with VR was not the study aim – No control group | |
| Li W, Lam-Damji S, Chau T, Fehlings D. The development of a home-based virtual reality therapy system to promote upper extremity movement for children with hemiplegic cerebral palsy. Technol Disabil. 2009;21(3):107–13. | No | Study topic: home-based therapy | |
| Matar E, Shine JM, Naismith SL, Lewis SJG. Using virtual reality to explore the role of conflict resolution and environmental salience in Freezing of Gait in Parkinson's disease. Parkinsonism Relat Disord. 2013;19(11):937–42. | No | Improving motor function with VR was not the study aim | |
| Metin-Ökmen B, Do¿an-Aslan M, Çuhadaro¿lu-Çetin F, Nakipo¿lu-Yüzer GF, Köse-Dönmez B, Özgirgin N. The effect of virtual reality therapy on psychological adaptation in children with cerebral palsy. Noropsikiyatri Arsivi. 2013;50(1):70–4. | No | Improving motor function with VR was not the study aim | |
| Mirelman A, Bonato P, Deutsch JE. Effects of training with a robot-virtual reality system compared with a robot alone on the gait of individuals after stroke. Stroke. 2009;40(1):169–74. | Yes | ||
| Mitchell L, Ziviani J, Oftedal S, Boyd R. The effect of virtual reality interventions on physical activity in children and adolescents with early brain injuries including cerebral palsy. Dev Med Child Neurol. 2012;54(7):667–71. | No | There is no control group | |
| Robles-García V, Arias P, Sanmartín G, Espinosa N, Flores J, Grieve KL, et al. Motor facilitation during real-time movement imitation in Parkinson's disease: a virtual reality study. Parkinsonism Relat Disord. 2013;19(12):1123–9. | No | Improving motor function with VR was not the study aim | |
| Saleh S, Bagce H, Qiu Q, Fluet G, Merians A, Adamovich S, et al. Mechanisms of neural reorganisation in chronic stroke subjects after virtual reality training. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:8118–21. | No | Conference | |
| Sampson M, Shau YW, James-King M. Bilateral upper limb trainer with virtual reality for post-stroke rehabilitation: case series report. Disabil Rehabil Assist Technol. 2012;7(1):55–62. | No | – No control group – Case series | |
| Shine JM, Matar E, Bolitho SJ, Dilda V, Morris TR, Naismith SL, et al. Modeling freezing of gait in Parkinson's disease with a virtual reality paradigm. Gait Posture. 2013;38(1):104–8. | No | No control group | |
| Shiri S, Feintuch U, Lorber-Haddad A, Moreh E, Twito D, Tuchner-Arieli M, et al. Novel virtual reality system integrating online self-face viewing and mirror visual feedback for stroke rehabilitation: rationale and feasibility. Top Stroke Rehabil. 2012;19(4):277–86. | No | – Improving motor function with VR was not the study aim – No control group | |
| Singh DKA, Mohd-Nordin NA, Aziz NAA, Lim BK, Soh LC. Effects of substituting a portion of standard physiotherapy time with virtual reality games among community-dwelling stroke survivors. BMC Neurol. 2013;13:199. | Yes | ||
| Standen PJ, Brown DJ, Battersby S, Walker M, Connell L, Richardson A, et al. A study to evaluate a low cost virtual reality system for home based rehabilitation of the upper limb following stroke. Int J Disabil Hum Dev. 2011;10(4):337–41. | No | Study topic: home-based therapy | |
| Sung WH, Chiu TY, Tsai WW, Cheng H, Chen JJ. The effect of virtual reality-enhanced driving protocol in patients following spinal cord injury. J Chin Med Assoc. 2012;75(11):600–5. | No | Improving motor function with VR was not the study aim | |
| Trobia J, Gaggioli A, Antonietti A. Combined use of music and virtual reality to support mental practice in stroke rehabilitation. J Cyber Ther Rehabil. 2011;4(1):57–61. | No | Improving motor function with VR was not the study aim | |
| Trotti C, Menegoni F, Baudo S, Bigoni M, Galli M, Mauro A. Virtual reality for the upper limb motor training in stroke: a case report. J Cyber Ther Rehabil. 2009;7(1):257–60. | No | Case report | |
| Tsoupikova D, Stoykov N, Kamper D, Vick R. Virtual reality environment assisting post stroke hand rehabilitation: case report. Stud Health Technol Inform. 2013;184:458–64. | No | Case report | |
| Villiger M, Bohli D, Kiper D, Pyk P, Spillmann J, Meilick B, et al. Virtual reality-augmented neurorehabilitation improves motor function and reduces neuropathic pain in patients with incomplete spinal cord injury. Neurorehabil Neural Repair. 2013;27(8):675–83. | No | Improving motor function with VR was not the study aim | |
| Wang CY, Hwang WJ, Fang JJ, Sheu CF, Leong IF, Ma HI. Comparison of virtual reality versus physical reality on movement characteristics of persons with Parkinson's disease: effects of moving targets. Arch Phys Med Rehabil. 2011;92(8):1238–45. | No | Patients with Parkinson's disease | |
| Wang M, Reid D. Virtual reality in pediatric neurorehabilitation: attention deficit hyperactivity disorder, autism and cerebral palsy. Neuroepidemiology. 2011;36(1):2–18. | No | Improving motor function with VR was not the study aim | |
| ISI Web of Science (WOS) | Deutsch JE. Using virtual reality to improve walking post-stroke: translation to individuals with diabetes. J Diabetes Sci Technol. 2011;5(2):309–14. | No | Patients with diabetes |
| Lucca LF. Virtual reality and motor rehabilitation of the upper limb after stroke: a generation of progress? J Rehabil Med. 2009;41(12):1003–6. | No | Improving motor function with VR was not the study aim | |
| Wang M, Reid D. Virtual reality in pediatric neurorehabilitation: attention deficit hyperactivity disorder, autism and cerebral palsy. Neuroepidemiology. 2011;36(1):2–18. | No | Improving motor function with VR was not the study aim | |
| SPORTDiscus | Brien M, Sveistrup H. Poster 131: an intensive virtual reality program improves balance and functional mobility of adolescents with cerebral palsy. Arch Phys Med Rehabil. 2010;91(10):e45. | No | Oral presentation at a congress |
| Golomb MR, McDonald BC, Warden SJ, Yonkman J, Saykin AJ, Shirley B, et al. In-home virtual reality videogame telerehabilitation in adolescents with hemiplegic cerebral palsy. Arch Phys Med Rehabil. 2010;91(1):1–8. | No | Study topic: telerehabilitation | |
| HyeonHui S, GyuChang L. Additional virtual reality training using Xbox Kinect in stroke survivors with hemiplegia. Am J Phys Med Rehabil. 2013;92(10):871–80. | Yes | ||
| Jinhwa J, Jaeho Y, Hyungkyu K. Effects of virtual reality treadmill training on balance and balance self-efficacy in stroke patients with a history of falling. J Phys Ther Sci. 2012;24(11):1133–6. | No | Improving motor function with VR was not the study aim | |
| Navarro MD, Lloréns R, Noé E, Ferri J, Alcañiz M. Validation of a low-cost virtual reality system for training street-crossing. A comparative study in healthy, neglected and non-neglected stroke individuals. Neuropsychol Rehabil. 2013;23(4):597–618. | No | Study topic: validation of a VR system | |
In each article the variables and information analysed were: type of study, research goals, the number of subjects, therapy used, VR system used, treatment duration, variables and tests/scales used, results, levels of evidence, and grade of recommendation.
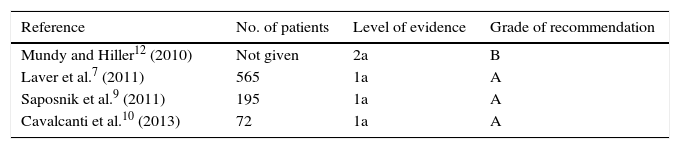
The level of evidence and grade of recommendation of each of the selected studies were analysed using the classification proposed by the Oxford Centre for Evidence-Based Medicine.21
ResultsSystematic reviewsIn Australia, Mundy and Hiller12 published a government report on the use of VR to improve motor function in stroke patients. These authors concluded that VR is a promising tool, since it is becoming less costly, treats patients more intensively, and does not require constant supervision by a therapist.
Laver et al.7 analysed the effects of VR and interactive video games on upper limb (UL) and lower limb (LL) function (balance and gait), and global motor function in patients with chronic stroke. They also analysed the effects of VR on cognitive function, quality of life, and presence of adverse effects. The authors included 19 studies consisting of a total of 565 participants. Seven studies assessed improvements in UL motor function, 3 studies analysed improvements in gait, 3 analysed performance of activities of daily living (ADL: taking a shower, getting dressed, etc.), and the remaining 6 assessed cognitive function, quality of life, and possible adverse effects. The authors concluded that VR improves UL motor function as well as performance of ADL. No statistically significant results were obtained for the remaining study variables. None of these studies described any adverse effects.
Saposnik et al.9 conducted a meta-analysis to determine the effects of VR on UL motor function in stroke patients. They analysed 12 studies (5 RCT and 7 observational studies with a pre-/post-intervention design) including 195 participants in total. The authors determined that VR improves UL motor function (positive results found in 11 of the studies included in the meta-analysis). However, as these authors highlighted, the outcome measures used vary greatly, the number of studies is limited, and there are very few studies assessing quality of life, motivation-participation, and ADL performance, which may lead to biased results.
Cavalcanti et al.10 conducted an SR to determine whether VR improved gait in stroke patients. The authors included 4 studies with a total of 72 participants. Their results showed that VR improves gait to a greater extent than conventional therapy, no therapy, or VR combined with other types of intervention.
Despite the favorable results reported by the analysed SR,7,9,10,12 the authors were cautious in drawing their conclusions since these studies do not provide sufficient scientific evidence.7,9,10,12 We need studies with larger sample sizes, conducted over longer periods, and that analyse whether VR changes cortical reorganisation in order to establish the benefits and potential risks of using this therapeutic resource. Furthermore, identifying the patients who would benefit the most from this therapy would be of great interest.7,12
According to the Oxford Centre For Evidence-Based Medicine classification,21 3 of the SR have level of evidence ‘1a’ and grade of recommendation ‘A’ (Table 3).
Randomised and/or controlled clinical trialsThis section is structured according to the defined objectives.
Virtual reality devices/systems used in neurological diseasesAll the analysed studies used semi-immersive or non-immersive VR systems,22–42 and only 2 of them used low-cost devices to create VR environments.26,38
Motor symptoms most frequently treated with virtual reality in stroke patients. Effects and benefits of virtual realityThe studies on VR for therapeutic purposes are aimed at improving UL motor function, performance of ADL, LL motor function and/or gait, as well as static and dynamic balance. In 10 of the analysed studies, VR was used for patients with chronic stroke (>6 months from diagnosis of stroke).7,22–24,30,32,35–37,40
Fourteen of the analysed studies used VR to improve UL motor function.23,25,26,29,31–35,38–42 Of these, only 3 analysed performance of ADL,33,39,41 4 used VR to improve LL motor function and/or gait,22,24,27,37 and 5 used VR to improve static and/or dynamic balance.22,28,30,36,37 We will now describe the most relevant studies.
Most of the studies using VR to improve UL motor function included 2 subject groups: one group where VR was applied alone or combined with conventional therapy, and another group treated exclusively with conventional therapy.23,25,26,29,31,33,34,38–41 Only one of the studies included a placebo group,32 and 2 studies included 3 patient groups and 3 different types of stimulation.35,42
In most of the studies, the group treated with VR experienced an improvement in UL motor function which was measured with different tests including the Wolf Motor Function test, the Fugl-Meyer test, the Chedoke Arm and Hand Activity Inventory, the Motricity Index, the modified Barthel index, the Functional Independence Measure, and the Manual Function test. However, studies by Connelly et al.,25 Kwon et al.,33 Crosbie et al.,34 HyeonHui and GyuChang,38 and Singh et al.39 found no statistically significant differences between groups.
We should highlight that the analysed studies use different sample sizes and types of VR (splints/orthoses to perform functional activities,23,25 computer devices and software to stimulate and guide subjects in performing tasks with UL,29,31,32,34,35,39–42 and low-cost videogames26,38).
Most of the analysed studies applied the same treatment intensity (number of sessions per week, session duration, weeks of treatment) in all groups,23,25,26,29,32,34,35,39–42 with the exception of 3 studies, in which the study group received a more intensive treatment (greater number of sessions and longer session duration).31,33,38
The 4 studies that used VR to improve LL motor function and/or gait included 2 subject groups; one group used VR alone or combined with another therapy, whereas the control group used conventional or alternative therapy and no VR.22,24,27,37
Both groups in all studies were treated with the same intensity (number of sessions per week, session duration, weeks of treatment). The VR groups showed statistically significant improvements in gait and UL motor function22,24,27,37 (measured with the 10-minute walk test; the kinematic gait parameters ‘cadence’, ‘velocity’, and ‘walked distance’; joint range of motion; and the Modified Motor Assessment). Two of these studies also assessed the effect of VR on balance,22,37 and both found improvements in this parameter (using the Berg Balance Scale and the Timed Up and Go test).
In addition to the studies by Kim et al.22 and Cho and Lee,37 other authors have used VR to improve static and/or dynamic balance.28,30,36 All these studies included 2 subject groups, one of which received VR while the other did not. In 2 of these studies, balance was trained using a treadmill.28,30
All studies found statistically significant differences between groups. In general, patients in the VR groups experienced improvements in dynamic balance28,30,36 (measured with computerised dynamic posturography, the Berg Balance Scale and the Timed Up and Go test). Patients’ static balance, however, was shown to improve only in the study by Jung et al.30 (using computerised dynamic posturography).
We should point out that all the studies used the same treatment intensity in all groups, except for the study by Cho et al.;36 in this study, the participants included in the experimental group received a more intense treatment (greater number of sessions and longer session duration), which may have biased their results.
According to the Oxford Centre For Evidence-Based Medicine classification,21 most of the clinical trials analysed had a level of evidence ‘1a’ and grade of recommendation ‘A’ (Table 4).
Summary of results obtained in the controlled and/or randomised clinical trials included in our review.
| Reference | Type of study | No. of patients | Therapy | Therapy duration | Study variables, and scales and tests | Results | Level of evidence Grade of recommendation |
|---|---|---|---|---|---|---|---|
| Kim et al.22 (2009) | RCT (double-blind: patients and rater) | 24 | SG (12 patients): conventional therapy+VR CG (12 patients): conventional therapy only | 4 weeks (4 sessions/week; 40min). SG: 40min of conventional therapy+30min of VR CG: 40min of conventional therapy | Assessment at the beginning and end of the intervention: – Balance (computerised dynamic posturography and Berg Balance Scale) – Gait (10-min walk test: kinematic variables; and Modified Motor Assessment scale) | – Statistically significant differences between groups; greater improvements in balance in the SG (higher scores on the Berg Balance Scale and dynamic balance test) – The SG shows statistically significant improvements in cadence, step length, step time, velocity, and Modified Motor Assessment Scale scores – Dynamic balance improvement was positively correlated with velocity and cadence | 1b-A |
| Housman et al.23 (2009) | RCT | 28 | SG (14 patients): therapy using T-WREX (UL orthosis) CG (14 patients): performance of conventional semiautonomous training | 12 weeks (2 sessions/week; 1h) | Assessment at the beginning and end of the intervention, and 6 months later: – UL motor function (Fugl-Meyer test) – UL range of motion – Amount of UL use (Motor Activity Log test) | – Significant improvement in both groups at the end of the intervention and at 6 months after the intervention in all tests – Statically significant differences between groups regarding Fugl-Meyer test scores (higher scores in the SG) This difference between groups remained after 6 months. | 1b-A |
| Mirelman et al.24 (2009) | RCT (single-blind) | 18 | SG (9 patients): robotic device in LL+VR CG (9 patients): only robotic device in LL | 4 weeks (3 sessions/week; 1h) | Assessment at the beginning and end of the intervention, and 3 months later: – Gait kinematic variables (no. of steps, velocity, walked distance) in both clinical and community settings | – The SG showed greater improvements in velocity and walked distance. This difference between groups remained after 3 months. | 1b-A |
| Connelly et al.25 (2010) | CAT | 14 | SG (7 patients): patients handled real and virtual objects using the PneuGlove pneumatic glove CG (7 patients): no PneuGlove; patients handled real objects | 6 weeks (3 sessions/week; 90min) | Assessment at the beginning and end of the intervention: – Motor function of the paretic UL (Fugl-Meyer test) – Motor function of the paretic hand and wrist (Fugl-Meyer test) – Hand dexterity of the paretic UL (Box and Block test) – Palmar pitch strength (dynamometer) | – There were significant improvements in the 4 variables analysed, and these were slightly more significant in the SG – No statistically significant differences between groups | 2b-B |
| Saposnik et al.26 (2010) | RCT (single-blind: rater) | 17 | SG (9 patients): VR therapy CG (8 patients): recreational therapy (playing cards, bingo, etc.) | 2 weeks (4 sessions/week; 1h) | Assessment at the beginning and end of the intervention and 4 weeks after the intervention: – Feasibility of Wii gaming system (time receiving the intervention) – Safety of Wii gaming system (intervention-related adverse effects) – UL motor function (Wolf Motor Function test) – Manual dexterity (Box and Block test) – Quality of life (Stroke Impact Scale) | – No adverse events – SG scores were statistically significantly higher than CG scores on the Wolf Motor Function Test | 1b-A |
| Mirelman et al.27 (2010) | RCT (single-blind: rater) | 18 | SG (9 patients): VR gait training CG (9 patients): gait training with conventional therapy only | 4 weeks (3 sessions/week; 1h) | Assessment at the beginning and end of the intervention: – Gait kinematic variables (cadence, velocity, walked distance) – Gait kinetic variables (range of motion of hip, knees, and ankles) | – Statistically significant differences between groups in knee and ankle ranges of motion, with greater changes in the SG | 1b-A |
| Yang et al.28 (2011) | RCT | 14 | SG (7 patients): balance training with treadmill+VR CG (7 patients): balance training with treadmill only | 3 weeks (3 sessions/week; 40min) | Assessment at the beginning and end of the intervention: – Static and dynamic balance (computed dynamic posturography platform) – No. of steps of the paretic LL – Contact area of the paretic foot during quiet stance – Contact area of the paretic foot during sit-to-stand transfer – Contact area of the paretic foot during level walking | – Training had no positive effect on static balance – Statistically significant differences between groups, with improvements in dynamic balance in the SG (center of gravity displacements) during gait and sit-to-stand transfers. Contact area of the paretic foot during gait and transfer also improved in this group. | 1b-A |
| Da Silva Cameirao et al.29 (2011) | RCT | 16 | SG (8 patients): conventional therapy+VR CG (8 patients): conventional therapy+interactive games | 12 weeks (3 sessions/week; 40min) SG: 40min of conventional therapy+30min of VR SG: 40min of conventional therapy+30min of interactive games | Assessment at the beginning and end of the intervention: – Motor function of the affected UL (Fugl-Meyer test, Chedoke Arm and Hand Activity Inventory) | – Statistically significant differences between groups, with the SG showing more pronounced improvements in the affected UL and higher scores on the Fugl-Meyer test and the Chedoke Arm and Hand Activity Inventory – Significantly faster improvement during the treatment period for SG regarding all the clinical scales | 1b-A |
| Jung et al.30 (2012) | CAT | 21 | SG (11 patients): gait training with treadmill+VR CG (10 patients): gait training with treadmill only | 3 weeks (3 sessions/week; 1h) | Assessment at the beginning and end of the intervention: – Static and dynamic balance assessment (computed dynamic posturography equipment) | – Static and dynamic balance significantly improved in both groups – Significant differences between groups, with greater improvements in static and dynamic balance in the SG | 1b-A |
| Jo et al.31 (2012) | RCT | 29 | SG (15 patients): UL rehabilitation with VR CG (14 patients): UL rehabilitation with conventional therapy | 4 weeks SG: 60min of therapy, 5 sessions/week CG: 30min of therapy, 3 sessions/week | Assessment at the beginning and end of the intervention: – UL motor function (Wolf Motor Function Test) – Visual perception (Motor-Free Visual Perception Test) | – Scores in both tests improved significantly in both groups – Statistically significant differences between groups; the SG achieved higher scores on the Motor-Free Visual Perception Test | 1b-A |
| In et al.32 (2012) | RCT | 19 | SG (11 patients): conventional therapy+VR CG (8 patients): conventional therapy+VR-simulating treatment (placebo) | 4 weeks (5 sessions/week) SG: 30min of VR therapy CG: 30min of simulated VR therapy (placebo). | Assessment at the beginning and end of the intervention: – Muscle tone (Modified Ashworth Scale) – UL motor function (Fugl-Meyer test) – Manual dexterity (Box and Block Test) – Jebsen-Taylor Hand Function and the Manual Function tests | – Scores on all tests improved significantly in both groups – Significant differences between groups; improvements in motor recovery and motor function were more marked in the SG | 1b-A |
| Kwon et al.33 (2012) | RCT | 26 | SG (13 patients): conventional therapy+VR CG (13 patients): conventional therapy only | 3 weeks (3 sessions/week) SG: 1.5h per session CG: 1h per session | Assessment at the beginning and end of the intervention: – UL motor function (Fugl-Meyer test, Manual Function Test) – Performance of ADL (modified Barthel Index) | – The SG showed statistically significant improvements in the scores on the 3 tests. However, the CG showed no statistically significant improvements in Manual Function Test scores – There were no statistically significant differences in scores between groups on the 3 tests | 1b-A |
| Crosbie et al.34 (2012) | RCT | 18 | SG (9 patients): use of VR CC (9 patients): conventional therapy only | 3 weeks (3 sessions/week; 1h) | Assessment at the beginning and end of the intervention, and 6 weeks later: – UL motor function (Motricity Index and Action Research Arm Test) | – There were no statistically significant differences in scores on the Motricity Index and the Action Research Arm tests between groups | 1b-A |
| Cameirao et al.35 (2012) | RCT | 44 | SG1 (15 patients): training of the affected UL with VR (visual stimuli) SG2 (15 patients): training of the affected UL with VR (haptic stimuli) CG (14 patients): training of the affected UL with VR (passive exoskeleton) | 5 weeks (5 sessions/week; 35min) | Assessment at the beginning and end of the intervention: – UL motor function (Fugl-Meyer Test, Manual Function Test) – Performance on ADL (modified Barthel Index) | – The 3 groups showed statistically significant improvements in the scores of the 3 study variables – There were statistically significant differences between groups, with higher scores in SG1 and SG2 | 1b-A |
| Cho et al.36 (2012) | RCT | 22 | SG: (11 patients): conventional therapy+VR CC (11 patients): conventional therapy only | 6 weeks (5 sessions/week; 1h) Note: the SG has trained with VR in sessions of 30min, 3 sessions/week for 6 weeks. | Assessment at the beginning and end of the intervention: – Assessment of static balance with eyes open and closed (computed dynamic posturography) – Assessment of dynamic balance (Berg Balance Scale and Timed Up and Go test) | – No significant improvements in static balance in any group – There were statistically significant differences between groups in dynamic balance; the SG achieved higher scores on the Berg Balance Scale and Timed Up and Go test | 2b-B |
| Cho et al.37 (2013) | RCT | 14 | SG (7 patients): conventional therapy+treadmill gait training with VR projection (real-world video recording during gait) SG (7 patients): conventional therapy+treadmill gait training without VR projection | – Conventional therapy was applied for 6 weeks (3 sessions/week; 45min) – Treadmill therapy with and without VR was applied for 6 weeks (3 sessions/week; 30min) | Assessment at the beginning and end of the intervention: – Dynamic balance (Berg Balance Scale and Timed Up and Go test) – Gait kinetic variables (parameters obtained with the treadmill) | – Statistically significant improvements in the study variables in both groups – Statistically significant differences between groups in dynamic balance, cadence, and gait velocity; the SG displayed higher scores | 1b-A |
| HyeonHui and GyuChang38 (2013) | RCT | 40 | SG (20 patients): VR using Xbox Kinect+conventional occupational therapy CG (20 patients): conventional occupational therapy only | 6 weeks (3 sessions/week) SG: 90min per session CG: 45min per session | Assessment at the beginning and end of the intervention: – Range of motion of the affected UL – Motor function of the affected UL (Fugl-Meyer Test) – Hand dexterity of the paretic UL (Box and Block Test) | – The 3 analysed variables improved significantly in both groups; improvements were slightly greater in the SG – No significant differences between groups | 1b-A |
| Singh et al.39 (2013) | CAT | 28 | SG (14 patients): conventional therapy+VR CC (14 patients): conventional physiotherapy only | 6 weeks (2 sessions/week; 2h) SG: 90min of conventional physiotherapy+30min of VR CG: 120min of conventional physiotherapy | Assessment at the beginning and end of the intervention: – Gait (Timed Up and Go test, 30-econd Sit-to-Stand test, Timed Ten-Metre Walk test, and Six-Minute Walk Test) – ADL (modified Barthel Index) – Assessment of static balance using the Wii balance board | – Scores on the Timed Up and Go and 30-Second Sit-to-Stand tests improved significantly in both groups – No statistically significant differences between groups were observed in the study variables | 1b-A |
| Subramanian et al.40 (2013) | RCT | 32 | SG (16 patients): VR therapy CG: (16 patients): therapy in a conventional physical environment | 4 weeks (3 sessions/week; 1h) | Assessment at the beginning and end of the intervention: – UL kinematic variables (digital goniometric measurement) – Range of motion of the UL (digital goniometric measurement) – UL impairment (mild, moderate, severe) | – All variables showed statistically significant improvements in both groups after the intervention – Statically significant differences between groups in shoulder horizontal adduction and flexion (greater improvements in the SG) | 1b-A |
| Turolla et al.41 (2013) | CAT | 376 | SG (188 patients): conventional therapy+VR CG (188 patients): conventional therapy only | 4 weeks (5 sessions/week; 2h) | Assessment at the beginning and end of the intervention: – UL motor function (Fugl-Meyer Test) – UL functionality (Functional Independence Measure scale) | – Statistically significant improvements in the 2 study variables in both groups – Statistically significant differences between groups: greater improvements in motor function and UL functionality in the SG | 1b-A |
| Lee and Chun42 (2014) | RCT | 59 | Group A (20 patients): cathodal transcranial stimulation Group B (20 patients): VR therapy Group C (19 patients): cathodal transcranial stimulation+VR therapy | 3 weeks (5 sessions/week; 1h) | Assessment at the beginning and end of the intervention: – Assessment of muscles (Manual Muscle Test) – Hand function (Manual Function Test) – Motor function of the affected UL (Fugl-Meyer Test) – Assessment of ADL performance (modified Barthel Index) | – The 4 variables analysed showed statistically significant improvements in the 3 groups – Statistically significant differences between groups, with group C showing higher scores on the Manual Muscle and Manual Function tests | 1b-A |
ADL: activities of daily living; RCT: randomised controlled trial; CCT: controlled clinical trial; CG: control group; SG: study group; LL: lower limb(s); UL: upper limb(s); no.: number; VR: virtual reality.
In addition to the VR systems specifically designed for therapeutic purposes,5 there is currently a wide variety of low-cost commercial video games which represent an alternative way to generate virtual environments that may be used in clinical settings. Only 2 studies out of all the analysed clinical trials used low-cost devices or systems to generate VR environments.26,38 As might be expected, over the next few years these devices will be increasingly used as this technology becomes more accessible and less expensive, and more results will be published as a consequence.
Based on the studies in hand, we can conclude that currently we have solid scientific evidence on the beneficial effects of VR for motor rehabilitation after stroke,7,9,10,22–42 particularly in regards to UL motor function improvement.23,25,26,29,31–35,38–42
The analysed studies show differences in treatment duration (ranging from 2 to 12 weeks23–29; mean treatment duration in most of the studies was 4–6 weeks24,25,31,32,38,40) and intensity (VR session duration ranged from 30min32 to 1.5h25). Likewise, few studies evaluated whether VR effects endured long term as they did not follow up patients after therapy.23,24,26,34,35
Most of the studies had small sample sizes, with the exception of the study by Turolla et al.,41 which analysed a sample of 376 stroke patients.
Much remains to be understood about the impact of VR systems on motor rehabilitation. Furthermore, we do not know precisely which characteristics of these systems are essential for obtaining beneficial effects. We need more studies similar to that by Orihuela-Espina et al.43 to better understand the physiological basis of why and how VR systems improve motor function in certain neurological diseases. In this particular study, the authors tried to quantify the neuronal changes underlying the motor improvements achieved thanks to imitation therapy (conducted with VR), and concluded that activity generated in the prefrontal cortex and cerebellum was responsible for motor rehabilitation in this type of treatment.
It is important to identify the most suitable interface to be used in any particular VR system in order to maximise motor improvements. For example, the study by Cameirão et al.35 compared 3 types of interfaces (vision-based tracking, haptics, and a passive exoskeleton) to determine which one was the most effective. Further studies using different interfaces are needed in order to reach a more definitive conclusion.
We also need more studies on whether motor function improvements are caused by the VR system itself or are a consequence of the characteristics of the task trained and the participation-motivation of users. Studies including a placebo group should be conducted to evaluate this issue. Of all the analysed studies, only one includes a placebo group.32 This study found no functional improvement in the placebo group, leading to the deduction that the improvements detected in the other group are due to the use of VR.
At this point we may hypothesise as to why VR is a valuable adjuvant or alternative therapy to conventional treatment of motor function in stroke patients. To answer this question, we should first consider the 4 key elements for optimal functional recovery in this type of patient: motor learning, high intensity (repetition), positive feedback (stimulus-response), and patients’ motivation.18 According to recent studies, changes in the neuronal architecture must take place for motor learning and relearning to occur. Therefore, therapy should be based on the long term repetition of functional activities and rewards should be used to encourage patients.19,20 VR therapies can be designed to meet these characteristics. Furthermore, VR creates individualised treatment environments by manipulating and regulating user's interaction with the environment.44 These systems are usually attractive, motivating, easy to use, and safe. They are becoming more affordable and are capable of analysing if tasks are performed correctly.19,20
Conclusions- -
Today, semi-immersive and non-immersive VR systems are the most widely used VR systems in the management of motor symptoms of stroke patients.
- -
Stroke is the neurological disease most frequently treated with therapeutic VR. Clinical trials and SR published to date offer compelling scientific evidence on the benefits of VR for UL motor function in these patients.
- -
The neurological symptoms most frequently treated with VR in stroke patients are UL motor function, LL motor function and gait, and static and dynamic balance.
- -
The studies included in our review show optimal levels of evidence and grades of recommendation, but further studies with larger sample sizes are needed to draw more reliable and robust conclusions.
- -
We need more studies focused on resolving whether VR changes cortical reorganisation, determining if VR results are sustained in the long term, identifying the most suitable type of VR system, and defining the most appropriate treatment frequency and intensity.
This study has received no private or public funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Viñas-Diz S, Sobrido-Prieto M. Realidad virtual con fines terapéuticos en pacientes con ictus: revisión sistemática. Neurología. 2016;31:255–277.
This study has not been presented at any national or international congress nor has it been published in any Spanish or international journal.