Population ageing, the rising demand for healthcare, and the establishment of acute stroke treatment programs have given rise to increases in the number and complexity of neurological emergency cases. Nevertheless, many centres in Spain still lack on-call emergency neurologists.
MethodsWe conducted a retrospective study to describe the role of on-call neurologists at Hospital General Universitario Gregorio Marañón, a tertiary care centre in Madrid, Spain. Sociodemographic characteristics, most common pathologies, diagnostic tests, and destination of the patients attended were recorded daily using a computer database. Results were compared with the general care data from the emergency department.
ResultsThe team attended 3234 patients (3.48% of the emergency department total). The mean number of patients attended per day was 11.15. The most frequent pathologies were stroke (34%), epilepsy (16%) and headache (8%). The mean stay in the emergency department was 7.17hours. Hospital admission rate was 40% (7.38% of emergency hospital admissions). The main destinations for admitted patients were the stroke unit (39.5%) and the neurology department (33%). Endovascular or thrombolytic therapies were performed on 76 occasions. Doctors attended 70% of the patients during on-call hours.
ConclusionsEmergency neurological care is varied, complex, and frequently necessary. Neurological cases account for a sizeable percentage of both patient visits to the emergency room and the total number of emergency admissions. The current data confirm that on-call neurologists available on a 24-hour basis are needed in emergency departments.
El envejecimiento poblacional, el aumento en la demanda asistencial y la instauración de tratamientos avanzados para el ictus agudo han originado que las urgencias neurológicas crezcan en número y complejidad. A pesar de esto, muchos centros hospitalarios de España carecen de guardias específicas de Neurología.
MétodosEstudio prospectivo durante un año (agosto 2010-julio 2011), que describe la labor asistencial del equipo de guardia de Neurología del Hospital terciario Gregorio Marañón de Madrid. Se recogieron las características sociodemográficas, las principales afecciones, las pruebas diagnósticas y el flujo de los pacientes atendidos, utilizando un registro diario mediante una base de datos informatizada. Los resultados fueron comparados con la asistencia médica general en urgencias.
ResultadosSe atendió a 3.234 pacientes (3.48% del total de urgencias médicas), con una media de 11.15 pacientes/día. La edad media fue de 59 años. Las enfermedades más frecuentes fueron la cerebrovascular (34%), epilepsia (16%) y cefalea (8%). La estancia media en urgencias fue de 7.17 h. La tasa de ingreso hospitalario fue del 40% (7.38% del total de ingresos urgentes por afección médica). Los principales destinos de los pacientes hospitalizados fueron Unidad de Ictus (39.5%) y la planta de Neurología (33%). Se realizaron 76 procedimientos trombolíticos o intravasculares en ictus agudos. El 70% de los pacientes fue valorado fuera del horario laboral.
ConclusionesLa atención neurológica es frecuente, variada y compleja, representando un alto porcentaje sobre el total de paciente atendidos o ingresados en urgencias. Nuestros resultados justifican la presencia física de un neurólogo de guardia 24h en urgencias.
Care for neurological patients in emergency departments is attracting growing interest.1–5 The rising demand for neurological care, population ageing, new developments in neuroimaging scans, and the implementation of advanced treatments for acute stroke have resulted in increases in the number and complexity of neurological emergency cases. On-call neurology teams available on a 24-hour basis in hospital emergency departments are becoming increasingly necessary.1,6,7 This situation, associated with the substantial societal and healthcare impact of neurological disorders, has led to a significant rise in the number of positions available for neurology specialists and neurology residents (120 positions in the 2012 round of hiring).6,8,9 An on-call neurologist has also been proved to deliver better quality care and appropriate patient referrals, reduce unnecessary hospital admissions, and promote the neurology department.10–12 Despite the above, many Spanish hospitals still do not have an on-call neurologist for emergency patients; in the Region of Madrid, for example, there are only 6 hospitals in which neurologists work 24-hour on-call shifts and directly supervise the neurology resident.13
This one-year prospective study aims to describe the workload of on-call emergency room neurologists in Madrid at Hospital General Universitario Gregorio Marañón (HGUGM).
Materials and methodsHGUGM is a public hospital in the Madrid healthcare area; it has 1671 beds and serves a population of 317940 inhabitants.14 It is the centre of reference for specialist care in former Health District 1 in the Region of Madrid (792972 inhabitants) and its stroke unit provides care to a total of 1043972 inhabitants.14,15
At HGUGM, the medical emergency department consists of the outpatient area, observation area, high dependency unit (HDU), and accident and emergency cubicles. Patients are referred to one area or another based on the clinical priority assigned according to the Manchester Triage System.16 The HDU is an intermediate care unit with 10 beds, managed by the internal medicine department and available to other medical specialties. It provides structural support (continuous monitoring and non-invasive mechanical ventilation) to patients of intermediate severity not requiring intensive care.
The internal medicine team is the first to assess patients with non-surgical conditions, except under certain circumstances: patients with suspected cerebrovascular disease and covered by the consensus protocol for acute stroke care (Madrid stroke care plan, 2009) are referred directly to the neurology department. This is also the case for patients transferred from hospitals without on-call neurologists to undergo an emergency neurological evaluation, and in cases of exacerbation of previously diagnosed neurological diseases.15 Patients with suspected acute neurological disease are also assessed by the neurology department at the request of internal medicine or other departments. The on-call neurology team consists of a neurologist and a neurology resident, available on site 24hours a day, 365 days a year.
We conducted a prospective longitudinal observational study to describe our work in emergency units and included all patients assessed by on-call neurology teams between 1 August 2010 and 31 July 2011. We excluded consultations resolved by telephone and visits to patients already admitted to the neurology department, which comprises the neurology ward (28 admission beds), stroke unit (6 admission beds) and neurological patients admitted to other wards. We recorded a detailed clinical history for every patient and in the case of stroke patients, we used a pro-forma.17 The analysis included sociodemographic characteristics (age, sex, nationality), clinical characteristics (type of disease), diagnostic features (computed tomography [CT], CT angiography [CT-angio], magnetic resonance imaging, lumbar puncture, electroencephalogram, and neurosonology study), patient flow (times, requesting department, attending department, final referral) and miscellanea (‘code stroke’, thrombolysis, pregnancy, return to the emergency department). ‘Code stroke’ is the activation of an alert system designed to provide emergency care in case of stroke in such a way as to minimise transfer time to hospital and diagnosis and treatment times in acute stroke.15
We used an electronic database (Microsoft Access® 2007) to keep daily records. Recorded data were compared to general data for patient care in the HGUGM emergency department during the same period. General data were obtained from the digital records used to manage the HGUGM emergency department. Statistical analysis was completed using SPSS® software v15.0 and Microsoft Excel® 2007 for Windows®.
ResultsBetween 1 August 2010 and 31 July 2011, a total of 236770 emergency evaluations were performed at the hospital; of these, 92762 corresponded to emergency medical care, excluding traumatology, obstetrics-gynaecology, paediatrics, and surgical emergencies. A total of 17552 hospital admissions were due to medical emergencies, which means an admission rate of 18.8% of total patients seen.
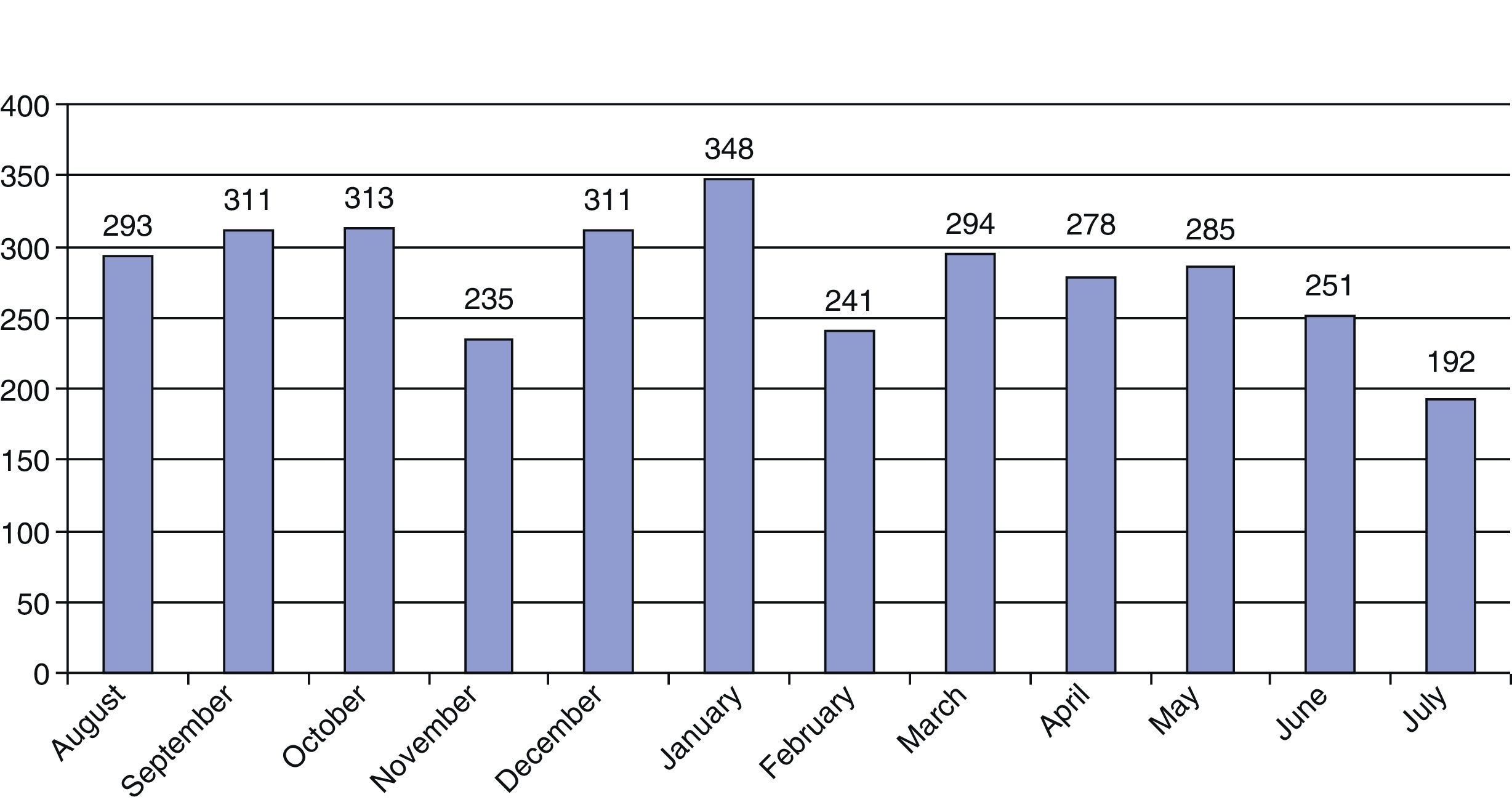
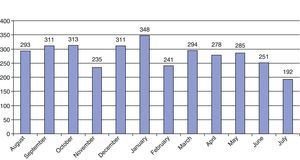
During this same period, the hospital recorded 3234 emergency patients as being treated by the neurology department, which accounts for 3.48% of the total medical emergencies. Of the 365 days analysed, we excluded 73 days (20%) because the data gathered were incomplete. An estimate for the whole year gives the percentage of emergencies seen by the neurology department as 4.35%. The demand for emergency neurological care was estimated at 11.92 patients per 1000 inhabitants per year. Doctors saw a mean of 269 patients/month and 11.15 patients/day (range: 2–23 patients). The median number, as well as mode, was 10 patients/day. January 2011 was the month with the highest demand for care (348 patients), while July 2011 was the month remained the lowest demand (192 patients). Demand for care was constant throughout all four seasons, with a slight decrease during the summer (Fig. 1).
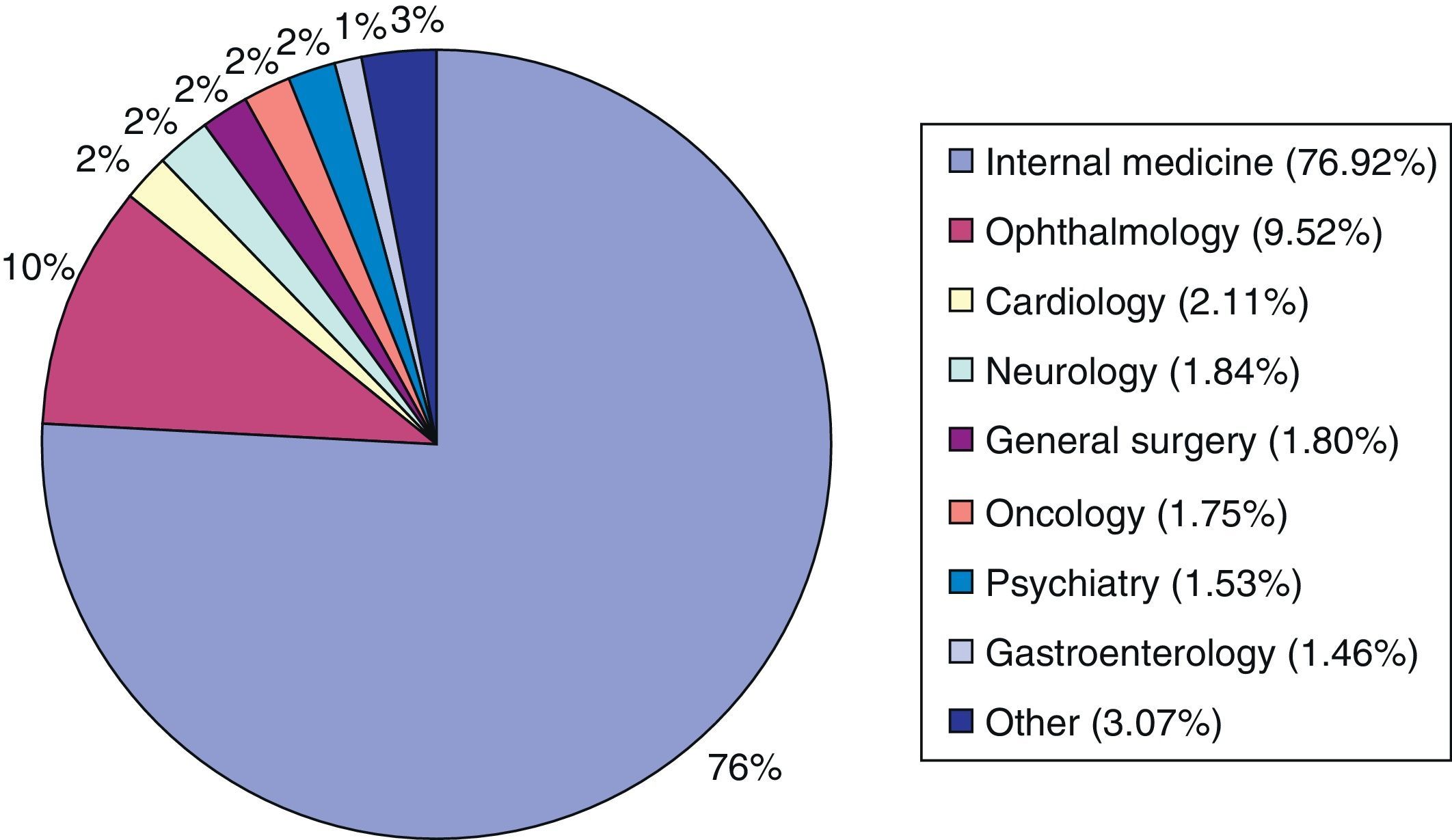
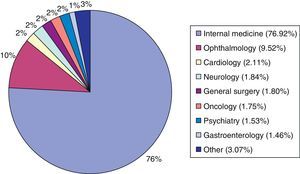
Distribution of patients by sex was homogeneous (48% men, 52% women). Mean age and standard deviation was 59.34±21.16 years. Of the patient total, 93% were Spanish. The remainder came from Latin America (4%), Eastern Europe (1%), and other locations such as sub-Saharan Africa, the Maghreb, China, Western Europe, India, and the USA (2%). Regarding time of the patient's initial evaluation, 30% were assessed in the morning (8.00–15.00), 46% in the afternoon (15.00–22.00), and 24% during the night (22.00–8.00). The neurology department initially assessed 35% of the patients, while the remaining 6% were assessed at the request of other specialists (Fig. 2). In 5% of the cases, the neurology department requested consults with other specialists: 2% with internal medicine, 1% with neurosurgery, 1% with intensive care, and 1% with others).
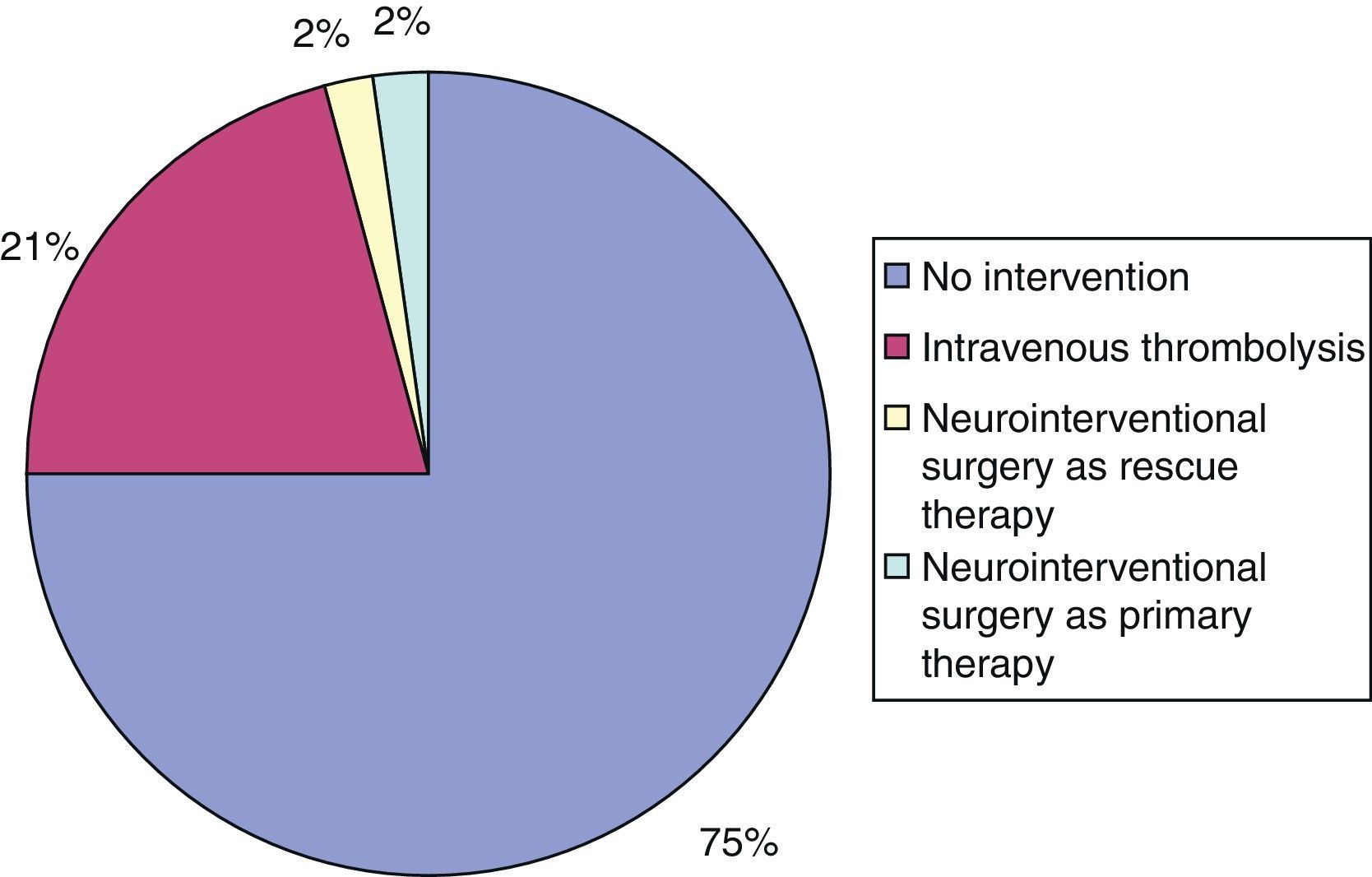
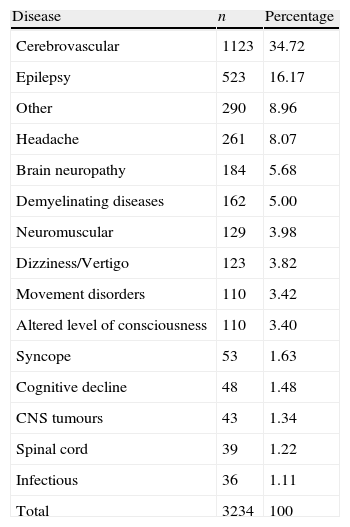
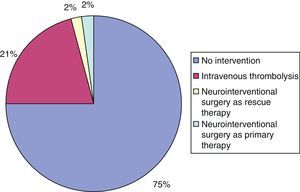
Patient assessments were completed in the emergency department in 91.83% of the cases (47.50% in the observation area, 31.56% in the outpatient area, 10.28% in the accident and emergency cubicles, and 2.49% in the HDU), while 8.17% were assessed in wards other than the neurology ward. Records show that 67 patients (2.06%) were transferred from hospitals with no on-call neurologist available for emergency neurological assessments. The most frequent diseases were cerebrovascular disease (34%), epileptic seizure (16%), and headache (8%) (Table 1). ‘Code stroke’ was activated on 306 occasions and thrombolytic or intravascular interventions were performed in 76 of these cases (25%) (Fig. 3). Mean door-to-needle time was 54.3minutes. We found no significant differences between working days (53.8minutes) and weekend days (56.4minutes).
Diseases treated by the on-call neurology team.
| Disease | n | Percentage |
| Cerebrovascular | 1123 | 34.72 |
| Epilepsy | 523 | 16.17 |
| Other | 290 | 8.96 |
| Headache | 261 | 8.07 |
| Brain neuropathy | 184 | 5.68 |
| Demyelinating diseases | 162 | 5.00 |
| Neuromuscular | 129 | 3.98 |
| Dizziness/Vertigo | 123 | 3.82 |
| Movement disorders | 110 | 3.42 |
| Altered level of consciousness | 110 | 3.40 |
| Syncope | 53 | 1.63 |
| Cognitive decline | 48 | 1.48 |
| CNS tumours | 43 | 1.34 |
| Spinal cord | 39 | 1.22 |
| Infectious | 36 | 1.11 |
| Total | 3234 | 100 |
Seventy-nine patients (2.44% of the total) required intermediate care in the HDU; stroke patients were not included in this group. The most frequent reasons for admission in the HDU were poorly controlled epileptic seizures or seizures with prolonged post-ictal periods (33.3%), haemodynamic instability (16.4%), non-invasive mechanical ventilation for respiratory failure of neuromuscular origin (13.4%), Guillain-Barré syndrome (monitoring during the first 48hours after symptom onset) (4.4%), acute spinal shock (4.5%), severe coagulation disorders (4.5%), and other (11.9%). The most common motives for emergency evaluations of pregnant women (32 total cases) were epileptic seizures (31%) and headache (25%). Six pregnant women required emergency admission; 2 women had already been admitted for different reasons.
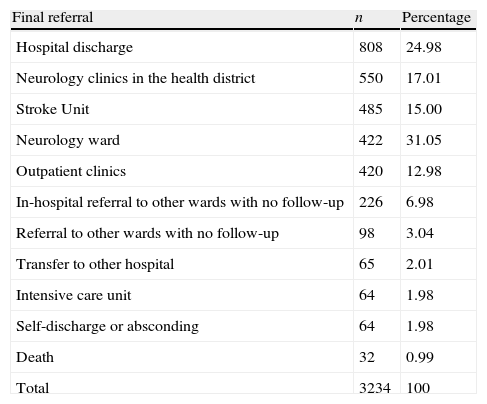
Mean hospitalisation time in the emergency department under the care of the on-call neurologist was 7.17±10.56hours per patient and the median time was 3hours per patient. The hospital admission rate of patients assessed by the neurology department was 40%, representing 7.38% of the total admissions to HGUGM due to medical emergencies. Admitted patients were transferred to the stroke unit (39.5%), neurology ward (33%), intensive care unit (3%), and other units (24.5%). Emergency readmission rate was 4.59% (we included prior evaluations by the neurology department, internal medicine department, and other specialties). Referrals of patients seen by the neurology unit are listed below (Table 2). Our hospital performed 2237 head CT scans (in 68% of the total), ordered by neurologists or other specialists. A total of 136 CT angiograms, 29 magnetic resonance imaging scans, 88 lumbar punctures, 119 electroencephalograms, and 63 emergency neurosonology studies were also performed.
Referral of patients seen by the on-call neurology team.
| Final referral | n | Percentage |
| Hospital discharge | 808 | 24.98 |
| Neurology clinics in the health district | 550 | 17.01 |
| Stroke Unit | 485 | 15.00 |
| Neurology ward | 422 | 31.05 |
| Outpatient clinics | 420 | 12.98 |
| In-hospital referral to other wards with no follow-up | 226 | 6.98 |
| Referral to other wards with no follow-up | 98 | 3.04 |
| Transfer to other hospital | 65 | 2.01 |
| Intensive care unit | 64 | 1.98 |
| Self-discharge or absconding | 64 | 1.98 |
| Death | 32 | 0.99 |
| Total | 3234 | 100 |
The workload of the on-call neurology team at HGUGM represents, in quantitative terms, 3.48% of the total share of medical emergencies. This percentage falls within the range of values published to date, from 2.6% to 14%.10,18 These data do not represent all patients with neurological symptoms in the emergency department; a previous study performed in our hospital showed that our neurology team only participated in caring for 41% of the patients referred by the emergency department to other neurology departments in our health district.12 The workload produced by emergency care to patients admitted to the neurology department was not measured. In another study, these cases accounted for 17.6% of the total, a scenario which reveals one of the main limitations of our study.10 The admission rate for patients assessed by the neurology department was higher than that in the medical emergency group (40% vs 18%). This information points to high severity, morbidity, and disability of patients assessed by the neurology team compared to those seen by other specialties, as shown by previous studies.10,18 Despite this fact, only 47% of the 69 neurology training centres in Spain have institutional on-call neurologists available 24hours a day.13
Providing specialised neurological care to stroke patients has been demonstrated to decrease mortality and in-hospital complications and increase the percentage of disability-free patients.19 This is the reason why emergency stroke care strategies, teams, and units have been created in recent years: stroke is the second-leading cause of mortality and the main cause of morbidity in Spain.20 Despite these efforts, currently available resources for treating stroke still trail far behind those considered necessary by the Spanish Society of Neurology's Study Group for Cerebrovascular Diseases (GEECV). According to their recent report, only 48% of provinces had a stroke unit in 2011, and only Asturias, Cantabria and the Basque Country met the goal of having a stroke unit bed per 100000 inhabitants.21
The demographic profile of the patients assessed by the neurology department in our study resembled that in other studies conducted in Spain.1 Patient care outside normal working hours (15.00–8.00) represented 69% of the total; this figure justifies the need for a 24-hour on-call neurology team, as has also been shown by other studies.10 Requests from other specialists motivated 65% of the evaluations, which could indicate a certain degree of dependency on the neurologist, or an increasing case complexity exceeding the scope of other specialists. Other studies showed that the internal medicine department requested the most evaluations; the department with the second-highest number of requests varied from study to study.22 The neurology team requested evaluations by other specialists in only 5% of their patients. These data could be interpreted as an indication of self-sufficient and comprehensive management of neurological patients, but it could also be explained by the high specificity of neurological diseases.
As seen in many previous studies, cerebrovascular disease, epilepsy and headache predominate in our setting, representing 58% of the total.10,18,23–25 As in other studies, neurologists treated a surprisingly low percentage of cases of neurological infectious disease (1.05%). These cases are predominantly handled by the internal medicine department.23,24,26 Use of the ‘code stroke’ system has been shown to improve functional outcomes of acute stroke patients.20,27 The fact that thrombolytic or intravascular interventions were only carried out in 25% of ‘code stroke’ cases shows the relevance of having an on-site neurology team able to appropriately select candidates for these treatments. As other studies have shown, the benefits of these treatments depend on the doctor administering them.28,29 Studies have also shown that presence of an on-call neurologist has a positive impact on the management of headache patients, resulting in a reduction in admissions for this condition of more than 50%.30
Over the last few years, the implementation of stroke units has permitted many stroke patients to benefit from higher quality care during the acute phase of stroke. However, some patients with non-vascular neurological disease and an intermediate level of severity are not candidates for intensive care. Such patients are not sufficiently monitored, usually due to lack of appropriate structural support in hospitals. This group of 74 patients represented 2.29% of the total and received adequate care through the intermediate care unit (HDU) in our hospital's emergency department. Although interest in intensive neurological care is certainly growing, neuro-ICUs in Spain are still far from materialising, especially in the context of the current economic situation.31–33
What is surprising here is the high percentage of patients who underwent emergency brain CT scans (68%). We cannot identify the departments that requested these tests, as this information was not systematically recorded. In other studies, this percentage was lower (18%); however, they only mention tests ordered by the neurology department.10 Fewer emergency neurosonology studies were performed in our hospital than in other centres.10 This was probably due to CT-angiography being available around the clock and to systematic admission to the stroke unit of every patient with transient ischaemic attack, which ensures performance of CT-angiography in less than 24hours in line with the latest recommendations.
Our study's main limitations were incomplete data collection on 20% of the days and not measuring the workload generated by emergency care for patients previously admitted to the neurology department, neurology ward, or the stroke unit. Incomplete data gathering was mainly due to failure on the part of the data gathering team, probably due to excessive workload or fatigue during on-call hours. These days were homogeneously distributed throughout the year with no concentrated periods. It is therefore possible that our results underestimate the workload of the on-call neurology team.
This study shows that neurological diseases seen in the emergency room are frequent, complex and diverse, and that they account for a high percentage of the total patients seen or admitted on an emergency basis. We should highlight the admission rate among patients treated by the neurology team (2 times the general rate), and the high volume of neurological assessments requested by other specialists. Cerebrovascular disease, epilepsy, and headaches are predominant in our setting. The above data justify the presence of a 24-hour on-call neurology team in the emergency department, as well as the need to provide hospitals with the technical and human resources necessary to deliver equitable emergency neurological care in Spain.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Rodríguez Cruz PM, Pérez Sánchez JR, Cuello JP, Sobrino García P, Vicente Peracho G, García Arratibel A, et al. Labor asistencial del equipo de guardia de neurología en un hospital terciario de Madrid: análisis prospectivo durante un año. Neurología. 2014;29:193–199.
These results have been partially presented at the 15th Congress of the European Federation of Neurological Societies (EFNS), under the title “Neurology on-call coverage in a Spanish tertiary academic hospital: a prospective one-year study”. P1815. Eur J Neurol. 19 Suppl. 1; 90–457.