Telemedicine (TM) can help in the management of chronic obstructive pulmonary disease (COPD). This study examines knowledge, current use and potential limitations for practical implementation of TM for the remoted management of COPD patients among members of the COPD area of SEPAR (n=3118).
Material and methodsAn electronic survey was circulated three times to these 3118 health-care professionals. Their knowledge, current use and potential limitations for implementation of different forms of TM, including tele-monitoring, tele-education and self-care, tele-rehabilitation and mobile health, for the remote management of COPD patients were tabulated and described.
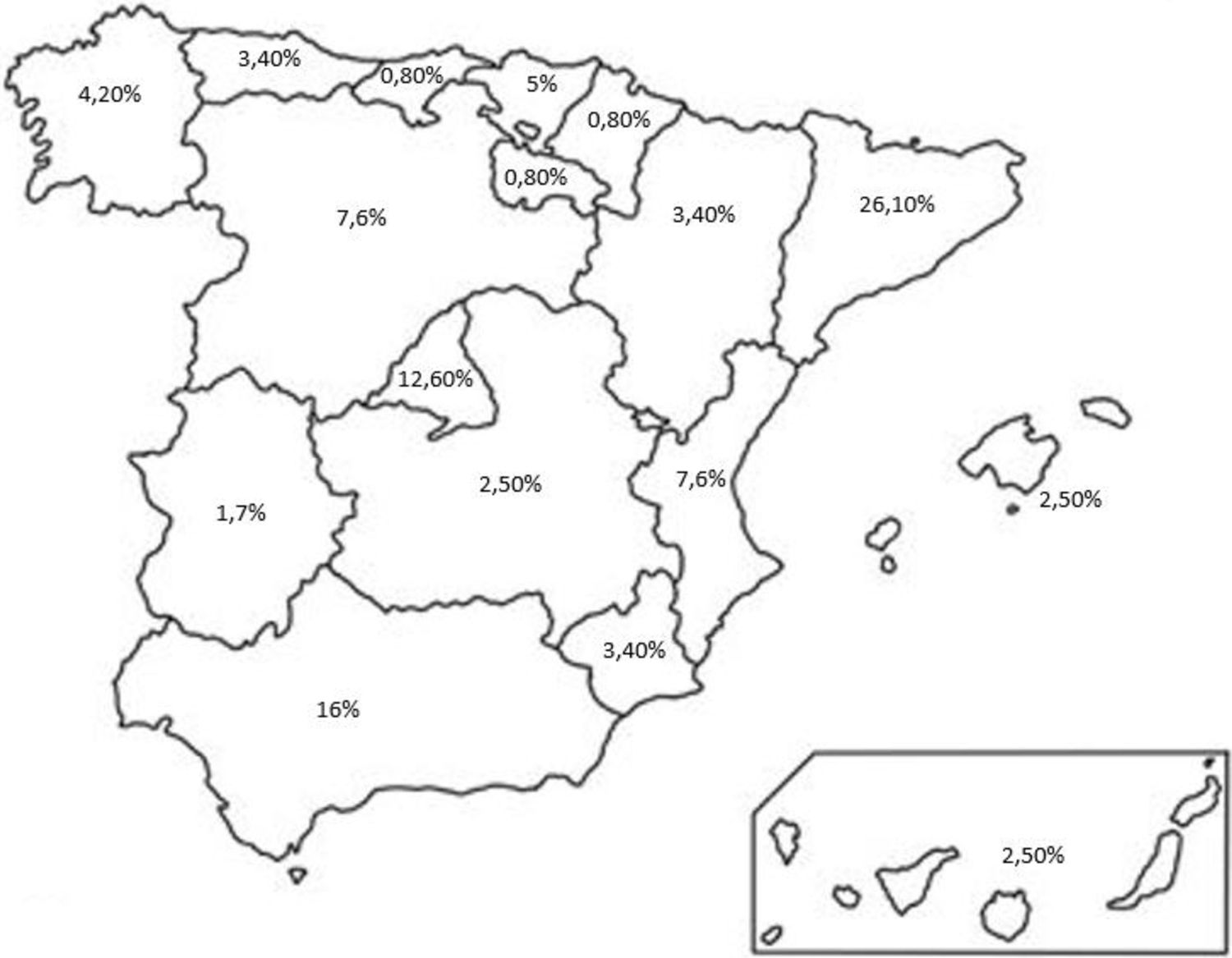
ResultsOnly 120 health-care professionals responded to the survey (3.9%). The rate of response varied greatly across different Autonomous Communities (AACC); 99.2% of responders declared being aware of TM, but only 60.5% knew about the different TM alternatives investigated here, and only 40.3% actually used some form of TM for their current management of patients with COPD. Of those using TM, 47.1% referred being satisfied with its use. Main identified barriers for implementation of TM in their institutions were technological limitations and data security.
ConclusionsThe potential of TM for the clinical management of COPD is well known among interviewed health-care professionals, but only less than half used it currently. The potential for growth is therefore clear. We propose that SEPAR analyze critically this potential and promotes measures to achieve it for the benefit of COPD patients.
La telemedicina (TM) puede ayudar en el tratamiento de la enfermedad pulmonar obstructiva crónica (EPOC). Este estudio examina el conocimiento, el uso actual y las posibles limitaciones para la implementación práctica de la TM para el tratamiento remoto de pacientes con EPOC entre los miembros del área de EPOC de la SEPAR (n=3.118).
Material y métodosSe distribuyó 3 veces una encuesta electrónica entre estos 3.118 profesionales de la salud. Se tabularon y describieron sus conocimientos, el uso actual y las limitaciones potenciales para la implementación de diferentes formas de la TM, incluida la telemonitorización, la teleeducación y el autocuidado, la telerrehabilitación y la salud móvil, para el tratamiento remoto de los pacientes con EPOC.
ResultadosSolo 120 profesionales sanitarios respondieron a la encuesta (3,9%). La tasa de respuesta varió mucho entre las distintas comunidades autónomas (CC. AA.); el 99,2% de los encuestados declaró conocer la TM, pero solo el 60,5% conocía las diferentes alternativas de la TM investigadas aquí, y solo el 40,3% realmente utilizó alguna forma de TM para el manejo actual de los pacientes con EPOC. De quienes utilizan la TM, el 47,1% refirió estar satisfecho con su uso. Las principales barreras identificadas para la implementación de la TM en sus instituciones fueron las limitaciones tecnológicas y la seguridad de los datos.
ConclusionesEl potencial de la TM para el tratamiento clínico de la EPOC es bien conocido entre los profesionales sanitarios entrevistados, pero solo menos de la mitad la utiliza actualmente. Por tanto, el potencial de crecimiento es claro. Proponemos que la SEPAR analice críticamente este potencial y promueva medidas para alcanzarlo en beneficio de los pacientes con EPOC.
The term “telemedicine” (TM) refers to the use of electronic technology to enable communication between health professionals and patients (or caregivers) in order to provide health care to those who are far from health institutions.1,2 TM so defined is a general term that encompasses several different concepts, since it can be used for remote monitoring of patients, promotion of health education and self-management of the disease, early recognition and management of episodes of exacerbation episodes, and/or the promotion of physical activity and rehabilitation, among others.1,2
Chronic obstructive pulmonary disease (COPD) is a major public health problem due to its high prevalence (11.8% [95% C.I. 11.2–12.5] in the adult population of our country3), health impact and associated socioeconomic cost.4 TM can be useful in patients with COPD because: (1) the ageing of the population creates mobility difficulties which in turn generates a greater demand for remote monitoring and care; (2) technological advances offer opportunities to improve personalized health care and reduce economic costs, as well as the environmental impact derived from the need to transport patients to the health centre; (3) the possibility of early detection and initial treatment of COPD exacerbations remotely; (4) TM provides the opportunity for continuous remote education of both the patient and the caregiver; and finally (5) it reduces barriers and facilitates access to health care for these patients.5
Recently, we published a systematic review on the safety and effectiveness of TM in patients with COPD, structured in four different domains: tele-monitoring, tele-education and self-care, tele-rehabilitation and mobile health (mHealth).6 Results showed that, although the available evidence is still weak in many of these domains, TM is a viable and safe option for COPD patients, it improves their health status, it reduces the use of health care resources and is well appreciated by the patients.6 However, it also showed that the use of TM is not yet widespread in routine clinical practice7 due largely to the necessary organizational changes and the education and awareness of health-care professionals.8 Therefore, here we sought to understand the use of TM and its modalities in the remote clinical management of patients with COPD in our country, as well as to explore potential organizational and/or logistical barriers that facilitate or limit the implementation of TM tools in routine clinical practice. To do this, we circulated an electronic survey to all members of the COPD area of the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) requesting their voluntary participation.
MethodsStudy design and ethicsThis qualitative, cross-sectional study was designed to collect quantifiable data on the use of TM and their modalities, as well as to evaluate potential limitations to its practical implementation, using an electronic survey that was circulated to all members of the SEPAR COPD area (n=3118) with the consent of SEPAR. Information about the purpose of the study was provided and anonymization of their responses was ensured. The data collection period ranged from July 2023 to February 2024. During this period, three friendly reminders were sent. Responses were structured using Likert scales, dichotomous and multiple options questions to facilitate their quantitative analysis. The study was approved by the CEIM of the Catalan Union of Hospitals (code number 23/71). All responders accepted their participation in the study voluntarily and signed their informed consent digitally.
Data analysisResults are shown as n, range, percentage and/or mean±standard deviation. The R-Rstudio v4.2.3 software was used for data analysis.
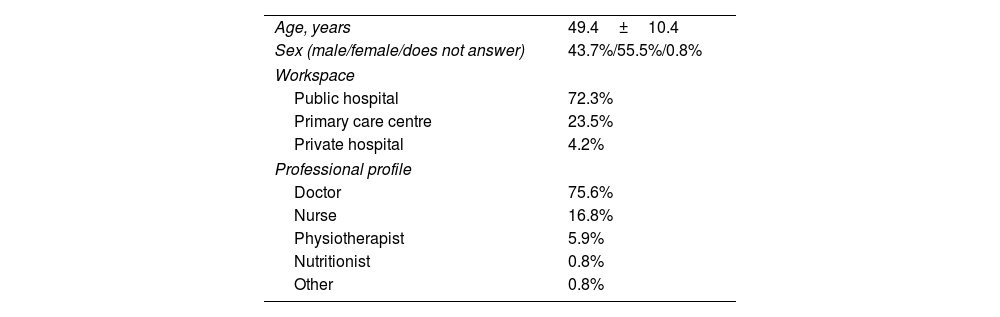
ResultsSurveyed populationOnly 120 members of the COPD area of SEPAR responded to the survey (3.9% of all). Participation was however very different in different regions of the country (Fig. 1). Table 1 shows the main characteristics of responders. Their mean age was 49.4±10.4 years, gender distribution was similar, the majority of them worked in a public hospital setting and were mostly physicians.
Characteristics of the surveyed population (n=120). Data is presented as mean±SD or proportions.
| Age, years | 49.4±10.4 |
| Sex (male/female/does not answer) | 43.7%/55.5%/0.8% |
| Workspace | |
| Public hospital | 72.3% |
| Primary care centre | 23.5% |
| Private hospital | 4.2% |
| Professional profile | |
| Doctor | 75.6% |
| Nurse | 16.8% |
| Physiotherapist | 5.9% |
| Nutritionist | 0.8% |
| Other | 0.8% |
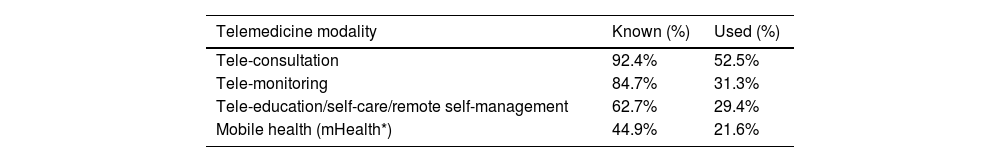
Although 99.2% of respondents stated that they were familiar with TM in general, only 60.5% of them knew an institution that uses TM for the management of COPD, and only 40.3% uses it in their own centre. Tele-consultation and tele-monitoring were the best-known uses of TM while mobile health devices were the least ones, with the proportion of actual users being less than half (Table 2). Among the latter, 47.1% indicated that they were satisfied as health-care professionals with the use of TM for the remote management of patients with COPD. Finally, architectural and logistical barriers, including limitations of technological infrastructure, concerns about data security, and difficulty of integration of TM in existing healthcare systems, were identified by 56.3% of responders as the main hurdles for the adoption of TM in their respective institutions.
Degree of knowledge and use of various TM modalities for the remote clinical management of patients with COPD.
| Telemedicine modality | Known (%) | Used (%) |
|---|---|---|
| Tele-consultation | 92.4% | 52.5% |
| Tele-monitoring | 84.7% | 31.3% |
| Tele-education/self-care/remote self-management | 62.7% | 29.4% |
| Mobile health (mHealth*) | 44.9% | 21.6% |
The results of this study are limited by the low response rate to the survey (despite repeated invitations) but, with this caveat in mind, they show that: (1) the vast majority of responders was aware of the possibility of using TM tools in the clinical management of patients with COPD, although less than half of them used them in their own institution due to various architectural and/or logistical limitations; and (2) 47.1% of those who use TM to care for COPD patients were satisfied with its use.
Previous studiesDuring the COVID-19 pandemic, TM tools experienced a significant boost due to the need of social distancing,9–12 with good acceptance by patients and professionals.13 This level of acceptance may vary in a post-pandemic context for the clinical management of chronic diseases.13,14 In the field of COPD, there are few studies on the use of TM in these patients.15–17 Our recently published systematic review on this topic showed that, although the available evidence is still weak, TM is a viable and safe option for COPD patients, improves their health status, reduces the use of health-care resources and is positively valued by patients and professionals.6
Interpretation of survey resultsThe response rate to the survey was low and heterogeneous (Fig. 1). The CCAA of Catalonia, Andalusia and Madrid clearly led it. We do not know if this observation responds to a different interest in the use of TM in COPD in different CCAA (higher in larger ones, perhaps with greater access to telematic tools) or, simply, to a lack of interest/time in answering this survey. This last possibility represents a missed opportunity to generate potentially useful information for SEPAR in its strategic plan and dialogue with the administration.
Participation in the survey was similar in men and women, indicating that interest in the use of telemedicine in the management of COPD is independent of gender. Most responders worked in a hospital setting (Table 2) where, possibly, there are more facilities for technological implementation of TM. However, the significant participation of primary care professionals is encouraging, as they play a key role in the chronic care of patients with COPD.
Finally, although the vast majority of respondents claimed to be familiar with TM, less than half of them (Table 2) uses it in their own centre, indicating that there is ample room for improvement. A more detailed analysis of the potential reasons limiting the use of TM in clinical practice may help its implementation for the benefit of patients with COPD.
Strengths and limitationsThe main strength of this study is that it is the first carried out among members of the COPD area of SEPAR (a national professional society that incorporates a variety of health professions) on the role of TM in the clinical management of these patients. Among its limitations, the low response rate is of note. Besides, it is possible that the real rate of TM use may be lower if we consider that the mean age of responders was 43 years whereas the COPD area of SEPAR includes also older pulmonologists, likely less prone to use TM in their practice.
ConclusionsMost responders were aware of the potential of TM tools for the clinical management of COPD patients, but less than half of them used them. There is, therefore, ample room for improvement in the use of TM in these patients. We propose that SEPAR analyzes critically this potential and promotes measures to achieve it for the benefit of COPD patients.
FundingNone declared.
Authors’ contributionsAll authors contributed to the design of the study, interpretation of results and approved the final manuscript.
Conflicts of interestNone declared.
The authors thank all the responders for their time and the information provided.