The first-line treatment for obstructive sleep apnoea is (OSA) continuous positive airway pressure (CPAP) therapy, which achieves a high level of efficacy with continuous use. However, daily application of this therapy requires a motivated patient profile, as lack of adherence is the main problem with this therapy. The aim of this study was to determine whether an educational and training program based on motivational interviewing and proper feedback, improved adherence.
MethodsA randomized, controlled, single-center trial design was performed. The interventions were standard of care vs MEntA Program based on motivational interview for adherence. The main outcome was the adherence with the CPAP therapy after 90 days of treatment. Secondary outcomes were the motivation, perceived competence, quality of life, sleepiness, emotional state, activities and social relations.
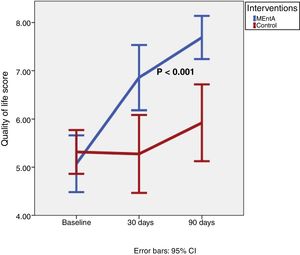
ResultsFor adherence, statistically significant results were obtained in favor of the interventional arm with the MEntA (p<0.01), with a mean difference of 1.60h (95% CI, 0.60 to 2.61). The Questionnaire of Evaluation of Perceived Competence in Adherence to CPAP in OSA show also a statistically significant change in favor of the MEntA intervention with a mean difference of 4.61 (95% CI, 3.49 to 5.72) (p<0.001), as well as quality of life p<0.001.
ConclusionsThe MEntA intervention included as part of an educational and training program for patients with OSA with CPAP therapy shows solid results in terms of its efficacy.
El tratamiento de primera línea para la apnea obstructiva del sueño (AOS) es la terapia de presión positiva continua en las vías respiratorias (CPAP), que alcanza un alto nivel de eficacia con el uso continuo. Sin embargo, la aplicación diaria de esta terapia requiere un perfil de paciente motivado, ya que la falta de adherencia es el principal problema de esta terapia. El objetivo de este estudio fue determinar si un programa educativo y de capacitación basado en entrevistas motivacionales y una adecuada retroalimentación, mejoró la adherencia.
MétodosSe realizó un diseño de ensayo aleatorizado, controlado y de un solo centro. Las intervenciones fueron el estándar de atención frente al programa MEntA basado en la entrevista motivacional para la adherencia. El outcome principal fue la adherencia a la terapia CPAP después de 90 días de tratamiento. Los outcomes secundarios fueron la motivación, la competencia percibida, la calidad de vida, la somnolencia, el estado emocional, las actividades y las relaciones sociales.
ResultadosPara la adherencia se obtuvieron resultados estadísticamente significativos a favor de la intervención con MEntA (p<0.01), con una diferencia media de 1.60 horas (IC95%, 0.60 a 2.61). El Cuestionario de Evaluación de la Competencia Percibida en Adherencia a CPAP en SAHOS muestra también un cambio estadísticamente significativo a favor de la intervención MEntA con una diferencia media de 4,61 (IC95%, 3,49 a 5,72) (p<0,001), así como calidad de vida p<0,001.
ConclusionesLa intervención MEntA incluida como parte de un programa educativo y formativo para pacientes con AOS con terapia CPAP muestra sólidos resultados en cuanto a su eficacia.
Obstructive sleep apnea is a chronic illness with increasing prevalence. In addition to associated cardiovascular comorbidities, obstructive sleep apnea syndrome has been linked to poor quality of life, occupational accidents, and motor vehicle crashes secondary to excessive daytime sleepiness.1 The first-line treatment is continuous positive airway pressure (CPAP) therapy, which achieves a high level of efficacy with continuous use. Standard treatment consists of starting therapy where practical training in the use of CPAP is carried out, with a series of scheduled visits to monitor adherence. In Spain, for the beginning of therapy, the performance of “CPAP Schools” has been standardized. It consists of summoning the patient and her partner in groups of no more than 8–10 people. A trained nurse explains what CPAP is and how it works. In this way, the CPAP installation is carried out in the sleep unit or specialized consultation. In addition to being well accepted by patients, they are cost-effective.2
Multidisciplinary approaches have been proposed, from the perspective of behavioral changes or constant monitoring.3
Behavioral therapy such as motivational interview (MI) shows promise as a means of maximizing CPAP adherence.4–7 With MI, the key goal is to empower the patient to commit to follow CPAP therapy, while providing empathic support, in a positive atmosphere, and without prejudice. The nurse does not directly advocate for behavior change (i.e. use CPAP as prescribed), but asks key questions to help the patient explore their feelings about the change, weighs the pros and cons of such change, and allows the patient to realize the discrepancy between the current risk (that is, not using CPAP as directed) and the benefits with good adherence.
The objective of this study was to determine whether the educational and training program ‘MEntA’ based on the use of the motivational interview technique in patients diagnosed with OSA with CPAP treatment improves of adherence, variables related to the efficacy of therapy and quality of life. MEntA (‘Motivation Interview Adherence’ in Spanish; Motivational & Interview for Adherence) is presented as a structured program (content, materials, and sessions) with the use of the specifically directed motivational interview in the continuous treatment (not only in a specific way) of CPAP.
Materials and methodsDesignA randomized, controlled, single-center trial design was performed. Adult patients with OSA who attended the Respiratory Medicine Department at La Princesa University Hospital (Madrid) were enrolled between March and April 2018. The study protocol was approved by the Clinical Research Ethics Committee at the participating hospital (Registration number: 3687). This Committee reports to the Spanish Drug Agency, where all clinical studies are registered at the national level.
PatientsThe subjects enrolled in the study were required to have a diagnosis of OSA confirmed by polysomnography (PSG), be recommended for treatment with CPAP and be naïve to this type of intervention. The study excluded subjects requiring bi-level ventilation, such as those with central sleep apnoea syndrome, a CPAP assessment study, those with severe chronic obstructive pulmonary disease (COPD), cognitive disorders and those unable to understand the consent form to participate. Prior to enrolment in the study, all patients were informed in detail about the study and signed the consent form to participate.
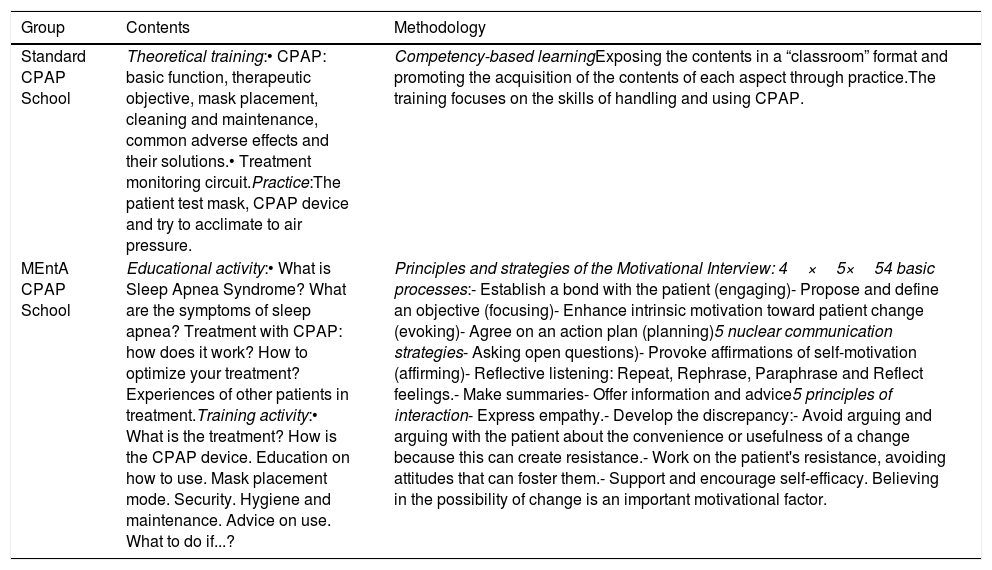
InterventionsStandard of care group: subjects undergoing this training intervention follow the standard procedure. It consists of a CPAP School for the initiation of therapy, and follow-up visits (in person and/or by telephone) that follow the frequencies indicated by the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR).2 The CPAP School consists of a single session lasting around 80min. The theoretical training includes the importance of adherence, as well as handling the equipment and accessories, cleaning and maintenance of the equipment, and prevention of complications and possible side effects. The practical training consists of showing patients how to carry out the technique themselves. The learning methodology used is called “competency-based learning”, which consists of exposing the contents in a “classroom” format and promoting the acquisition of the contents of each aspect through practice. The training focuses on the skills of handling and use of CPAP (Table 1). The follow-up is carried out one month and 90 days after the start of therapy, supervised by the nurse who checks compliance and resolves any difficulties that may have arisen.
Contents and methodology used in each of the groups.
| Group | Contents | Methodology |
|---|---|---|
| Standard CPAP School | Theoretical training:• CPAP: basic function, therapeutic objective, mask placement, cleaning and maintenance, common adverse effects and their solutions.• Treatment monitoring circuit.Practice:The patient test mask, CPAP device and try to acclimate to air pressure. | Competency-based learningExposing the contents in a “classroom” format and promoting the acquisition of the contents of each aspect through practice.The training focuses on the skills of handling and using CPAP. |
| MEntA CPAP School | Educational activity:• What is Sleep Apnea Syndrome? What are the symptoms of sleep apnea? Treatment with CPAP: how does it work? How to optimize your treatment? Experiences of other patients in treatment.Training activity:• What is the treatment? How is the CPAP device. Education on how to use. Mask placement mode. Security. Hygiene and maintenance. Advice on use. What to do if...? | Principles and strategies of the Motivational Interview: 4×5×54 basic processes:- Establish a bond with the patient (engaging)- Propose and define an objective (focusing)- Enhance intrinsic motivation toward patient change (evoking)- Agree on an action plan (planning)5 nuclear communication strategies- Asking open questions)- Provoke affirmations of self-motivation (affirming)- Reflective listening: Repeat, Rephrase, Paraphrase and Reflect feelings.- Make summaries- Offer information and advice5 principles of interaction- Express empathy.- Develop the discrepancy:- Avoid arguing and arguing with the patient about the convenience or usefulness of a change because this can create resistance.- Work on the patient's resistance, avoiding attitudes that can foster them.- Support and encourage self-efficacy. Believing in the possibility of change is an important motivational factor. |
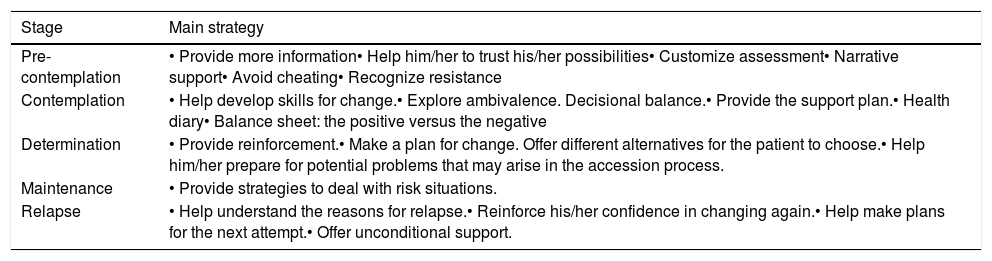
MEntA group: subjects in this group underwent an intervention based on the motivational interviewing (MI) technique in CPAP School format for the initiation of therapy, and follow-up as indicated by SEPAR. MEntA CPAP School intervention consists of one session lasting approximately 90min, which is divided into two blocks: educational activity and training activity. In the first block, an expert explains the concepts of sleep apnoea and the symptoms, while a patient shows the CPAP treatment and how to optimize this to the fullest. This block was reinforced with documentation in hard copy and digital format. The second block on training activity was based on working with the treatment, equipment, safety, hygiene and advice. MEntA has the specific contents but the key is in how these contents are treated with the patients, using the MI to the treatment of OSA with CPAP. Using MI, the nurse does not directly advocate for behavior change (i.e. use CPAP as prescribed), but asks key questions to help the patient explore conflicting feelings about the change, weighs the positive consequences and negatives of this change, and allows the patient to realize the discrepancy between current risk behavior (i.e. not using CPAP as directed) and the patient's self-identified goals. The nurse uses MI rules (Table 1) not only at the beginning of therapy, but also in every contact that the patient has with the patient throughout the treatment (subsequent follow-up visits, phone calls, etc.). Table 2 shows the main MI strategies to be used during CPAP School and follow-up, depending on the stage of the patient.
Description of the Motivational Interview Interventions in each of the stages.
| Stage | Main strategy |
|---|---|
| Pre-contemplation | • Provide more information• Help him/her to trust his/her possibilities• Customize assessment• Narrative support• Avoid cheating• Recognize resistance |
| Contemplation | • Help develop skills for change.• Explore ambivalence. Decisional balance.• Provide the support plan.• Health diary• Balance sheet: the positive versus the negative |
| Determination | • Provide reinforcement.• Make a plan for change. Offer different alternatives for the patient to choose.• Help him/her prepare for potential problems that may arise in the accession process. |
| Maintenance | • Provide strategies to deal with risk situations. |
| Relapse | • Help understand the reasons for relapse.• Reinforce his/her confidence in changing again.• Help make plans for the next attempt.• Offer unconditional support. |
For the MEntA group, a nurse was specifically trained to give this intervention to patients. This aspect is fundamental, since the key to the success of MI is not due to the assimilation of knowledge about OSA and its treatment, but to the acquisition of certain communication skills (see Tables 1 and 2). The training process done by a specialist psychologist consisted of an introduction to MI, training in evaluating the motivation of the patient, stage-specific interventions and how to use the materials using this communication strategy. Meanwhile, in the standard training group, the nurse carried out the intervention in the usual way (competency-based learning), giving information about how the device function and about the patients’ experience during the technique evaluation study.
Unlike the standard intervention, the key component of this intervention is the personalized feedback, which is based on the MI technique. While the subjects received general feedback on OSA, they were also given feedback on their own responses to the questionnaire. The three key components of this intervention are establishing a connection with the patient, agreeing on a training plan and expressing empathy. Furthermore, it leads to statements of self-motivation and the patients’ intrinsic motivation toward change is encouraged.
Family members are invited to participate in both groups. However, on numerous occasions the patient attends alone. The average time of the training part of the CPAP School is 20min, not including the time dedicated to the adjustment of the mask, and general management of CPAP, which is an average of 50min. In total, the start of therapy in the standard treatment (control group) takes about 80min on average. The mean time for follow-up visits in standard treatment is 15min/visit. The average time of the educational and training part of the CPAP School with MEntA is 25min, and the part of the session dedicated to mask fitting, equipment management, etc. is 40min. In this case, the practical contents are carried out simultaneously with the more theoretical contents. The average time devoted to the evaluation with questionnaires is 15min. The total time to start therapy using MEntA is 80min on average. The average time on follow-up visits MEntA treatment is 20min/visit. The main difference between the two is the methodology used.
OutcomesFor the main outcome, adherence with the CPAP therapy after 90 days of treatment was assessed. The total number of night-time hours registered by the CPAP device was recorded by specific counters within the device. These data were collected by the nursing team during the study follow-up period. The data were also analyzed after 30 days as a secondary outcome.
The secondary outcomes were motivation, perceived competence, quality of life, sleepiness, emotional state, daily activities and social relationships. All were analyzed at 30 and 90 days. Motivation was also assessed, as defined in the Prochaska and DiClemente transtheoretical model,8 using an open-ended question to the patient “Your doctor has diagnosed OSA and we have explained the treatment with CPAP, as well as the need for changes in your lifestyle to make it healthier. What do you think about this?”. The nurse classified the answer in one of the five stages: precontemplation (very low motivation), contemplation (low motivation), determination (some motivation), active change (quite motivated) and maintenance (high motivation). For perceived competence was used the validated Questionnaire of Evaluation of Perceived Competence in Adherence to CPAP in OSA (CEPCA).9 This questionnaire consists of 3 categories and 13 items: knowledge of OSA and its associated risk; expectations regarding CPAP treatment; and confidence in overcoming obstacles associated with the use of this type of treatment. The scores obtained in the CEPCA imply they are positively related to quality of life and motivation and negatively related to daytime sleepiness.
The quality of life was assessed using the Visual Analogical Well-being Scale for apnoea10 and sleepiness was assessed using the Epworth Sleepiness Scale (ESS).11,12 Finally, emotional state, daily activities and social relationships were also measured using the following ad hoc question “Taking into account your sleep problems, how would say you are in terms of mood/activities/social relationships?”. The answer alternatives are: Good, Normal/no change, Bad.
Data analysisReviews of previous research on the efficacy of motivational interviewing in patients undergoing CPAP treatment on the outcome variables that are considered (somnolence, adherence, quality of life), revealed that some studies that do not accurately detail the design of the studies, and therefore do not offer data on standardized effect size that serve as a starting point in the definition of, among other aspects, the ideal sample size for our research. Considering those that do detail it, due to the characteristics of the existing studies6 we observe values of the effect size around 0.50. In addition, for a study such as the one proposed, a sufficient number of subjects is required to allow observing and assuming the normality of the scores in the variables considered, as well as the performance of multivariate analyses, with a sufficient number of observations to carry them out. For all the above considerations, we conclude that at least 33 subjects per group would be the size of the sample necessary to assess the therapeutic efficacy of the interventions developed. On the other hand, we take into account the type of patient we are treating, who tends to drop out of treatment in the initial stages, for which a minimum number of 36 subjects per group was established (anticipating a certain experimental mortality).
A descriptive analysis of the demographic and clinical characteristics of all patients enrolled in the study was performed, as well as a baseline analysis comparing both study groups after randomization. For comparison of the results with continuous outcomes, normality tests were performed in advance, which determined the use of parametric or non-parametric analysis models. For parametric data, we used Student's t-test, while the non-parametric data distributions were compared based on the Mann–Whitney U test. The chi-squared test or Fisher's exact test was used for categorical variables. Analyses were carried out to compare the final outcomes as well as an analysis to compare the changes from baseline between the study groups. To adjust baseline imbalances, generalized lineal model (GLM) with a scale response distribution was used. The scale parameter method for this model was maximum likelihood estimate using a type III analysis and a Wald IC95%. The results included the observation of Relative Risk (RR).
The alpha value used was 0.05 and the analyses were carried out in the form of two-tailed tests. All data were analyzed using SPSS software v25 (IBM Corporation, Armonk, NY).
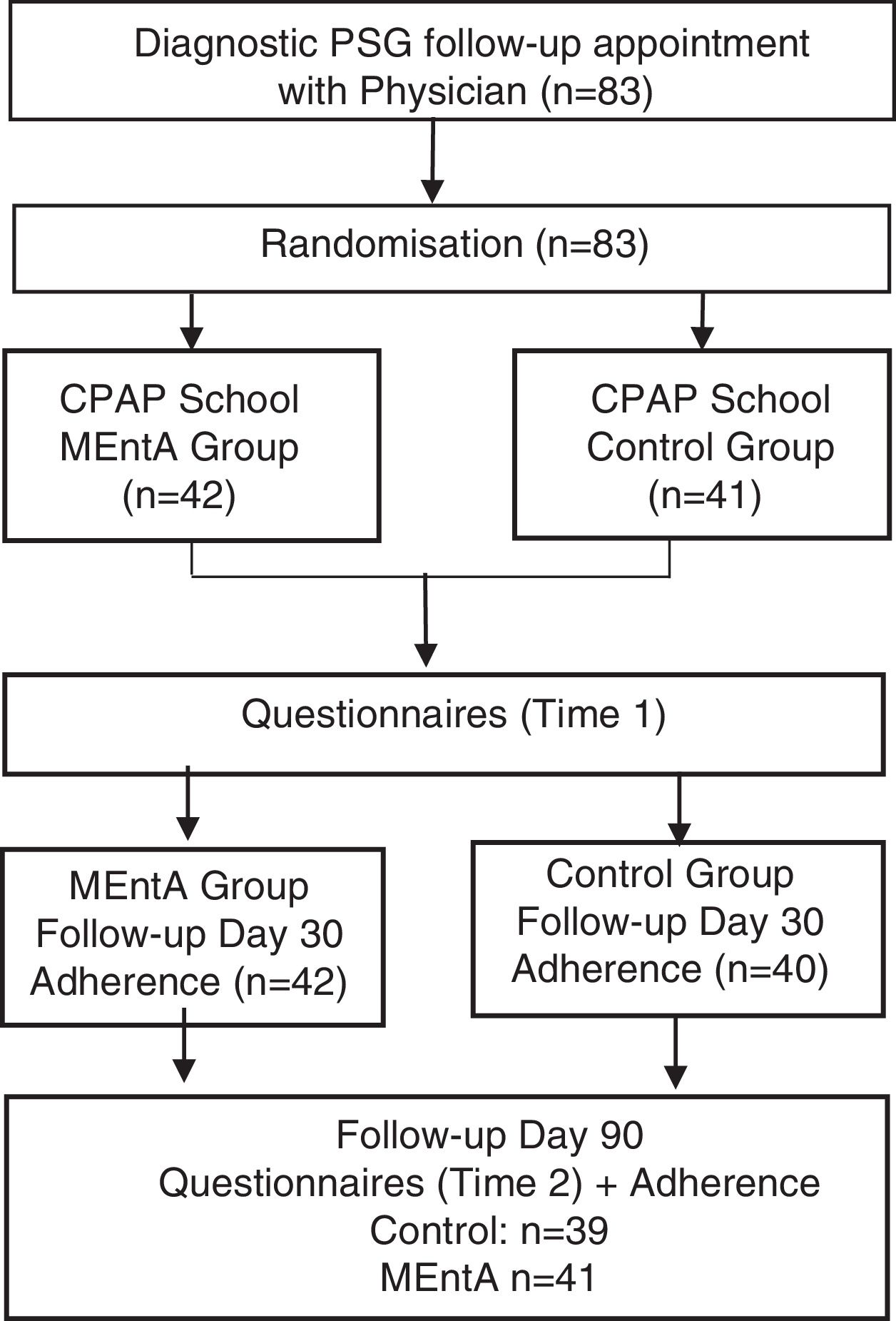
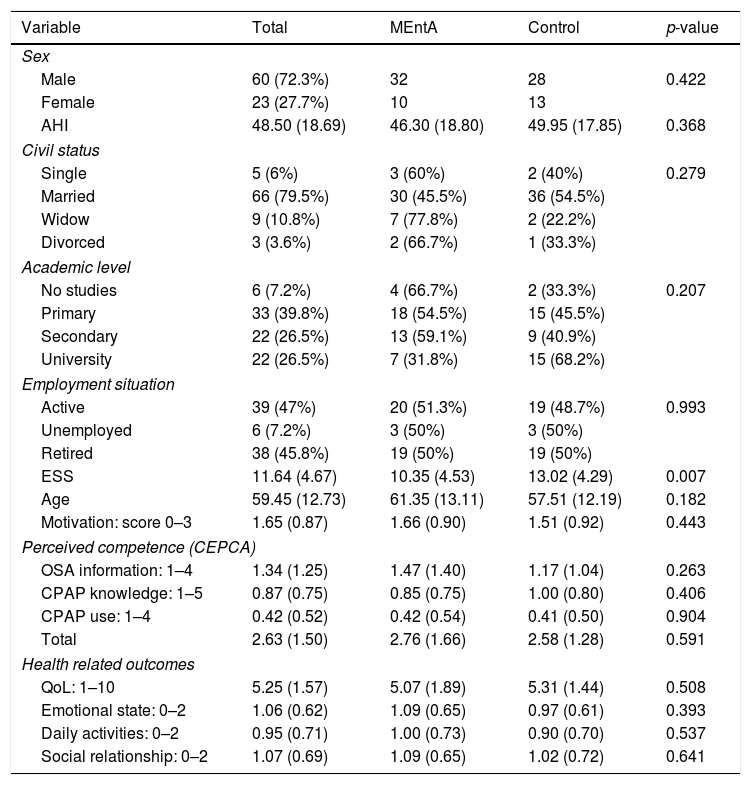
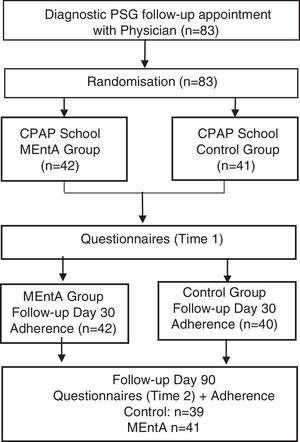
ResultsA total of 100 patients were initially screened to obtain 83 subjects who met the inclusion criteria and could be randomized into the study interventions, Fig. 1. Of these subjects enrolled in the study, 60 were men and 23 were women, with a mean age of 59 years (SD 12.73) and an Apnoea–Hypopnoea Index (AHI) of 48.50 (SD 18.32). Of these, 79.5% were married and the academic level with the highest percentage of subjects was primary school (39.8%). In terms of employment status, the percentages of subjects in active employment and retired subjects were similar (47% and 45.8%, respectively). Table 3 provides full descriptive characteristics of the subjects by group.
Demographic and clinical characteristics of included subjects.
| Variable | Total | MEntA | Control | p-value |
|---|---|---|---|---|
| Sex | ||||
| Male | 60 (72.3%) | 32 | 28 | 0.422 |
| Female | 23 (27.7%) | 10 | 13 | |
| AHI | 48.50 (18.69) | 46.30 (18.80) | 49.95 (17.85) | 0.368 |
| Civil status | ||||
| Single | 5 (6%) | 3 (60%) | 2 (40%) | 0.279 |
| Married | 66 (79.5%) | 30 (45.5%) | 36 (54.5%) | |
| Widow | 9 (10.8%) | 7 (77.8%) | 2 (22.2%) | |
| Divorced | 3 (3.6%) | 2 (66.7%) | 1 (33.3%) | |
| Academic level | ||||
| No studies | 6 (7.2%) | 4 (66.7%) | 2 (33.3%) | 0.207 |
| Primary | 33 (39.8%) | 18 (54.5%) | 15 (45.5%) | |
| Secondary | 22 (26.5%) | 13 (59.1%) | 9 (40.9%) | |
| University | 22 (26.5%) | 7 (31.8%) | 15 (68.2%) | |
| Employment situation | ||||
| Active | 39 (47%) | 20 (51.3%) | 19 (48.7%) | 0.993 |
| Unemployed | 6 (7.2%) | 3 (50%) | 3 (50%) | |
| Retired | 38 (45.8%) | 19 (50%) | 19 (50%) | |
| ESS | 11.64 (4.67) | 10.35 (4.53) | 13.02 (4.29) | 0.007 |
| Age | 59.45 (12.73) | 61.35 (13.11) | 57.51 (12.19) | 0.182 |
| Motivation: score 0–3 | 1.65 (0.87) | 1.66 (0.90) | 1.51 (0.92) | 0.443 |
| Perceived competence (CEPCA) | ||||
| OSA information: 1–4 | 1.34 (1.25) | 1.47 (1.40) | 1.17 (1.04) | 0.263 |
| CPAP knowledge: 1–5 | 0.87 (0.75) | 0.85 (0.75) | 1.00 (0.80) | 0.406 |
| CPAP use: 1–4 | 0.42 (0.52) | 0.42 (0.54) | 0.41 (0.50) | 0.904 |
| Total | 2.63 (1.50) | 2.76 (1.66) | 2.58 (1.28) | 0.591 |
| Health related outcomes | ||||
| QoL: 1–10 | 5.25 (1.57) | 5.07 (1.89) | 5.31 (1.44) | 0.508 |
| Emotional state: 0–2 | 1.06 (0.62) | 1.09 (0.65) | 0.97 (0.61) | 0.393 |
| Daily activities: 0–2 | 0.95 (0.71) | 1.00 (0.73) | 0.90 (0.70) | 0.537 |
| Social relationship: 0–2 | 1.07 (0.69) | 1.09 (0.65) | 1.02 (0.72) | 0.641 |
Qualitative data in frequencies and percentages (in brackets). Cuantitative data in means and standard deviation (in brackets). AHI: Apnea–Hypopnea Index. ESS: Epworth Sleepiness Scale. CPAP: continuous positive airway pressure. OSA: sleep apnoea/hypopnoea syndrome. CEPCA: Questionnaire of Evaluation of Perceived Competence in Adherence to CPAP in OSA. QoL: Visual Analogical Well-being Scale for apnoea.
The randomization properly balanced the groups in terms of their baseline conditions, both at the demographic level and the clinical characteristics and severity of the symptoms, which were initially measured by the various scales used in the study. Only an imbalance was found on the ESS and university education. No statistically significant differences were observed between the groups in terms of their baseline condition for the rest of variables.
One subject interrupted the treatment without providing data at either of the study's two cut-off points, while two subjects provided data at the 30-day point only. The three subjects were part of the study's control group.
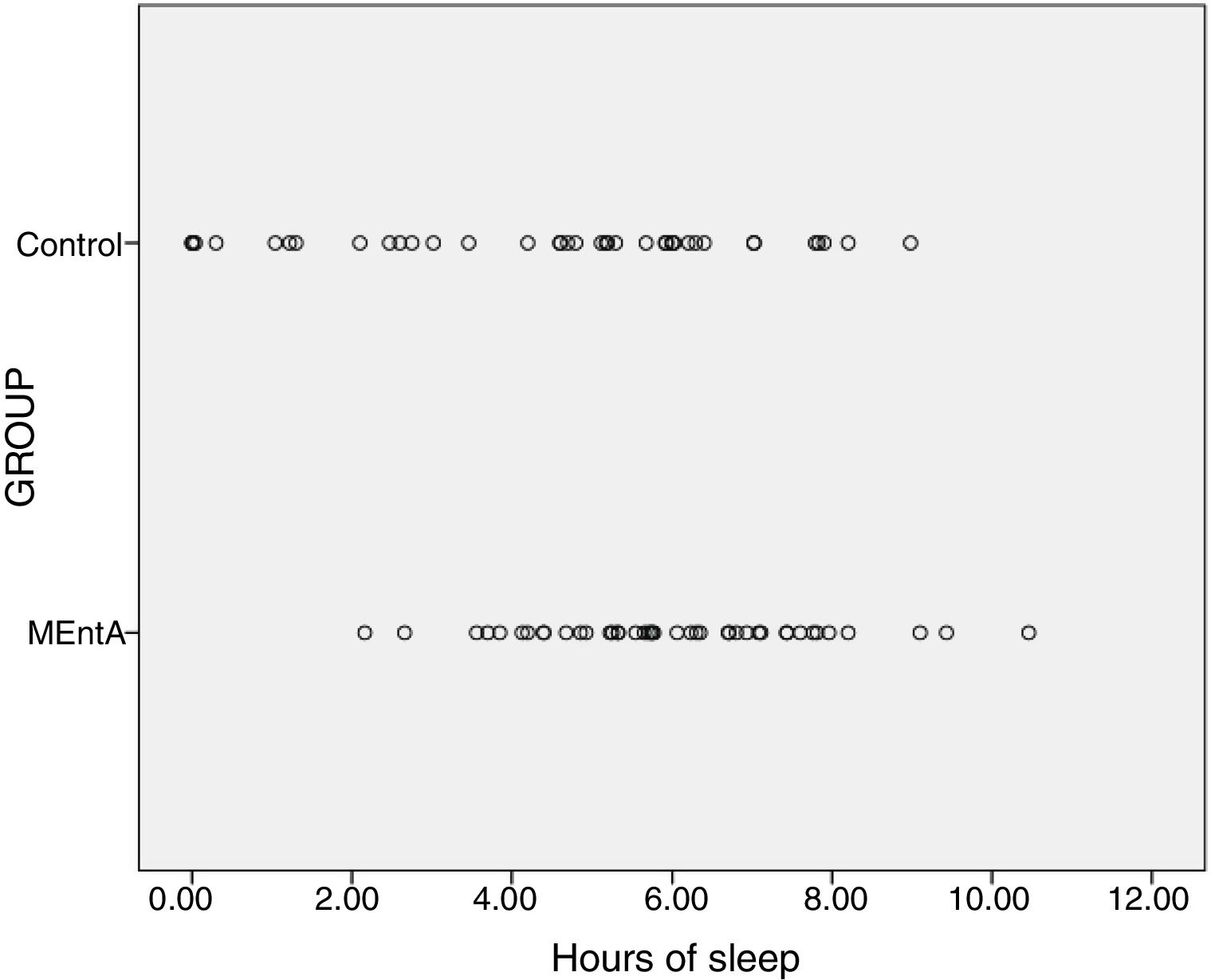
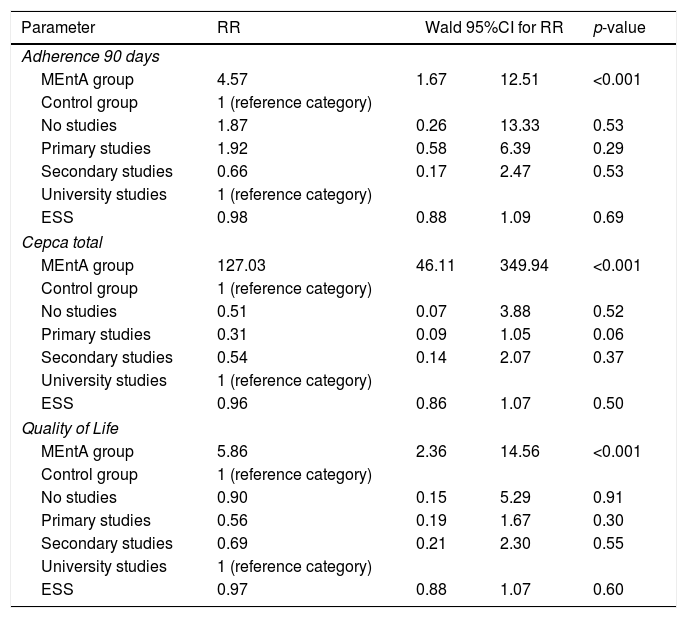
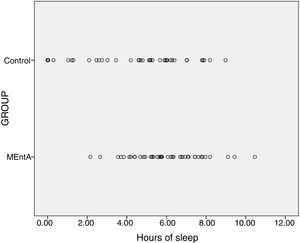
EfficacyFor the main outcome (treatment adherence after 90 days of follow-up), statistically significant results were obtained in favor of the interventional arm with the MEntA assessment (p<0.01), with a mean difference of 1.60h (95% CI, 0.60 to 2.61) (see Fig. 2). Meanwhile, there were not yet any significant differences observed between the study arms at 30 days with a mean difference of 0.48h (4.63 vs 4.15h) (95% CI −0.69 to 1.67) (p=0.413). The adjusted analysis for the main outcome, including the baseline imbalances variables, showed same results and a RR up to 4.57 (95% CI, 1.67 to 12.51) (p<0.001) in favor of the MEntA group. It means that the risk of higher values was more than four times for MEntA group in comparison to the control group while no statistically significant differences were observed for the baseline unbalances variables (see Table 4 for adjusted analysis).
Adjusted results for the main outcomes including the imbalance baseline variables. Generalized lineal model.
| Parameter | RR | Wald 95%CI for RR | p-value | |
|---|---|---|---|---|
| Adherence 90 days | ||||
| MEntA group | 4.57 | 1.67 | 12.51 | <0.001 |
| Control group | 1 (reference category) | |||
| No studies | 1.87 | 0.26 | 13.33 | 0.53 |
| Primary studies | 1.92 | 0.58 | 6.39 | 0.29 |
| Secondary studies | 0.66 | 0.17 | 2.47 | 0.53 |
| University studies | 1 (reference category) | |||
| ESS | 0.98 | 0.88 | 1.09 | 0.69 |
| Cepca total | ||||
| MEntA group | 127.03 | 46.11 | 349.94 | <0.001 |
| Control group | 1 (reference category) | |||
| No studies | 0.51 | 0.07 | 3.88 | 0.52 |
| Primary studies | 0.31 | 0.09 | 1.05 | 0.06 |
| Secondary studies | 0.54 | 0.14 | 2.07 | 0.37 |
| University studies | 1 (reference category) | |||
| ESS | 0.96 | 0.86 | 1.07 | 0.50 |
| Quality of Life | ||||
| MEntA group | 5.86 | 2.36 | 14.56 | <0.001 |
| Control group | 1 (reference category) | |||
| No studies | 0.90 | 0.15 | 5.29 | 0.91 |
| Primary studies | 0.56 | 0.19 | 1.67 | 0.30 |
| Secondary studies | 0.69 | 0.21 | 2.30 | 0.55 |
| University studies | 1 (reference category) | |||
| ESS | 0.97 | 0.88 | 1.07 | 0.60 |
RR: relative risk. ESS: Epworth Sleepiness Scale. CEPCA: Questionnaire of Evaluation of Perceived Competence in Adherence to CPAP in OSA. QoL: Visual Analogical Well-being Scale for apnoea.
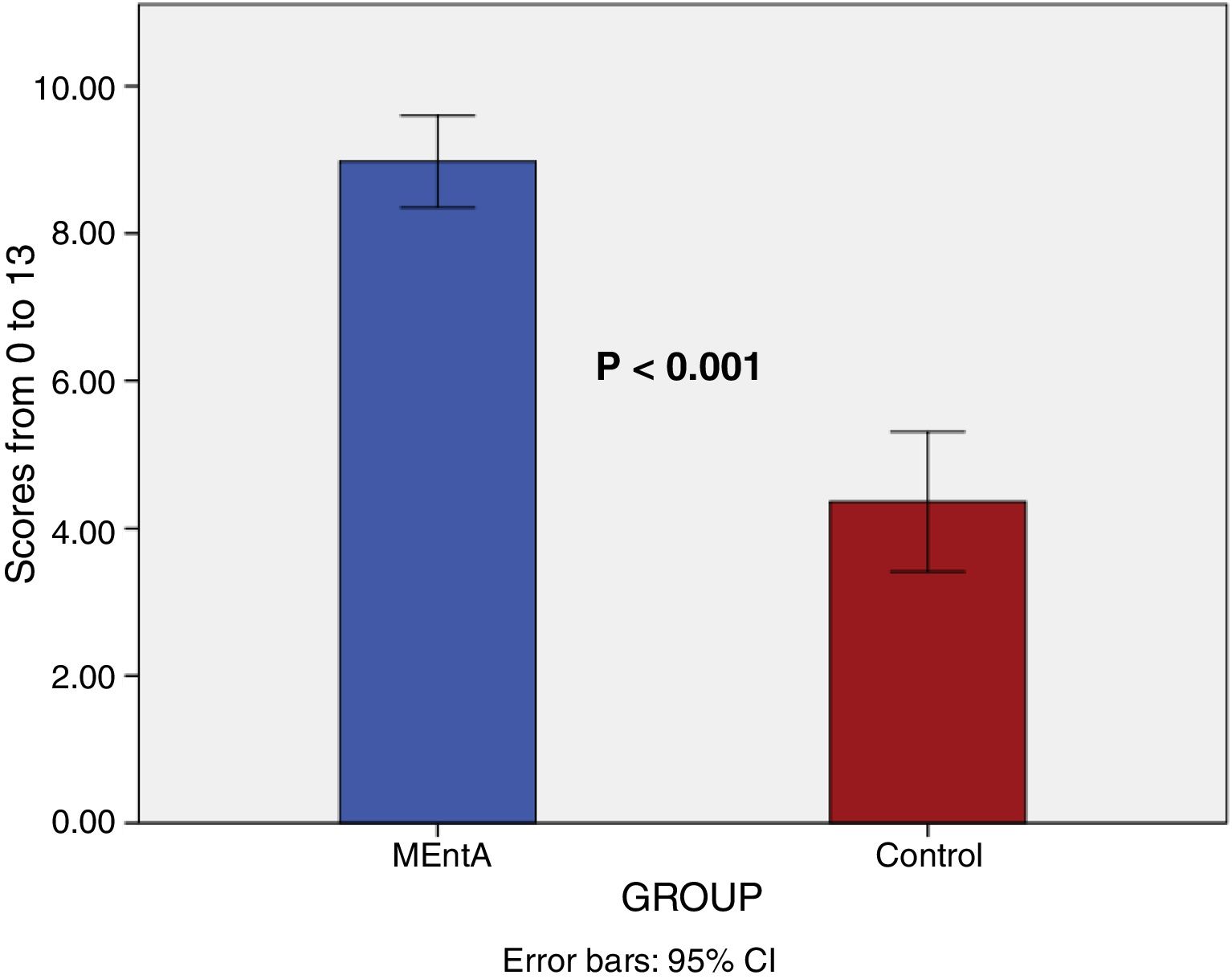
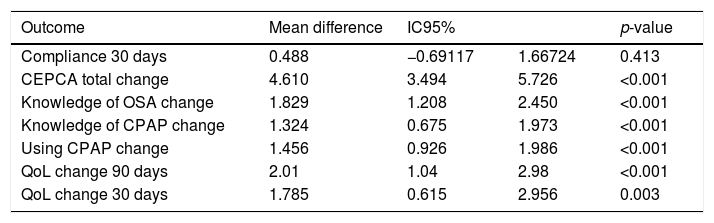
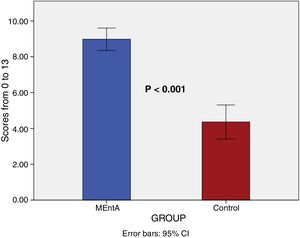
The results obtained for the CEPCA Questionnaire show a statistically significant change, from baseline to the end of follow-up at 90 days, when comparing the two study arms, in favor of the MEntA intervention (p<0.001) with a mean difference of 4.61 (95% CI, 3.49 to 5.72) for all of the factors measured (means by groups 11.73 vs 6.95). Fig. 3 and Table 5 for secondary outcomes. When analyzed separately by factors, statistical significance was observed in favor of the MEntA intervention for all of these: knowledge of OSA (p<0.001), treatment expectations (p<0.001) and overcoming obstacles associated with using the intervention (p<0.001) (Table 5). Statistically significant differences were also observed in favor of the intervention being evaluated when comparing this variable's final outcomes between the two study arms (p<0.001). The adjusted analysis adding the baseline imbalance variables showed a high-risk value of improvement for MEntA group RR 127.02 (95% CI, 46.11 to 349.94) (p<0.001) (see Table 4).
Secondary outcomes.
| Outcome | Mean difference | IC95% | p-value | |
|---|---|---|---|---|
| Compliance 30 days | 0.488 | −0.69117 | 1.66724 | 0.413 |
| CEPCA total change | 4.610 | 3.494 | 5.726 | <0.001 |
| Knowledge of OSA change | 1.829 | 1.208 | 2.450 | <0.001 |
| Knowledge of CPAP change | 1.324 | 0.675 | 1.973 | <0.001 |
| Using CPAP change | 1.456 | 0.926 | 1.986 | <0.001 |
| QoL change 90 days | 2.01 | 1.04 | 2.98 | <0.001 |
| QoL change 30 days | 1.785 | 0.615 | 2.956 | 0.003 |
| Outcome | Mean rank difference | Sum diff. | p-value |
|---|---|---|---|
| Non-parametric test | |||
| Motivation 90 days | 18.46 | 808 | <0.001 |
| Motivation Change 90 days | 10.94 | 496 | 0.032 |
| Outcome | X2 value | p-value |
|---|---|---|
| Qualitative variables | ||
| Emotional state 30 days | 10.101 | 0.006 |
| Daily activities 30 days | 7.227 | 0.027 |
| Social relationship 30 days | 5.899 | 0.052 |
| Emotional state 90 days | 6.079 | 0.048 |
| Daily activities 90 days | 4.755 | 0.093 |
| Social relationship 90 days | 11.139 | 0.004 |
CEPCA: Questionnaire of Evaluation of Perceived Competence in Adherence to CPAP in OSA. QoL: Visual Analogical Well-being Scale for apnoea.
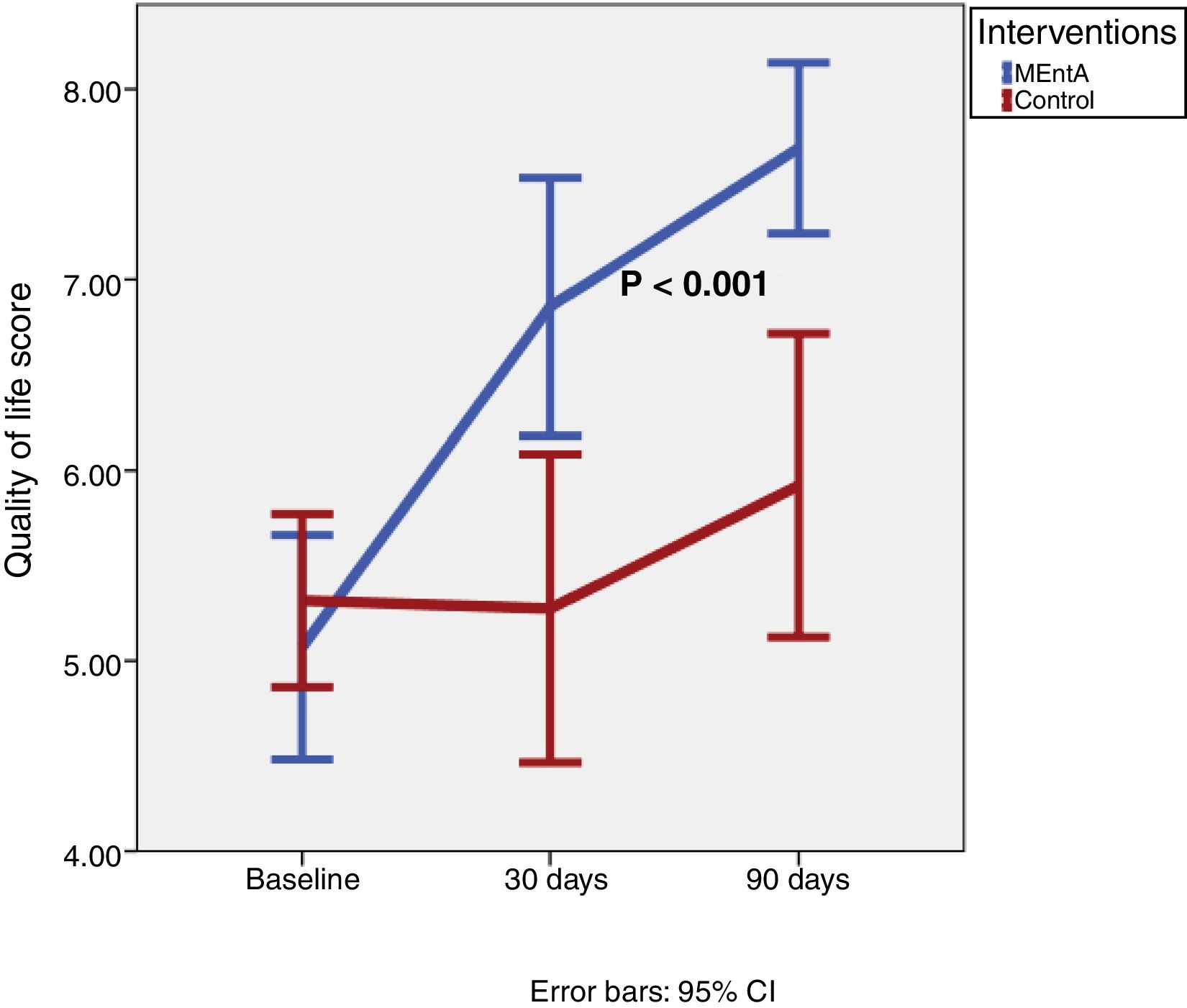
For the quality of life variable, measured using the Visual Analogical Well-being Scale, a statistically significant change was also observed in favor of the intervention being evaluated when compared to the follow-up at 30 and 90 days (p<0.001) for both cut-off points and for both the change from baseline and the final outcomes. Means by groups: 7.69 vs 5.92 to 90 days; 6.85 vs 5.27 to 30 days (see Fig. 4 and Table 5). Likewise, for motivation, according to the Prochaska and DiClemente transtheoretical model, when comparing the change from baseline to the end of follow-up between the two arms, a statistically significant difference was observed for the MEntA arm (p=0.032) as well as comparing both groups at the end of the follow up period (p<0.001) (Table 5). The adjusted analysis including imbalances baseline variables showed similar results with a RR up to 5.86 (95% CI, 2.36 to 14.56) (p<0.001) (Table 4). No statistically significant differences were observed for sleepiness when comparing the before-after change between the treatment arms (p>0.05) after 90 days of follow-up, but there were statistically significant differences found when comparing the final outcomes between the two study groups, with a mean difference in favor of the MEntA arm of −3.17 (95% CI, −4.70 to −1.65) after 90 days of follow-up (means by groups 4.19 vs 7.36). Although this effect may be due to the basal imbalance found.
When comparing final outcomes between the two groups, a statistically significant difference was observed between the two study arms for the emotional state variable (poor, normal or better), at 30 and 90 days (X2 10.101, p=0.006; X2 6.079, p=0.048 respectively) and for social relationships at 90 days (X2 11.139, p=0.004). Also, there were differences at 30 days for daytime activities variable (X2 7.227, p=0.027) (Table 5).
No side effects or adverse events related to the interventions studied were observed during the follow-up period.
DiscussionThis study, based on an experimental design and with the aim of comparing a new training model for patients with OSA receiving CPAP therapy, has found solid evidence that this training, based on motivational interviewing and proper feedback, achieves a higher level of efficacy in adherence to treatment, quality of life, emotional state, self-efficacy and motivation of patients, when compared to a standard training intervention.
Intervention with CPAP is the first-line treatment in patients with OSA, having shown efficacy in both moderate and more severe stages of the disease.13 Therapeutic alternatives such as surgery may be considered only in cases in which this technique cannot be applied, or the patient does not agree to it. However, there is less evidence on the efficacy of surgery in different subject profiles, in addition to its invasive nature.14 Alternatives to surgery include neurostimulation of the hypoglossal nerve in an attempt to increase muscle tone at the end of the tongue, and medication with 5-HT-receptor molecules, as well as controlling habits which could increase the severity of the disease, such as smoking, obesity and taking muscle relaxants.15,16
Nevertheless, despite the intervention with CPAP being considered the first-line treatment and the solid evidence of its benefit, the level of adherence with this therapy is still undergoing constant study. This may be due to the fact that, over the past 20 years, the percentage of subjects who did not complete 7h of night-time sleep with this intervention has remained constant, with failure to comply with 7h/night in 34.1% of patients with an average duration of 4.6h/night.17 These figures must be improved, as a high level of use of CPAP is associated with better scores in the sleep scales and, as a result, fewer daytime symptoms, even when comparing with subjects with support in sleep hygiene habits and daily activities.18 In some studies19,20 it has been shown that optimal adherence is related to better outcomes, such as sleepiness, quality of life or blood pressure.
As such, the results of our study show how an intervention based on motivational interviewing, as part of a specific program, maintains adherence to the therapy for three months. The intervention in the control group loses its efficacy at 30 days while it remains in the MEntA group. This is possibly the main benefit of the motivational interview, since it allows the involvement of the patient who adheres to the therapy from a different perspective: not because it is a prescribed treatment, but because he is motivated.
This therefore has an effect on improving the clinical conditions and day-to-day lives of the subjects. This psychological approach is based on patient-focused management to help them explore and resolve any ambivalence.21 The principles of this are empathy, developing patient discrepancies, avoiding confrontation between the therapist and the patient, in order to prevent the patient becoming defensive and working on resistance to change and perceived self-efficacy for the subject.4
In addition, motivational interviewing has a broad field of study and is an effective tool in the area of healthcare. This has allowed for an improvement in adherence to taking medication and an increase in physical activity for subjects with chronic diseases.22,23 It has also proven to be effective in acquiring healthy behavioral habits such as quitting smoking and maintaining and improving oral hygiene habits, with an increase of up to five times the frequency of brushing teeth with this intervention compared to a standard healthcare educational intervention.24,25 The technique has also shown efficacy, in relevant response measures, in subjects with HIV, such as a reduction in depression and risky sexual behavior.26,27 In the case of CPAP therapy in patients with OSA, clinical trials show evidence of a benefit when comparing motivational interviewing or motivational enhancement with the standard care for this type of patient, with a 50% increase observed in adherence to the interventions after three, six and twelve months, compared to the control group.4,7 Our work demonstrates the effectiveness of the use of motivational interviewing in the Spanish context within the model of home respiratory therapies that currently exists in Spain, more focused on technical, device and training aspects, and not so much on care issues. Nevertheless, the MEntA educational program that has been studied has been applied in groups (CPAP Schools) obtaining good results. In response to the growing number of patients diagnosed with OSA, this methodology favors the sustainability of the system without diminishing the benefits for the patient.
In our study, the intervention was based on an educational and training program to which the principles of motivational interviewing were added, which we have called MEntA, in an attempt to change the patients’ perceptions on the difficulty of use, the risks and their ability to use the technique. The results found, when compared to a control group with standard training in subjects who were naïve to CPAP therapy, showed not only benefits in adherence to this intervention, but also in the basic processes which lead to successful adherence with the therapy. Perceived self-efficacy and competence are fundamental factors for maintaining adherence to a treatment, as has been shown in our study. Likewise, conclusive results were obtained for relevant patient reported outcomes (PROs) such as quality of life, which significantly increased for the MEntA group after both 30 days and 90 days, as well as motivation, emotional state and even social relationships. These factors are closely related to the efficacy of the CPAP therapy and, therefore, to its proper adherence by patients.28
The expected results in the long term are a reduction in dropouts, since adherence is explained by reasons of motivation and self-efficacy, and not so much by adaptation.
Regarding the limitations of this work, we focused on short-term results, up to 90 days. The next step will be to know the impact of this educational and training program in the medium and long term. Although we know that the first 3 months in CPAP treatment are crucial and predictive of how adherence will be in the long term, we do not know if MEntA could have an impact on maintaining and optimizing the use of therapy. Another question to address in futures studies is that knowing that you are participating in a study suggests that there may be something about implicit knowledge of experimental group membership and additional nurse time, which may increase overall involvement. Another limitation was found in the sample, since there were differences in the level of sleepiness measured with the Epworth Scale. Regarding the inference of results to the reference population, one of the limitations of our study is also that it is considered single-center design.
To summarize, the MEntA intervention included as part of an educational and training program for patients with OSA for proper adherence with OSA therapy shows solid results in terms of its efficacy. These results are based on maintaining adherence to the treatment, which involves an improvement in the clinical variables and PROs, which are highly relevant in the day-to-day lives of these patients.
Conflict of interestThe authors declare to have no conflict of interest directly or indirectly related to the manuscript contents.