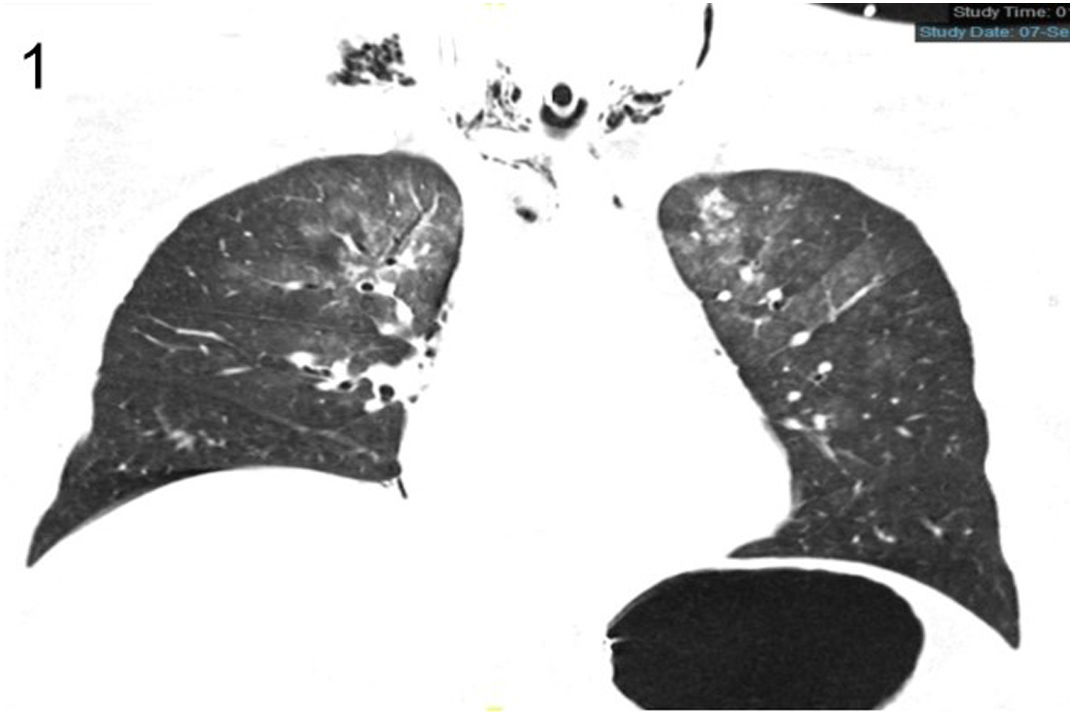
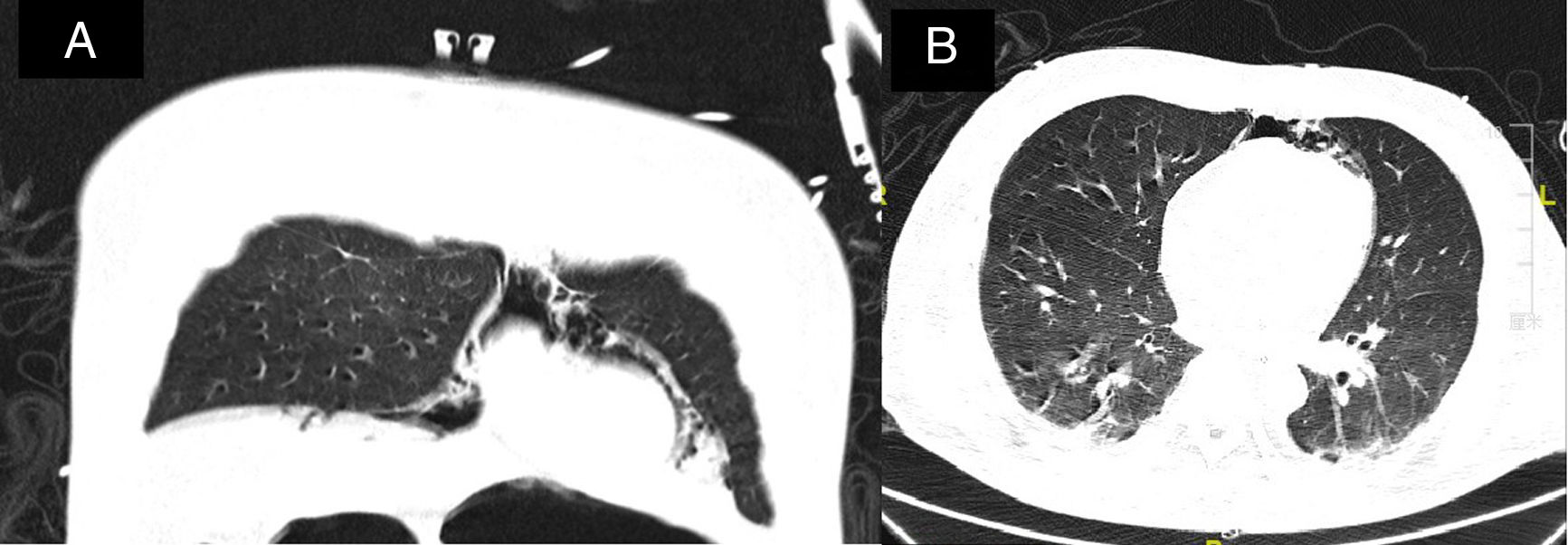
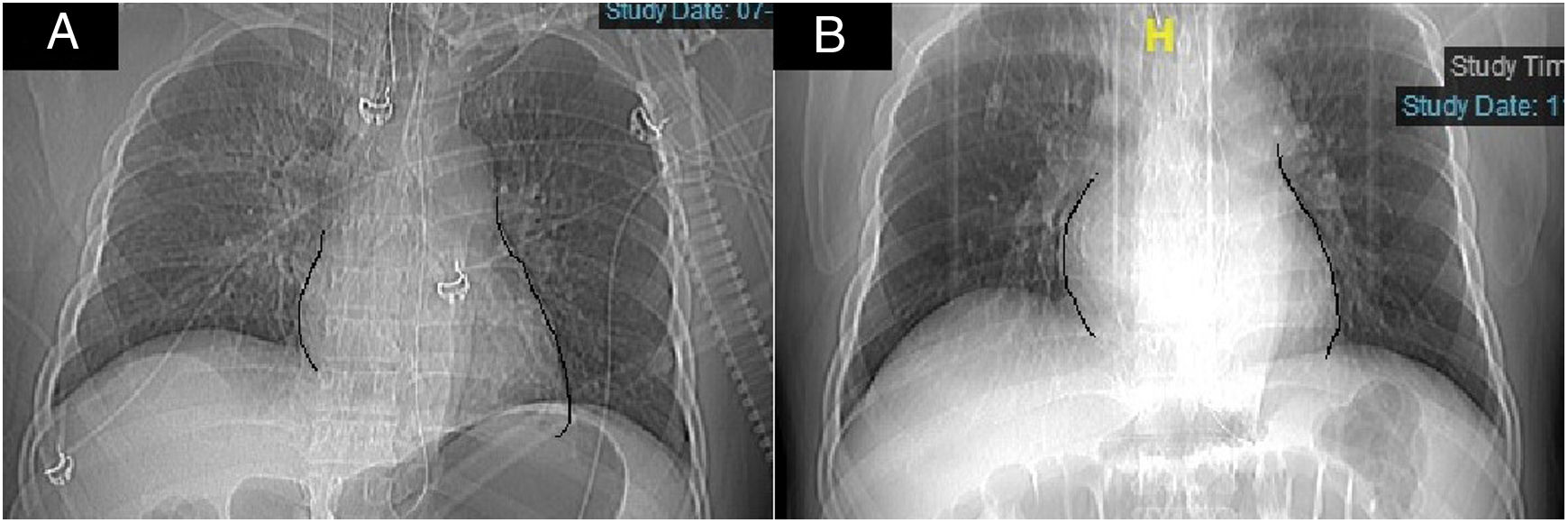
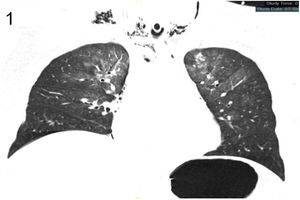
A 42 years old man was admitted to stomatology hospital on August 2019 due to relapse of gingival cancer (GC). As treatment procedures, patient received surgery and tracheostomy at the same time. After surgery, patient's condition was stabilized, incision of the neck appeared to be in the first stage of wound healing process and decannulation was done. On the night before discharge, patient appeared to be suffered from sudden dyspnea, unconsciousness and seizures, so emergency tracheostomy was performed, and patient was immediately transferred to Intensive Care Unit (ICU). In the process, patient suffered from transient hypotension, and ventilation via the stoma was administered. Patient didn’t receive Ambu mask during reanimation. On admission, patient's PO2 level was 100mmHg, patient had undergone CT scan and result shows that present of pneumomediastinum accompanied with subcutaneous emphysema (Figs. 1 and 2), and pulmonary embolism was excluded. Pneumomediastinum following tracheostomy is a rare occurrence, which has a percentage of 0.36 of incidence reported.1 Reviewing back his medical history, patient did complaint of chest distension 2 days ago before the onset of this scenario, and when emergency tracheostomy was performed, a lot of bubbles were seen. Therefore, we believe that there is a possibility that maybe after decannulation, pneumomediastinum was slowly formed which is very rare in the absence of positive airway pressure, and gradually compresses the heart, leading to obstructive shock, thus, when tracheostomy was performed again, patient's condition returned stabilized. CT reveals that pneumomediastinum compress the heart and lead to formation of Earth-Heart sign (Fig. 3).2 Patient return consciousness on the second day, he did a follow-up on CT scan after 5 days and result shows that pneumomediastinum and subcutaneous emphysema were completely absorbed.
Consulte los artículos y contenidos publicados en este medio, además de los e-sumarios de las revistas científicas en el mismo momento de publicación
Esté informado en todo momento gracias a las alertas y novedades
Acceda a promociones exclusivas en suscripciones, lanzamientos y cursos acreditados