The professional dedicated to respiratory health has an exemplary role in tobacco control, promoting smoking cessation in their patients. However, multiple circumstances cause a low implementation. Therefore, the objective of the study is to identify the consumption, knowledge and perception of tobacco and its emerging products in a representative sample of professionals involved in the treatment of respiratory patients integrated into the Spanish Society of Pneumology and Thoracic Surgery (SEPAR).
Material and methodsDescriptive analysis of a structured online interview addressed to 5340 SEPAR members.
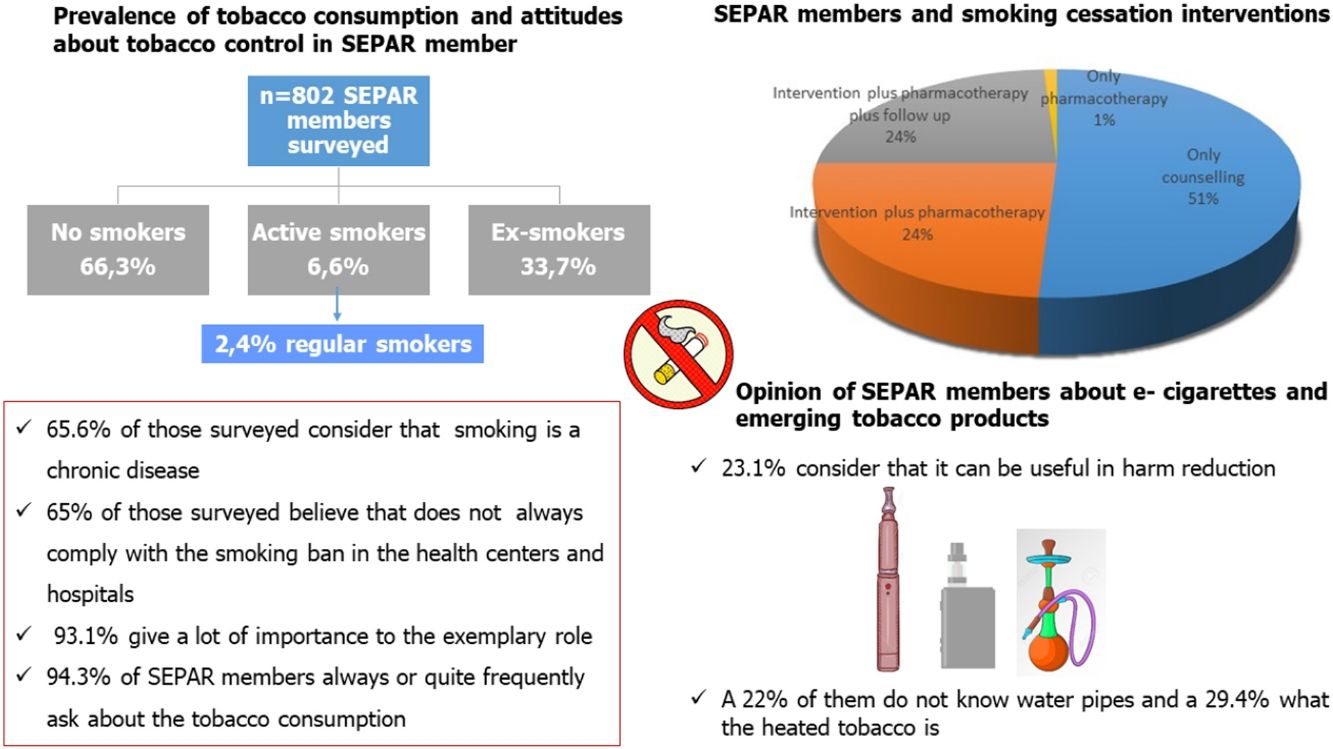
ResultsIn a sample of 802 respondents, more than 33% have smoked at some time and 6.6% continue to smoke. More than 66% consider smoking as a chronic disease. More than 90% consider their role model important and advise their patients to quit smoking, but less than half carry out a smoking intervention. Only 35% of them believe that the ban on smoking in health centers is always complied. More than 75% do not consider nicotine delivery devices an option for smoking cessation or harm reduction. 22% are unaware of water pipes and 29% of heated tobacco.
ConclusionsProfessionals specialized in respiratory diseases are highly sensitized to smoking. Despite this, there are still weak points such as the insufficient implementation of smoking cessation interventions or the scant training in smoking and in new emerging products.
El profesional dedicado a la salud respiratoria tiene un papel ejemplar en el control del tabaquismo, promoviendo el abandono del hábito tabáquico en sus pacientes. Sin embargo, múltiples circunstancias provocan una baja implementación. Por tanto, el objetivo del estudio es identificar el consumo, el conocimiento y la percepción sobre el tabaco y sus productos emergentes en una muestra representativa de profesionales implicados en el tratamiento de pacientes respiratorios integrados en la Sociedad Española de Neumología y Cirugía Torácica (SEPAR).
Material y métodosAnálisis descriptivo de una entrevista estructurada en línea dirigida a 5.340 miembros de la SEPAR.
ResultadosEn una muestra de 802 encuestados, más del 33% ha fumado alguna vez y el 6.6% sigue fumando. Más del 66% considera el tabaquismo como una enfermedad crónica. Más del 90% considera importante su modelo a seguir y aconseja a sus pacientes que dejen de fumar, pero menos de la mitad realiza una intervención para dejar de fumar. Solo el 35% de ellos cree que la prohibición de fumar en los centros de salud se cumple siempre. Más del 75% no considera que los dispositivos de suministro de nicotina sean una opción para dejar de fumar o reducir los daños. El 22% desconoce las pipas de agua y el 29% el tabaco calentado.
ConclusionesLos profesionales especialistas en enfermedades respiratorias están altamente sensibilizados al tabaquismo. A pesar de ello, aún existen puntos débiles como la insuficiente implantación de intervenciones para dejar de fumar o la escasa formación en tabaquismo y en nuevos productos emergentes.
Smoking is the leading preventable cause of death and loss of quality of life worldwide.1–3 In response, since 2003 a set of measures have been promoted. One of them is to offer help to the smoker from a health professional, who plays an exemplary role in the smoking habit.4 Thus, physicians who smoke have less likely to promote smoking cessation by their patients. However, according to some review, 21% continue to smoke.5 One of the most committed sectors to this epidemic is dedicated to the care of respiratory patients. The Spanish Society of Pneumology and Thoracic Surgery (SEPAR), which brings together this group, has been a leader in the fight against smoking developing initiatives to detect the prevalence, perception and knowledge of tobacco among its members developing several surveys throughout its history.6,7
However, in recent years there have been several important events with regard to this epidemic:
- a)
The emergence of electronic cigarettes and heated tobacco (IQOS®) as methods to stop smoking or minimize the harm of tobacco.8,9
- b)
The acquisition of other forms of consumption such as waterpipes.10,11
- c)
The passivity in the application of measures in Spain to control smoking.12
- d)
The funding of drugs for nicotinic dependence (varenicline, bupropion and cytisine).13–15
- e)
The COVID-19 pandemic has prioritized care to this disease, temporarily closing the stop smoking services. Besides, the pandemic also took a heavy toll on the mental health of professionals and in the population general, which facilitated the consumption of tobacco.16–19
For all these reasons, it is necessary to update the prevalence data and knowledge of the smoking among SEPAR members, incorporating new aspects such as the opinion about emerging tobacco products.
Material and methodsBetween June 1 and October 31, 2022, a structured interview was sent periodically with an on-line methodology to all SEPAR members. The questionnaire consisted of 21 questions about smoking habits, knowledge, attitudes in aspects related to tobacco control as the electronic cigarettes and heated tobacco. They are included demographic and anthropometric variables, specialty belonging to the respondent, importance of the role model, type of smoking cessation treatment, training received or perception about electronic cigarettes and heated tobacco as useful tools for smoking cessation or harm reduction. In the subgroup of smokers, the degree of smoking, the nicotine dependence, motivation and previous quit attempts were analyzed.
The sample size was calculated by the number of SEPAR members registered in May 2022 (5340). Thus, in order to achieve a representative sample, the objective was to reach the 380 respondents to achieve a precision of 4.86. For statistical analysis, we used the IBM SPSS version 22 software. Categorical variables were calculated using contingency tables expressing the values in frequencies and percentages. Continuous variables were analyzed using means and standard deviations. The comparative analysis was carried out using the Chi-square tests and Fisher's test for categorical variables. The continuous variables were compared using Student t-tests, ANOVA, Mann–Whitney, or Kruskal–Wallis, according to their normal distribution fit as assessed by the Kolmogorov–Smirnov test. A value of p<0.05 was considered as statistical significance.
The completion of this survey was approved by the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR). All information was treated confidentially in accordance with the current Organic Data Protection Law.
ResultsThe number of surveys conducted was significantly higher than that calculated number (802). As a consequence, the margin of sampling error decreased to 3.19% with a 95%CI. This level of sampling error was calculated knowing the total population, the number of respondents and the confidence interval. The percentage of participants of the total number of SEPAR members by specialties was the following: 12.4% pulmonologists, 40.06% nurses, 18.9% physiotherapists, 3.1% of thoracic surgeons and 7.1% pediatric pulmonologists. In conclusion, a sample was obtained representative of the group of SEPAR members in terms of disciplines, workplaces and sociodemographic characteristics.
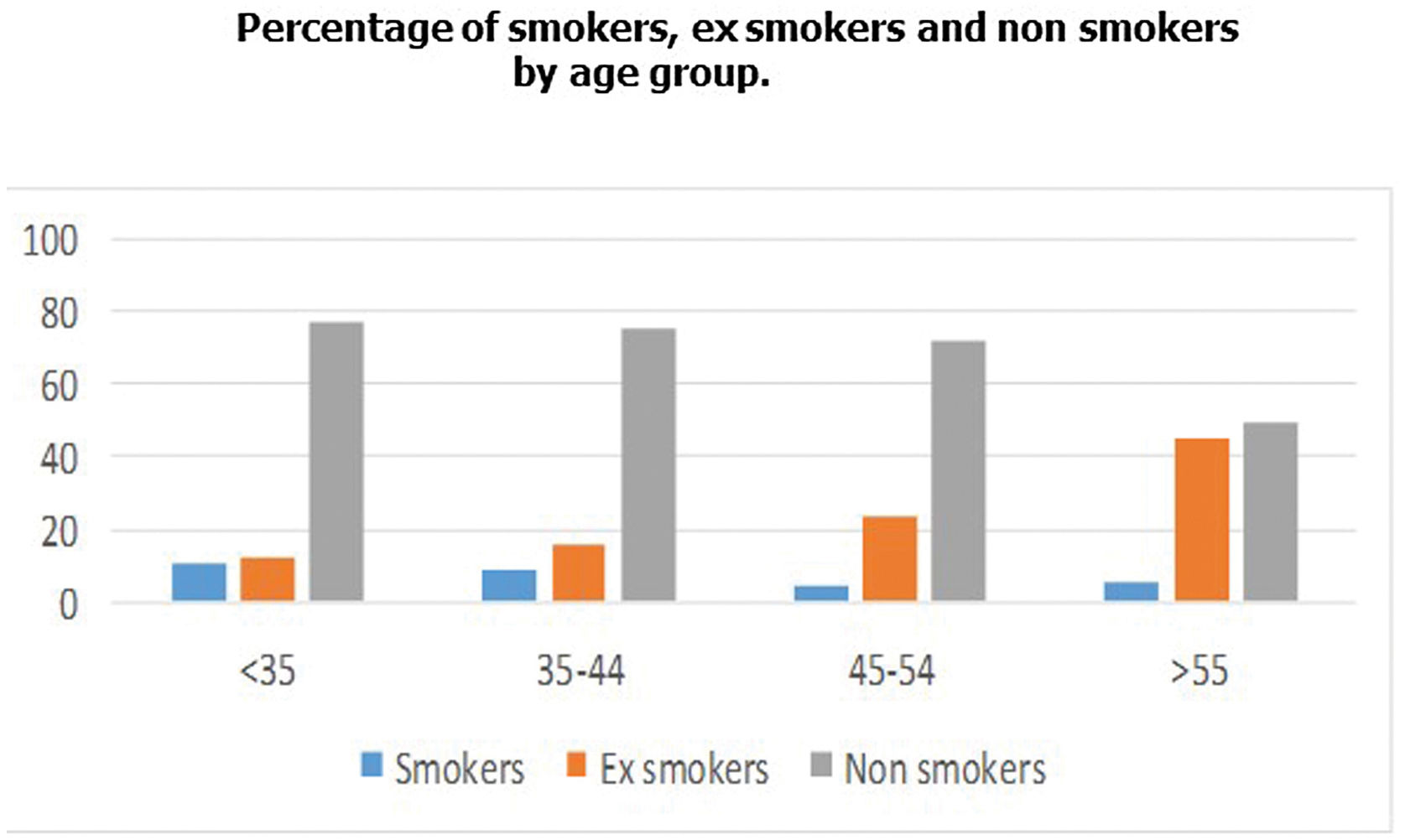
Of the 802 members surveyed, 36.8% were male and 63.2% female. The average age is 54±5.2. The distribution of the sample by age ranges was as follows (<35 years: 16.6%, 35–44 years: 22.9%, 45–54 years: 26.8% and over 55 years 33.4%).
Prevalence of smoking in SEPAR members33.7% CI 95% (30.4–36.9)% of respondents reported having smoked on some occasion in their life, while 66.3% CI 95% (63.1–69.6)% answered that they had never smoked. The percentage of smokers among those surveyed was 6.6% (95 CI 4.3–7.6) (2.5% were regular smokers and 4.1% occasional). The distribution of smoking is shown in Figs. 1–3.
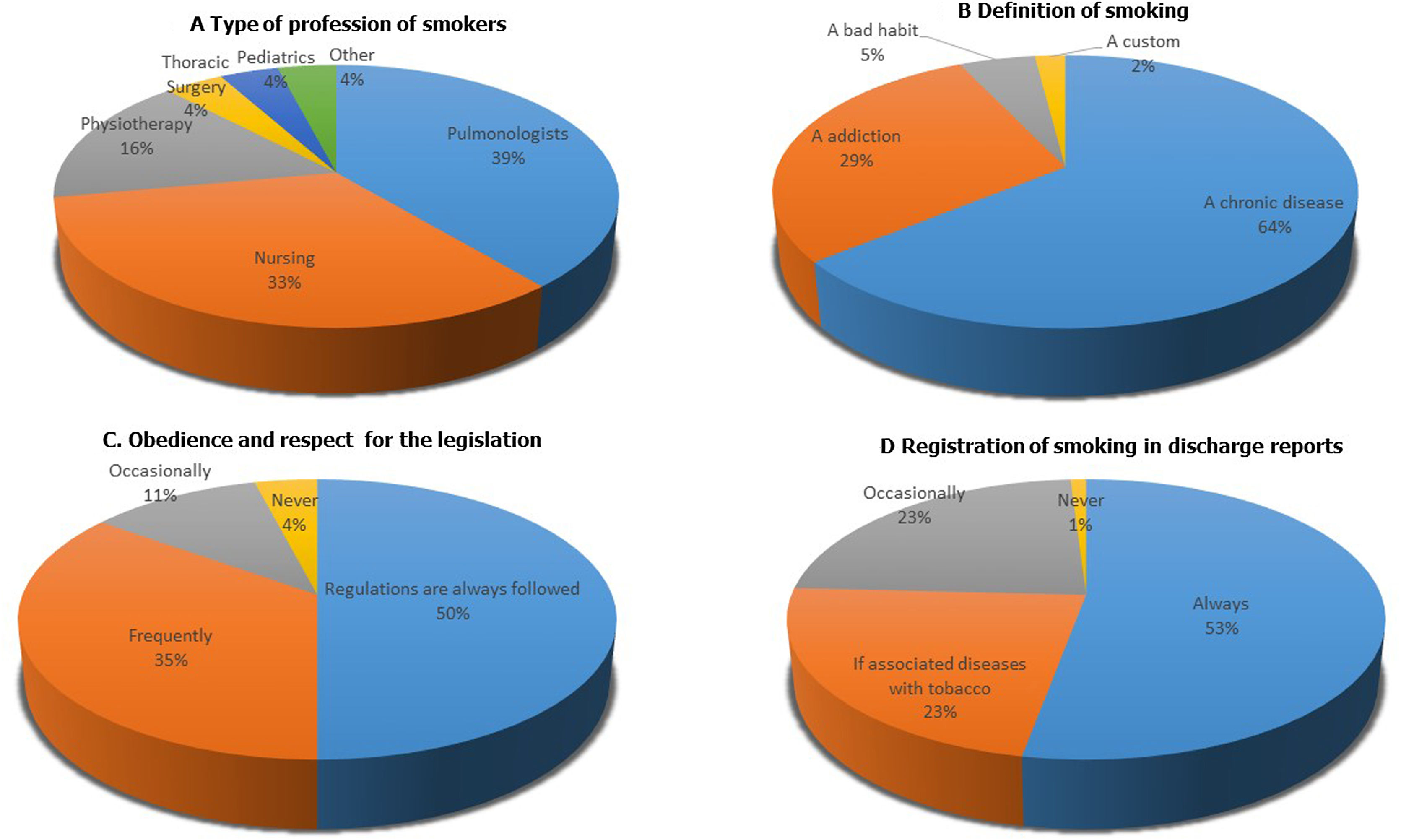
Of the 53 smokers surveyed, 66% are women and 34% men. 39.2% are pulmonologists, 33% nurses and 15.7% physiotherapists (Fig. 4A). The median age is 48±12 years. Mostly, they started smoking between the ages of 16 and 20 (60%).
In addition, they had a low degree of smoking (63% smoke less than 4 cigarettes a day) and a low dependence on nicotine (66% of the smokers members surveyed turn on their first cigarette 60min after waking up). The mean FTCD score (Fargerström Test Cigarette Dependence) was low (1.31±2.03).
63.2% of the smokers surveyed considered that it is important to quit smoking, with an average score of 9.5 out of 10 points, being slightly higher at ages 45–54 years (7.20±3.29) and in females (9.24±1.17).
Most smokers have previously tried to quit, 45.8% influenced by their condition as a health professional. More than 75% of smokers have been without smoking for more than 6 months. Almost 20% of these smoke at their workplace.
Attitude of SEPAR members regarding the implementation of legislation, registration of the tobacco use and smoking cessation interventionsDefinition of smoking65.6% of those surveyed consider that smoking is a chronic disease (Fig. 4B). This opinion grows as the age of the surveyed increases (70.9% between 45 and 54 years and 67% in those over 55 years; p=0.002). Pulmonologists and nurses are the health professionals who most frequently consider smoking as a chronic disease (72% and 59% respectively; p<0.001).
Obedience and respect for the legislation in force65% of those surveyed believe that does not always comply with the smoking ban in the health centers and hospitals (Fig. 4C). The elderly (44%) and physiotherapists (60%) are the members who most often think that the smoking ban is always respected in these.
The role model function93.1% give a lot of importance to the exemplary role, especially in older than 45 years (95%), in pulmonologists, nursing and trainee pulmonologists (in 90% of cases).
Questions and recording on tobacco use94.3% of SEPAR members always or quite frequently ask about the tobacco consumption in particular in older members (more than 85% in those over 55 years of age) in men (82.8%) and in pulmonologists (95%). Only 52.5% always record the smoking habit in the discharge report (Fig. 4D).
Attitude of SEPAR members toward smoking cessation interventions95.6% of members always advise their patients to quit smoking and more than 70% give a very high importance to the counseling. The youngest members are who attach the least importance to a counseling (55% in those under 35 years of age vs 65% in those over 55 years of age; p<0.001). Regarding the type of smoking cessation intervention, 50.8% of the respondents recommend only counseling and 48.4% counseling plus drugs (23.8% psychological counseling plus drugs and 24.6% adding to the above 6-months follow-up).
The most frequent attitude of the respondent toward a smoker is to refer to a Smoking Cessation Unit in 49.8% compared to 40.3% who decides for themselves to treat the disease with psychological counseling and drugs (Fig. 5A).
Opinion of the undergraduate and postgraduate training in smoking received by SEPAR members39.8% of SEPAR members had not received training in smoking during their postgraduate term and 38.9% little training (Fig. 5B).
During their undergraduate studies, 66.1% had no training in smoking and 29.2% had little training.
Perception of SEPAR members regarding electronic cigarettes and emerging tobacco products76.6% consider that the electronic cigarette is neither effective nor helps to minimize the toxic effects of tobacco. However, 23.1% consider that it can be useful to reduce in harm reduction. The pulmonologists (26% of them) are the discipline most likely to support these devices (Fig. 5C). A quarter of SEPAR members are unaware of emerging tobacco products. A 22% of them do not know water pipes and a 29.4%what the IQOS® is. The youngest members are the ones with the greatest lack of knowledge of these products (by 34.6% and 33% respectively) (Fig. 5D).
DiscussionThe results of this survey show a low prevalence of smoking in the professional dedicated to respiratory health care, with a collaborative attitude toward this problem. However, training in smoking cessation and knowledge of on new tobacco products could be improved. The most relevant findings are discussed below.
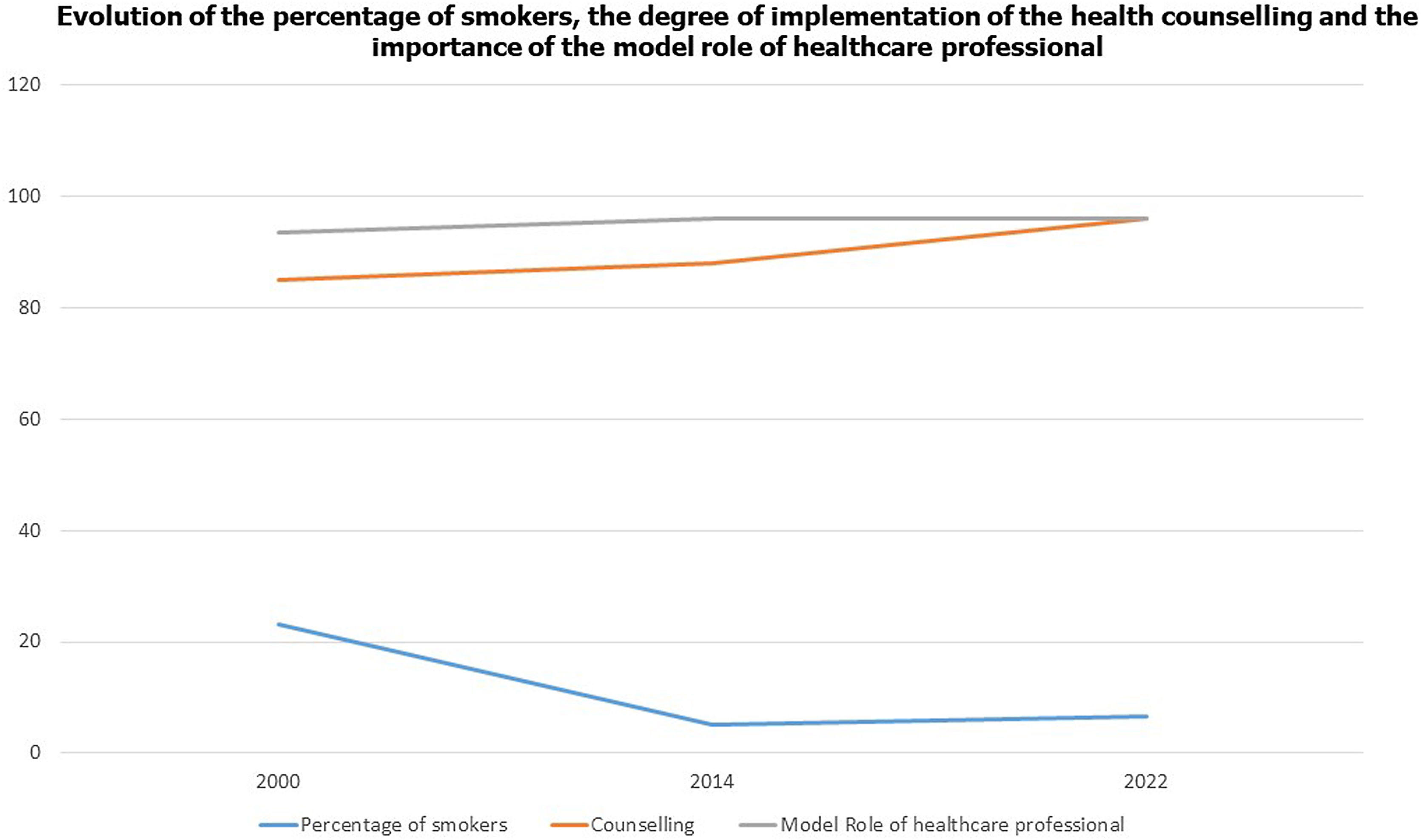
Prevalence of active smokingThe SEPAR member is characterized by being sensitized to smoking. It is known model role in the face of this disease, associating it with a greater probability of smoking cessation.5–7 Active tobacco use remains low compared to other surveys with a prevalence of 21% similar to general population.5,12,20 Despite these optimistic results, an increase of 1.6% is observed compared to previous surveys of these health professionals.7 This increase could be justified by the reduction in interest in smoking, the high workloads of respiratory health professionals motivated by the COVID-19 pandemic and the relaxation in the last 10 years in the application of measures tobacco control in our country.12,16,17 Also, the appearance of new tobacco products could encourage young respiratory health professionals to start in tobacco use.9 Pulmonologists continue to be the specialists who have fewer smokers. However, there is a worrying increase of smoking in non-pulmonology professionals compared to previous surveys.7 This increase reflects on the need to involve these groups more intensively in smoking cessation activities. In addition, they spend a great deal of time in contact with the smoker patient and their smoking quitting interventions can be decisive.
Another very worrying fact is that 10.6% of SEPAR members between the ages of 25 and 35 are smokers, reducing the percentage in this age group who have never smoked to 77.3%, 6% less than in previous surveys.7 On the other hand, the percentage of women smokers is higher. These results reflect the general trend observed in the general population in recent years, with a gradual incorporation of women and adolescents to tobacco consumption.6,7 When analyzing the subgroup of smokers, we observed, as in previous studies, a low physical dependence on nicotine (FTCD score less than 4 points) and a high motivation for quitting (more than 50% of the responders mark motivations equal to or higher than 8 points).
Compliance with laws in the workplaceIi is worth noting that 65.4% of those surveyed believe that their healthcare center does not always comply with the smoking ban. Similar results were found in a survey addressed to the general population from the Spanish Society of Family Medicine and Community (SEMFyC).21
Tobacco use registration and specific approach to smokingAlthough more than 90% of the professionals ask about tobacco consumption to their patients, up to 20% of them do not do it systematically. We observe an increase 7% among SEPAR partners who admit that they do not always ask their patients about the smoking habit.7
One of the pessimistic data obtained is that only 52.5% of the SEPAR members register of tobacco consumption in a medical records. These findings contrast with other studies showing a record of tobacco use in 68%.22 The systematic electronic recording of smoking habits through notification systems would improve these results.23
Although for more than 80% of those surveyed the combination of a pharmacological and a psychological approach is considered the most effective intervention for the treatment of tobacco addiction, its implementation is poor. Counseling is the most commonly used strategy (with an increase of 8% compared to the 2016 survey).7 These data objectify the importance that it has for the professional SEPAR this form of intervention, observing rates of implementation of this superior to other specialties.24 This can be attributed to the greater perception that the SEPAR professional has of the damage caused by the tobacco. However, less than half carry out in their practice usual more intensive approaches, opting to refer directly to the smoking units. However, if when we compare these data with those of the 2014 survey, the largest number of professionals who prescribe drugs (current 49% vs. previous 43%), reducing by 10% the referral to specific consultations.7 According to recent bibliography, among the factors that determine the absence of implementation of psychological counseling and treatment pharmacology of smoking quitting in professionals involved in respiratory are: the lack of training in smoking cessation, the length of the interview with the patient or erroneous beliefs about nicotine addiction.25 These obstacles are overcome by intensifying training in smoking, facilitating accessibility to pharmacotherapy by non-physician professionals or introducing smoking cessation protocols.23
Perception of smoking as a diseaseOne of the most relevant results of this survey is the decrease in the perception of smoking as a chronic disease, being considered or as a psychological addiction or a bad habit, opinions that exceed 30% of the respondents.
This conception has increased with respect to the 2014 survey (34.5% vs. 21%). These misperceptions pose a danger to the care of patients who smoke for various reasons: on the one hand, there is a risk of not giving them the attention they really require, since we must not forget the scope of the approach of smoking as a powerful, highly cost-effective measure.13–15 On the other hand, the ignorance of the chronicity of smoking and the failure to consider relapses as natural event of smoking cessation causes doubts about this type of intervention.25,26
Smoking cessation trainingAccording to SEPAR members, training in smoking cessation is referred to as scarce, both in the undergraduate and postgraduate periods. These results are common and overlapping with other studies published in the literature.27–29
Therefore, the development of attractive training strategies represents a point of improvement reinforcing the Expert Course in Smoking Cessation with a basic course for residents and healthcare professionals not involved on a daily basis in smoking, a rotation program in Excellence Stop Smoking Units and a university master's degree in training in this disease.30 On the other hand, the publication of the consensus document SEPAR on the standards of training in smoking cessation in the faculties of Medicine represents progress for such implementation.31
Perception of new tobacco and nicotine productsAs regards emerging tobacco products more than 20% of the SEPAR members are unaware of them, as is a review that analyzes knowledge of these devices in different specialists.32 This should make us reflect on increasing training in smoking and extend it to resident doctors and non-medical professionals.30,31
Most of the SEPAR members consider the release devices nicotine as products that are not safe, effective, or minimize the harm of tobacco. These findings are in line with current studies.32 However, in a recent review, 38% of physicians had recommended to the patient the electronic cigarette as a method to stop smoking or reduce the harm.24 The lowest percentage of respondents who consider electronic cigarettes as form of smoking cessation is attributable to the carried out by SEPAR through 2 statements about devices and emerging products of the tobacco and a recent review on the use of these as a strategy to reduce damage.8,9 However, more than 20% of SEPAR members consider the electronic cigarettes as a useful strategy to minimize tobacco harm. All this would be associated with the demotivation or low training in smoking cessation interventions that induces think of these methods as an alternative.26 Similar reviews in other countries show practically overlapping results,33–35 which should lead us to reflect on training deficiencies as well as the tobacco industry's messages.
In Fig. 3 we represent over a period of 20 years the changes in the prevalence and SEPAR member's attitudes toward smoking. It was observed between the year 2000 and 2020 a significant decrease of 18.2% in the number of SEPAR member smokers. During this period several important events took place focused on the prohibition of smoking in public spaces. In addition, the role of SEPAR was decisive in increasing the interest of its members in this epidemic. In recent years, COVID-19 and new tobacco products and nicotine together with the passivity of the Administrations in the face of this problem can justify this slight increase in smokers. Also, recently there have been new members belonging to new categories have been incorporated into SEPAR with a higher incidence of smoking. A positive fact is the increase in the last years of counseling among SEPAR members (Fig. 6).
As strengths, this article offers a vision of the healthcare professional that takes care to patients with pathologies associated with tobacco incorporating as a novel aspect his perception of new products and nicotine delivery devices. It not only includes pulmonologists, but also health professionals. It is a survey carried out in Spain using the on-line methodology which provides the health professional with more time to complete it, flexibility and possibility of accessing more people. Also, it compares the results with previous surveys assessing the effect of the different actions carried out in Spain against smoking. As weak points, the percentage of response to the survey stands out (15%) that would correspond to more motivated professionals. The data of participation are similar to previous ones, with the number of respondents being higher than estimated for the calculated sampling error.
ConclusionsThe percentage of smokers is low among SEPAR members. However, its implication can be improved. It is necessary to develop a strategy whose purpose is to train in smoking cessation to the healthcare professionals and motivate to intervene against this disease through programs based on incentives and recognition of their work with a subsequent evaluation of the effectiveness of these actions.
ApprovalWe confirm that the manuscript has been read and approved by all the cited authors. In addition, we confirm that the order of authors that appears in the manuscript has been approved by all. On the other hand, we have given due consideration to the protection of individual property associated with this work and that there are no impediments to its publication.
FundingNone of the authors have received funding.
Authors’ contributionsAll authors contributed equally to the conception, writing, revision, and final approval of the manuscript.
Conflicts of interestCAJ-R has received honoraria for presentations, participation in clinical studies and consultancy from: Aflofarm, Bial, GSK, Menarini and Pfizer.
RPP has received fees for presentations and publications from: Astra Zeneca, Boehringer-Ingelheim, Bial, Chiesi, Esteve, Ferrer, GSK and Novartis.
JIG-O has received fees for speaking, scientific consulting, clinical study participation, or publication writing for the following: Astra Zeneca, Chiesi, Esteve, Faes, Gebro, Menarini, and Pfizer.
EPE: You have received fees for presentations and collaborations for training from: Aflofarm, Bial, Chiesi, Faes, Ferrer, Novartis and Pfizer.
SS-R declares no conflict of interest.
IGU declares having received fees for presentations from: Aflofarm, Pfizer, Chiesi, Menarini.
RMB declares that he has no conflict of interest for this work.
EH-M has received fees for presentations, conferences and courses sponsored by: Astra-Zéneca, Bial, Boehringer, Chiesi, Esteve, Faes Farma, Ferrer, GSK, Mundiphasrma, Menarini, Novartis, Pfizer and Rovi.
JAR-M has received scientific consulting and/or speaking fees from Aflofarm, Astra-Zeneca, Bial, Boehringer Ingelheim, Chiesi, GSK, Menarini, Mundipharma, Novartis, Pfizer, Rovi, and Teva.
MRP declares that it has no conflict of interest for this work.
FGR has received honoraria as a speaker or consultant from AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Menarini, Novartis, Pfizer, and Rovi, and research grants from Chiesi, Esteve, Gebro Pharma, GlaxoSmithKline, Menarini, and TEVA.
CR-C has received honoraria for speaking engagements, sponsored courses, and participation in clinical studies from Aflofarm, GSK, Menarini, Mundipharma, Novartis, Pfizer, and Teva.