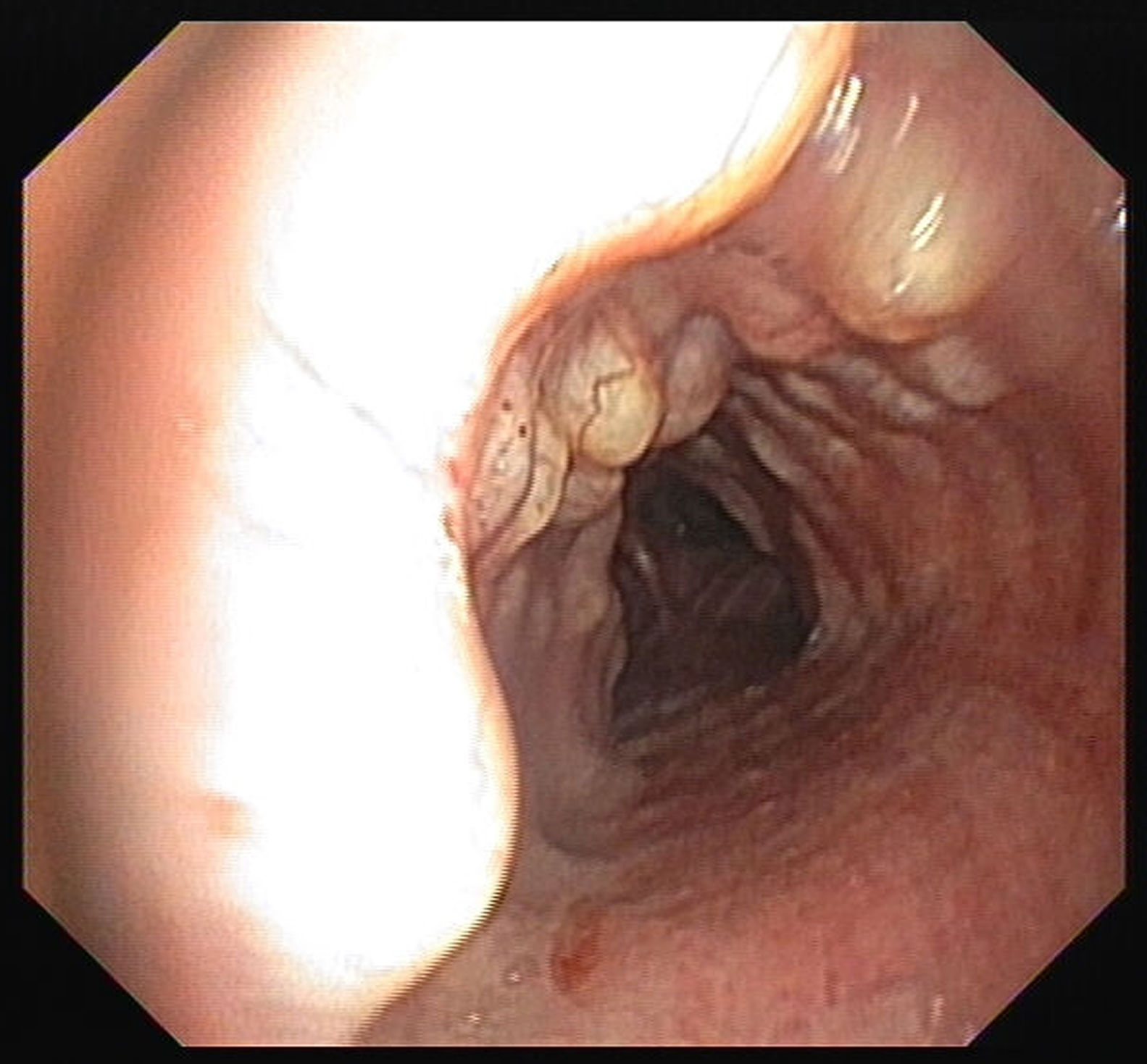
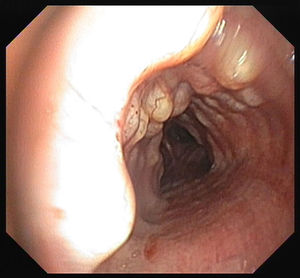
A 68-year-old woman had an incidental imaging finding in a chest computed tomography. She was a former smoker with no respiratory symptoms. Chest computed tomography revealed tracheal and left bronchus anterior wall irregularity with polypoid lesions. At bronchoscopy multiple hard consistency nodules were seen along the anterior wall of the tracheal mucosa extending to the left main bronchus (Fig. 1). This appearance was suggestive of tracheobroncopathia osteochondroplastica. Several biopsies of the lesions were performed confirming the diagnosis.
Tracheobroncopathia osteochondroplastica is a benign rare disease of unknown etiology.1 It is characterized by the presence of multiple submucosal osteocartilaginous nodules that involve luminal surfaces of anterior and lateral walls of the tracheobronchial tree, sparing the posterior wall.2 It is usually asymptomatic, but symptoms like chronic cough, dyspnea, wheezing and, occasionally, hemoptysis can occur. In most cases, it is an accidental finding that bronchoscopists should easily identify, as images are themselves often diagnostic. Nevertheless, biopsies are relevant to the exclusion of other differential diagnosis.1 The prognosis is favorable and treatment is aimed at symptoms relief or when patients develop serious complications like tracheal and/or bronchial stenosis or hemoptysis.1,2