Patellofemoral instability is a common cause of knee disability. Acute patellofemoral dislocation is the most common acute knee disorder in skeletally immature patients. In this group, the incidence of patellofemoral dislocation is approximately 43 per 100,000 individuals.
The precise objective addressed in the paperMedial patellofemoral ligament (MPFL) reconstruction has a significant role in the treatment of patellofemoral instability in skeletally immature patients. We evaluated the medium and long-term results results of MPFL reconstruction as the sole method of patellofemoral instability treatment and their relationship with the presence of other potentially associated factors.
MethodsWe conducted a prospective study with 35 young patients who underwent the same surgical technique between 2002 and 2009. Age, gender, patellar tilt, patella height, TT-TG, trochlear dysplasia, the Kujala score and the Tegner activity score were evaluated. Statistical analysis used SPSS® 20.
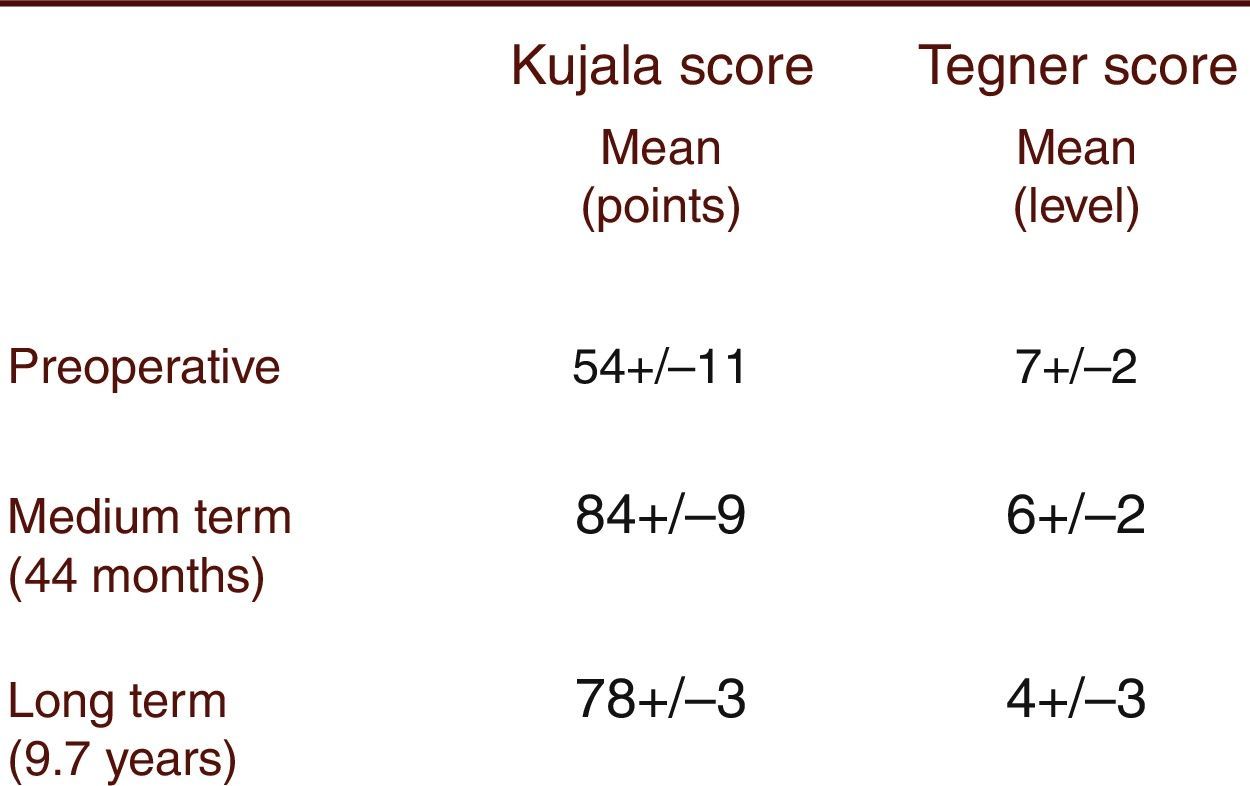
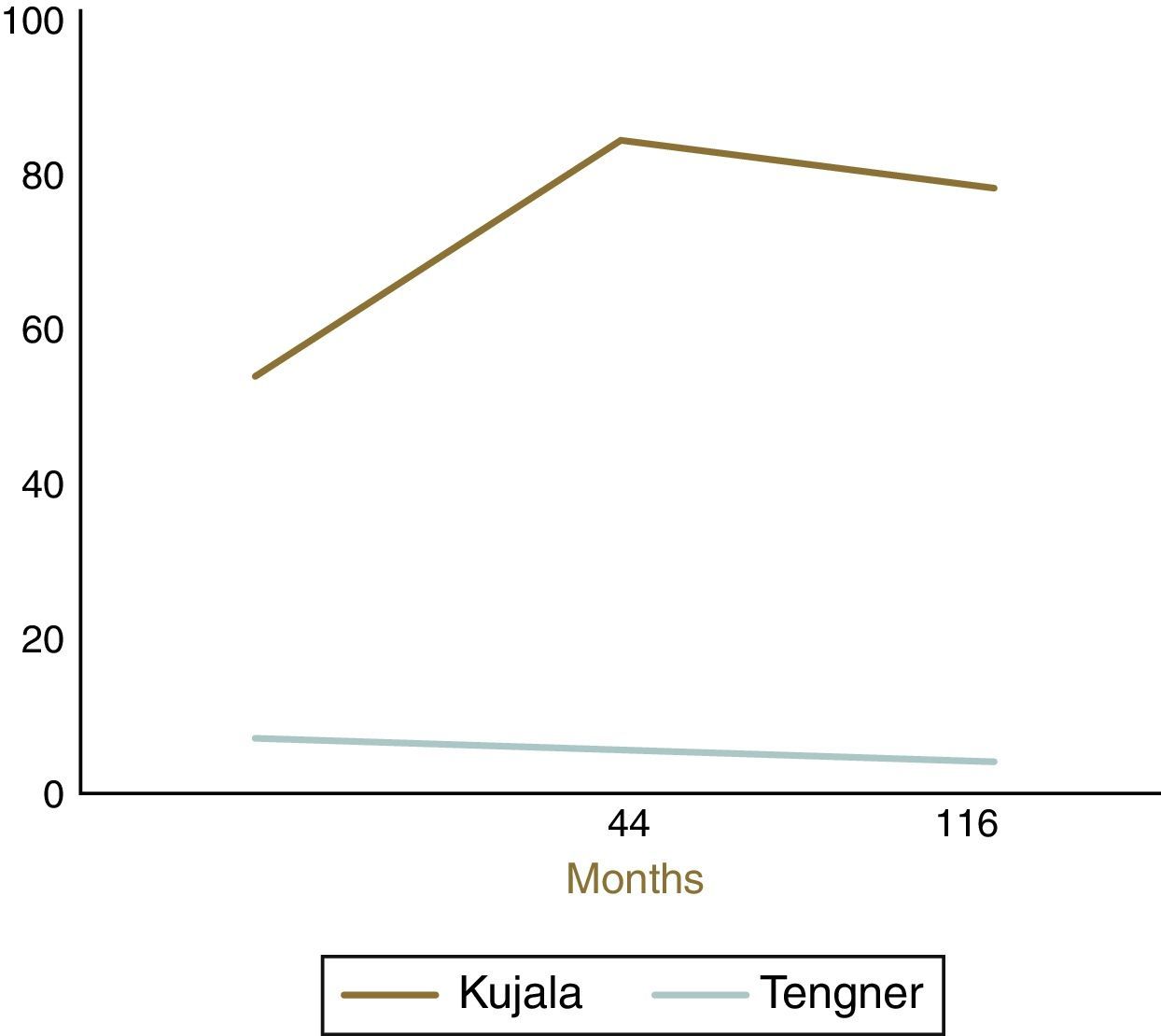
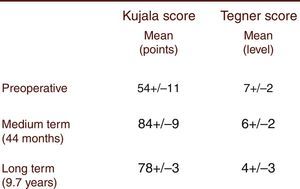
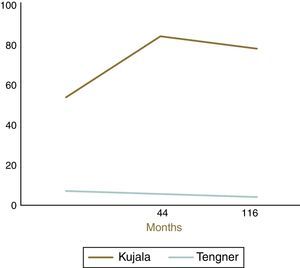
ResultsThe mean age of the patients was 15.9 years. High patella was observed in 10% of patients. All patients had TT-TG within a normal range. Trochlear dysplasia was found in 80% of the patients: 40% had Dejour's type A; 34% type B; 20% type C and 6% type D. The medium-term Kujala score (84±9) significantly improved compared to the pre-operative score (54±11). However, a decline in the long-term (78±3) score was observed. The Tegner activity score showed a significant decrease. The long-term results were significantly lower when patients had trochlear dysplasia type B to D.
ConclusionsA decade after isolated MPFL reconstruction, results remained satisfactory. Patients with trochlear dysplasia types B to D may benefit from associated trochleoplasty in a second intervention.
Acute patellofemoral dislocation is the most common acute knee disorder in skeletally immature patients. In this group, the incidence of patellofemoral dislocation is approximately 43 per 100,000 individuals.1 After a first episode, 33% of patients continue to feel pain or a feeling of the knee giving-way; these substantially impair the physical performance of patients. Previous studies report redislocation rates ranging from 15 to 44% following a first-time dislocation.2 After a first-time patellar dislocation and in the absence of associated injuries such as an osteochondral fracture, an avulsion of the vastus medialis obliquus or a meniscal tear, nonoperative treatment is recommended.3 The most common indications for surgical treatment are failure to improve with physical rehabilitation and repeat dislocations.3 Multiple surgical techniques have been described in order to solve instability, regarding its multifactorial pathoanatomy.4–6 The surgical approach must be individualized for each patient and may address all contributing factors; therefore, no single surgical technique corrects all problems. Surgical options for individuals with open physes include (1) proximal realignment, (2) distal realignment, (3) lateral release, (4) medial patellofemoral ligament (MPFL) reconstruction, (5) guided growth with tension-band plates, or a combination of the procedures. Osteotomies of the proximal part of the tibia and the distal end of the femur are not indicated in this age group because of the risk for damage to growth areas and axial deviations.7–9
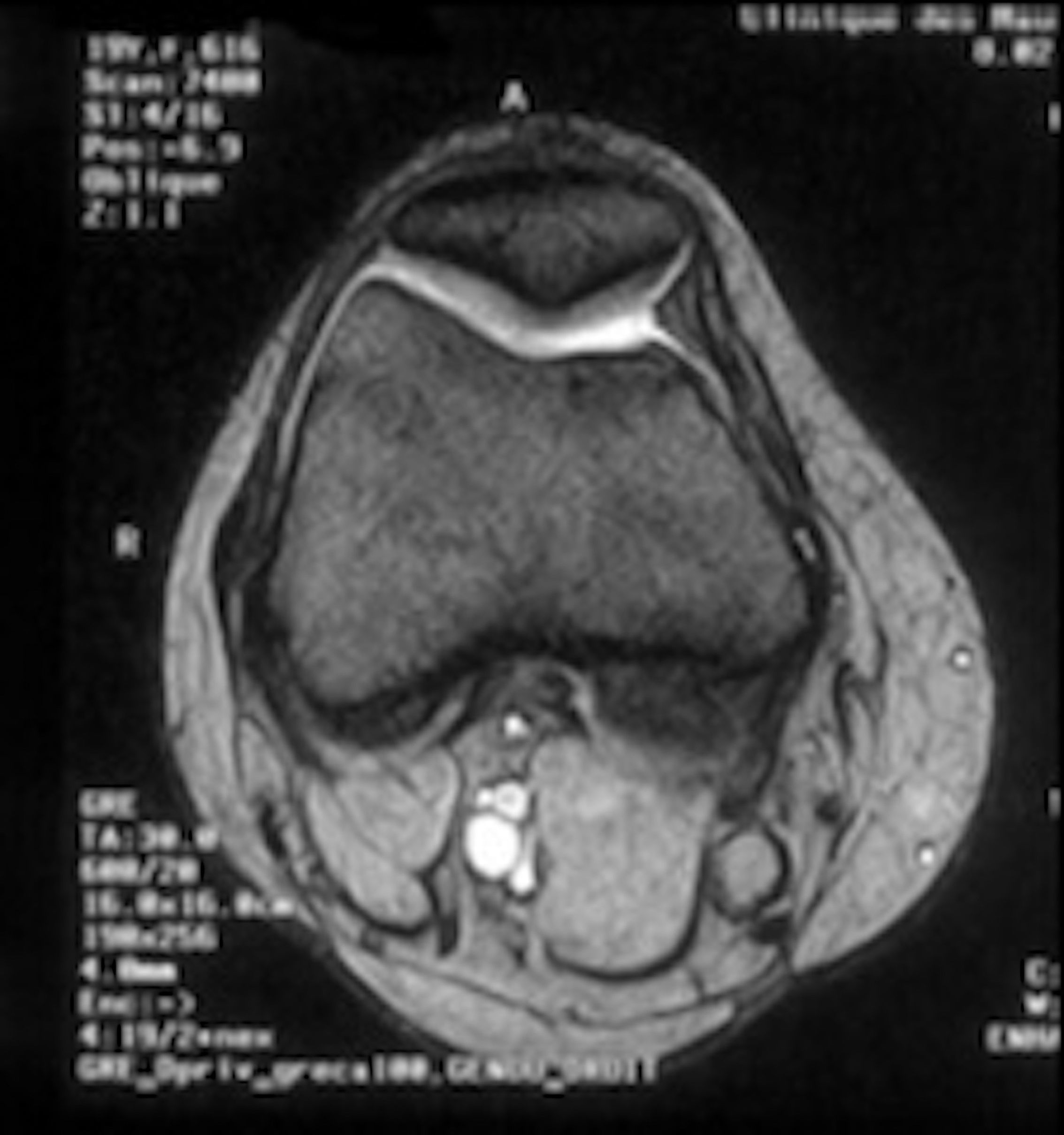
Conlan et al. performed a biomechanical study of the relative contributions of the medial soft-tissue restraints in the prevention of lateral displacement of the patella.9 They found MPFL (Fig. 1) to be the major medial soft-tissue stabilizer, providing 53% of the total restraining force.10–12 Surgical treatment of patellofemoral instability in skeletally immature patients is evolving from non-anatomic extensor mechanism procedures to anatomic restorative procedures based on MPFL reconstruction. Nonetheless, the treatment remains controversial and long-term results are unclear, particularly in patients with associated factors such as trochlear dysplasia or patella alta when MPFL reconstruction is the sole method used to treat patellofemoral instability. Our aim was to evaluate: (1) the long-term results of MPFL reconstruction as the sole method of patellofemoral instability treatment in skeletally immature patients and (2) their relationship with the presence of other potentially associated factors.
Patients and methodsInclusion/exclusion criteriaOur inclusion criteria were (1) patients without physeal closure (according to their X-rays which were evaluated by a senior orthopaedic surgeon and a senior radiologist), (2) patients undergoing MPFL reconstruction for treatment of symptomatic patellofemoral instability refractory to conservative treatment, (3) patients who underwent surgery with the same technique and (4) patients admitted to the same institution between 2002 and 2009 for surgery. Patients with other pathological associated conditions of the knee were excluded.
Study typeWe conducted a prospective study. Patients were evaluated in the medium- (mean 44 months) and long-term (mean 116.4 months) post-operative period. The following pre-operative data were collected for each patient: (1) age, (2) gender, (3) patellar tilt, (4) patella height, (5) TT-TG and (6) trochlear dysplasia. Existing risk factors for patellofemoral instability were depicted using conventional radiographs and computed tomography. Patella height was determined using X-rays with the Caton-Deschamps index. Although the Caton-Deschamps index was first described in adults, studies evaluating the validity of the index to investigate patellar height showed that it is a simple and reliable index for evaluating patellar height in children as well.13 According to Théveni-Lemoine et al., the mean±standard deviation patellar length was 33.39±7.4mm, the mean patellar tendon length was 34.57±6.7mm and the mean Caton-Deschamps index was 1.06±0.21. The latter was considered in this study as the standard value. Patellar tilt and TT-TG distance were evaluated using the computed tomography. TT-TG values greater than 20mm were considered abnormal. Trochlear dysplasia was evaluated according to Dejour et al. The patients were systematically examined arthroscopically and subsequently treated with MPFL reconstruction using a gracilis tendon autograft. The clinical results were calculated using an objective knee score according to Kujala. Additionally, the patient's levels of physical activity were determined as per Tegner. The results were compared pre- and post-operatively (at the medium- and long-term follow-up).
Surgical techniqueAll selected patients underwent MPFL reconstruction (Figs. 2–4) as described by Chassaing.14 This is a technique for patellar stabilization by reconstruction of the medial patellofemoral ligament with the gracilis tendon. The tendon is anchored posteriorly on the soft tissue of the medial femoral epicondyle and anteriorly on the medial border of the patella. The plasty is completed by suture of the medial patellar wing.
Statistical analysis was performed using SPSS® statistics software 20. The data are depicted as mean±standard deviation for each variable. Student's t-test was used to compare the pre-operative and post-operative results. A significance level of p<0.05 was considered.
ReabilitationAfter repair of the ligament, the patient's knee was kept in removable immobilizers for three weeks. Early rehabilitation protocols were used in all cases.
Postoperative instability recurrenceThe patients were divided into three groups according to patellofemoral instability recurrence after surgery:
- (1)
Dislocation, which indicated that the patient had a total loss of congruence between the patella and trochlea;
- (2)
Unstable, which indicated that the patient's knee presented with a positive apprehension test or showed signs of subluxation but without a dislocation recurrence;
- (3)
Stable, which indicated that the patient's knee did not show a positive Smillie test or showed signs of episodes of subluxation.
All patients and legal guardians gave their informed written consent for follow-up evaluation and data publication.
ResultsPopulation characterizationThirty-five patients met the inclusion criteria. There were 24 women and 11 men with a mean age of 15.9 years (ranging from 14 to 17) at the time of surgery. On physical examination, all patients presented with a clinical patellar tilt. High patella was found in 10% of patients. The TT-TG was within a normal range (12±5mm) for all patients. Trochlear dysplasia was observed in 80% of patients: 40% had Dejour's type A; 34% type B; 20% type C and 6% type D.
Functional evaluationAfter the application of the Kujala questionnaire, we found a pre-operative mean score of 54±11 points. The medium-term Kujala score (84±9) significantly improved (p<0.0001) compared to the pre-operative score (preliminary results presented by Simões and Oliveira at the 11th European Federation of National Associations of Orthopaedics and Traumatology congress). However, there was a decline in the long-term (78±3) score from the medium-term score. The Tegner activity score showed a significant decrease (p<0.0001) from the pre-operative period (level 7±2) to the medium- (level 6±2) and the long-term (level 4±3) follow-up (Figs. 5 and 6). The long-term results were significantly (p<0.0001) lower in the presence of trochlear dysplasia type B to D. No correlation with the presence of high patella was observed. The presence of intra-operative chondral lesions correlated with lower scores, though this was not statistically significant.
ComplicationsThere were three minor complications: two hematomas and one superficial infection that resolved without complications. Five patients maintained residual anterior knee pain as result of patellar chondropathy that was diagnosed intra-operatively. Three patients complained of graft donor site pain, while one patient presented with a patellar dislocation three years after surgery and three patients presented a positive apprehension test or showed signs of subluxation but without a redislocation. Knee stiffness was not observed in any patient.
DiscussionThere are many studies analysing the results of MPFL reconstruction in recurrent patellar instability. However, most are small case series, with less than 30 patients. With the exception of studies that include a long follow-up period, such as those of Li et al.15 and Zaffagnini et al.,16 both with a six year follow-up, all of the remaining studies have short follow-ups. The majority of the studies employ adjunctive techniques other than MPFL reconstruction, making it difficult to distinguish the determining factors in their outcomes. Furthermore, many of them include skeletally mature patients. Since patellofemoral instability is a common condition among patients with open physes and many surgical techniques are not appropriate for this patient subgroup, there is a clear demand for large studies analysing the long-term results of MPFL reconstruction as the sole method of patellofemoral instability treatment. We present a series of 35 cases evaluated in the medium- (mean 44 months) and long-term (mean 116.4 months) post-operative period. Our study includes 22 women and 11 men with a mean age of 15.9 years at the time of surgery. Epidemiologically, these data are in agreement with the literature, which suggest that recurrent instability is particularly high in females from 10 to 17 years of age.16 According to systematic reviews on the reconstruction of the MPFL, despite the identification of several methodological weaknesses, the existing studies document good results after MPFL reconstruction alone, even in the presence of other contributing factors for the disease.17–19 Our work confirms the good results in the medium-term but shows possible long-term deterioration. Compared to the pre-operative Kujala score (54±11 points), the scores remained significantly favourable in both the medium- (84±9) and long-term (78±3), though a decline over time was observed. The Tegner activity score showed a significant decrease (p<0.0001) over the entire follow-up period. We found that these long-term results were significantly (p<0.0001) lower in patients with trochlear dysplasia type B to D. No correlation with the presence of high patella was found. The presence of intraoperative chondral lesions correlated with lower scores, though not statistically significant. Trochlear dysplasia is characterized by abnormal trochlear morphology and a shallow groove. It is associated with recurrent patellar dislocation, but it is unclear whether dysplasia is congenital, the result of lateral tracking and chronic instability, or caused by a combination of factors. Trochlear dysplasia is estimated to occur in less than 2% of the population; however, it is present in up to 85% of patients with recurrent patellar instability. Dejour and Le Coultre reported that 96% of patients with a history of patellofemoral dislocation had radiographic evidence of trochlear dysplasia.20 In our study, trochlear dysplasia was found in 80% of patients. The presence of the long term deterioration especially with trochlear dysplasia in our patients may be explained by the occurrence of patellofemoral chondral lesions by repetitive trauma of a more fixed patella on a flat or convex trochlea. The long-term deterioration may also be explained by the fact that we are comparing results from patients with 10 years of difference, between young people in pubertal age with high physical activity and adults who do not have the same number of hours available for physical activity. According to the literature, the most reported complications after MPFL reconstruction include patellofemoral arthrosis, graft impingement, graft failure, quadriceps dysfunction and decreased knee range of motion. We recorded five cases of residual anterior knee pain as result of patellar chondropathy that was diagnosed intra-operatively, one case of patellar dislocation (three years after surgery) and three cases presenting a positive apprehension test or showing signs of subluxation but without a redislocation. This represents a redislocation rate of 2.85% and a residual instability rate of 11%. Quadriceps dysfunction or knee stiffness was not observed in any patient. A decade after isolated MPFL reconstruction, results remain satisfactory. The technique presented in this study allowed for good clinical results, with few complications, using a small incision to reconstruct in an isometric fashion this important patellar stabilizer, the MPFL. However, our study draws attention to a possible functional deterioration over time, especially in the presence of trochlear dysplasia, types B to D. This subgroup, especially individuals with high physical demands, may benefit from associate trochleoplasty in a second intervention. In this context, we must remember that patellofemoral instability is a multifactorial entity and when a factor is corrected, we must not ignore the problem as a whole.
ObservationsPart of the results of this paper were orally presented and discussed during the 16th Congress of the European Federation of National Associations of Orthopaedics and Traumatology (EFORT), held in Prague (Czech Republic) between the 27th and the 29th of May 2015.
Conflicts of interestThe authors declare no conflicts of interest.
Head of the Orthopedic Department at Centro Hospitalar de São João and Hospital CUF Porto.
Coordinator of the Knee and Arthroscopic Unit at Orthopedic Department/Centro Hospitalar de São João and Hospital CUF Porto; member of the Sports Medical Center at Hospital CUF Porto.