Measure clinical competence for female climacteric diagnosis and treatment in physicians from a Mexican social security system.
MethodsCross-sectional and multi-centric study in 78 physicians from five primary health care units from the Mexican Institute of Social Security in Guadalajara City, Jalisco, Mexico. We measured clinical competence with an instrument specially designed and validated (reliability p=0.92 accord to Kuder–Richardson test). We obtained descriptive statistics and compared proficiency level accord to labor, demographic and academic characteristics using no-parametric statistic.
ResultsClinical competencies medians in five primary health care units were 8–21 points in a scale with maximum value of 108. We do not found significant differences to compare medical unit, gender, specialty, previous training in female climacteric symptoms, contract type, workshift and medical certifications (p>0.05).
ConclusionsClimacteric clinical competence is null or very low in primary health care physicians from Guadalajara City. Educational interventions are required.
Medir competência clínica para o diagnóstico e tratamento do climatério feminino nos médicos a partir de um sistema de segurança social mexicano.
MétodosEstudo transversal e multicêntrico com 78 médicos de cinco unidades básicas de saúde do Instituto Mexicano de Segurança Social na Cidade de Guadalajara, Jalisco, México. Medimos competência clínica com um instrumento especialmente concebido e validado (confiabilidade p=0,92 de acordo com o teste de Kuder-Richardson). Obtivemos estatística descritiva e comparação do nível de proficiência no trabalho de acordo com as características demográficas e acadêmicas com o uso do método não paramétrico.
ResultadosCompetências clínicas medianas em cinco unidades básicas de saúde foram de 8 a 21 pontos em uma escala com valor máximo de 108. Não se encontraram diferenças significativas para comparar unidade médica, sexo, especialidade, treinamento prévio em sintomas do climatério feminino, tipo de contrato, turno de trabalho e certificações médicas (p>0,05).
ConclusõesCompetência clínica para o diagnóstico e tratamento do climatério é nula ou muito baixa em cuidados médicos primários de saúde na Cidade de Guadalajara. Intervenções educativas são necessárias.
An important number of mean age women have vasomotor symptoms as hot flashes and night sweats, and other alterations usually associated with diminished levels of endogenous estrogen. These conditions can diminish quality life in this specific group of women,1 by other way population aging with a large number of climacteric patients has great challenges in the identification of risk factors, population educational programs about natural consequences of aging and the preservation of health and quality life in mean age women. These factors are transcendent in developing countries.
In Guadalajara, Jalisco, Mexico, exist 307,225 women among 35–55 years-old.2 In this group, its estimated that 55% have climacteric symptoms,3 would amount to 168.974 women these characteristics. In this context, primary healthcare’ physicians have an opportunity to reduce risk for diverse group of cardiovascular, metabolic and oncologic diseases associated with female climacteric and to improve quality life of affected.4,5
Some studies explored knowledge, abilities, practices and self-perceived deficiencies of physicians for diagnosis and treatment of female climacteric and has displayed that clinical competence level is poor.3,6,7 This contrasted with high competencies perceived on physicians for women with these symptoms.8 The magnitude of this serious problem in Guadalajara City is unknown and in Mexico has been poorly explored.
A poor physician's clinical competencies for diagnosis and treatment of any disease is associated with high health cost and preventive deficiencies for risk factors non-identification, sub-diagnosis and bad treatment.9 Understanding this as the capacity of identify and treat variable complexity clinical problems and decide the best choice.10–12
In this context, this research aimed measure clinical competence for female climacteric diagnosis and treatment in physicians from a Mexican social security system.
MethodsCross-sectional and multi-centric study achieved in 78 physicians from five primary health care units from Mexican Institute of Social Security in Guadalajara City, Jalisco, Mexico. We studied a purposing sample composed by all physicians of any age and gender that we found working during study period and agreed participate in research.
We measured clinical competence of physicians for diagnosis and treatment of female climacteric and to compared by medical unit, type of contract, workshift, gender, specialty, previous training in female climacteric and medical certifications.
Labor, demographic and academic variables were collected by mean of a questionnaire, and clinical competence of physicians for diagnosis and treatment of female climacteric symptoms was measured using an instrument specially designed with this purpose.
Instrument for measurement of clinical competence of physicians for diagnosis and treatment of female climacteric evaluate five indicators or domain zones “risk factors”, “clinical data”, “diagnostic tools”, “diagnosis” and “therapeutic” and offered a global punctuation of clinical competence. A number of 108 multiple choice questions form this instrument with three answer options “true”, “false” and “I don’t know”, a correct answer of any question is equal to +1 and incorrect answer is equal to −1 while “I don’t know” answer is equal to 0. With this evaluation system the score of instrument is among −108 and 108 points classified in following clinical competence strata: “Null” <15 points, “Very low” 16–30 points, “Low” 31–45 points, “Middle” 46–60 points, “High” 61–75 points and “Very high” >76 points. This instrument obtained a global reliability coefficient of 0.92 accord to Kuder–Richardson test, and for each indicator was 0.76, 0.76, 0.86, 0.91 and 0.95 respectively with same test.
We obtained descriptive statistics and we compared level clinical competence accord to variables previously enunciated by mean U of Mann–Whitney or Kruskal–Wallis test (p≤0.05). This analysis was made using Epi Info© version 3.3.2 for Windows©.
This research was considered of “without risk” for participants accord to national legislation on health research,13 and don’t was necessary obtained informed consent.
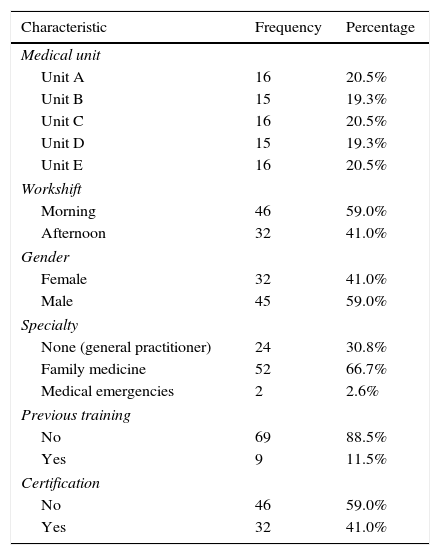
Results78 physicians were included and your demographic, labor and academic characteristics are showed in Table 1. Equally distributed between medical units was observed and most were of definitive contract, morning workshift, males, specialists in family medicine and without previous training in female climacteric neither certification.
Labor, demographic and academic characteristics of physicians.
| Characteristic | Frequency | Percentage |
|---|---|---|
| Medical unit | ||
| Unit A | 16 | 20.5% |
| Unit B | 15 | 19.3% |
| Unit C | 16 | 20.5% |
| Unit D | 15 | 19.3% |
| Unit E | 16 | 20.5% |
| Workshift | ||
| Morning | 46 | 59.0% |
| Afternoon | 32 | 41.0% |
| Gender | ||
| Female | 32 | 41.0% |
| Male | 45 | 59.0% |
| Specialty | ||
| None (general practitioner) | 24 | 30.8% |
| Family medicine | 52 | 66.7% |
| Medical emergencies | 2 | 2.6% |
| Previous training | ||
| No | 69 | 88.5% |
| Yes | 9 | 11.5% |
| Certification | ||
| No | 46 | 59.0% |
| Yes | 32 | 41.0% |
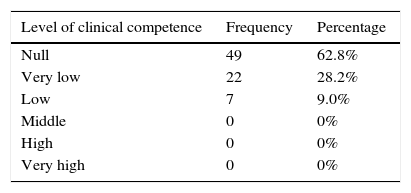
In Table 2 showed the clinical competence level observed in physicians. We observed that no were physicians with “Middle”, “High” or “Very high” level of competence.
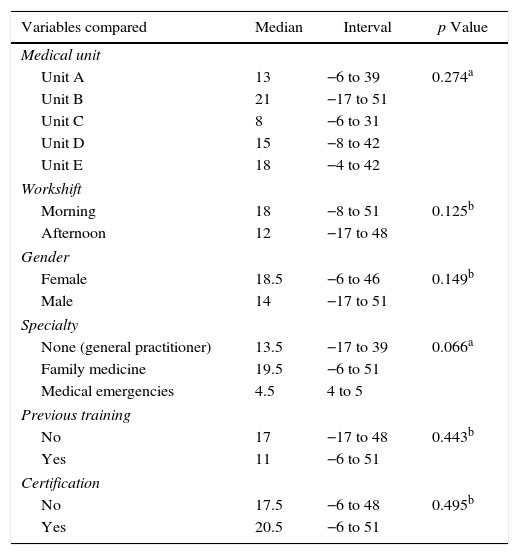
Comparing clinical competence for diagnosis and treatment of female climacteric do not found significant differences accord to medical unit, gender, specialty, previous training in female climacteric, type of contract, workshift and medical certifications (p>0.05). In Table 3 showed results of U of Mann–Whitney and Kruskal–Wallis test.
Comparison of clinical competence of physician's accord to variables included.
| Variables compared | Median | Interval | p Value |
|---|---|---|---|
| Medical unit | |||
| Unit A | 13 | −6 to 39 | 0.274a |
| Unit B | 21 | −17 to 51 | |
| Unit C | 8 | −6 to 31 | |
| Unit D | 15 | −8 to 42 | |
| Unit E | 18 | −4 to 42 | |
| Workshift | |||
| Morning | 18 | −8 to 51 | 0.125b |
| Afternoon | 12 | −17 to 48 | |
| Gender | |||
| Female | 18.5 | −6 to 46 | 0.149b |
| Male | 14 | −17 to 51 | |
| Specialty | |||
| None (general practitioner) | 13.5 | −17 to 39 | 0.066a |
| Family medicine | 19.5 | −6 to 51 | |
| Medical emergencies | 4.5 | 4 to 5 | |
| Previous training | |||
| No | 17 | −17 to 48 | 0.443b |
| Yes | 11 | −6 to 51 | |
| Certification | |||
| No | 17.5 | −6 to 48 | 0.495b |
| Yes | 20.5 | −6 to 51 | |
This is the first study of clinical competence of primary health physicians for diagnosis and treatment of climacteric symptoms in Guadalajara City, the second city most important from Mexico accord to your population dimensions after of Mexico City.14 Results showed, demonstrated that clinical competencies of primary health physicians for diagnosis and treatment of climacteric is poor. This agrees with reported by other authors whose has demonstrated this problem in other regions of Mexico,3,6,7 and we agree on the need of educational interventions for to improve these competencies.
However, these results go beyond this simple demonstration, whereas that we do not found significant differences to compare these competencies accord to variables as specialty and professional certification that suggest a poor quality of medical formation and continuous medical education. Also, is probable that exist a disproportionate cost in health care for this syndrome and, more serious and probable even that exist inadequate prescriptions of hormonal supplements with multiple secondary and adverse effects when are bad prescribing, as risk increasing of breast cancer,15 that should be measure.
Furthermore, considering that exist a guideline for diagnosis and treatment of peri- and post-menopause development in studied physicians’ adscription institution,16 our results suggest a poor disposition of these for self-training because this is open access.
We concluded that is necessary to explore prescription quality of hormonal supplements and to search intentionally adverse effects in women with risk age for menopause that received health care in the medical institution. In addition, to intervene for improve physician's clinical competencies for this syndrome and to explore for other diseases.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like thank to physicians’ participants and medical institution authorities for facilities granted, and to anonymous peer reviewers assigned to this manuscript for your contribution to improving.