Introduction
Atopy is the genetic propensity to develop IgE antibodies in response to allergens exposure.1 There are some reports, which associate urinary system diseases with allergic sensitization, however, a cause-effect relationship has not been demonstrated.2 Oehling proposed that if the urinary system removes waste products, toxins and excess water from the body, through a filtration, collection and excretion system, then a sensitization in situ to macromolecules contained in the glomerular filtrate, could occur in patients with atopy.3 Thus, inflammation at any level of the urinary tract could have an immunologic origin in response to allergenic proteins, causing type I, II, III or IV hypersensitivity, or a combination of some of them; so that, cellular and/or humoral response would trigger immediate or late reactions leading to an acute event, or a sustained proinflammatory response.3,4 In support of this theory, it has been demonstrated an allergic inflammatory response in the urinary bladder and the ureters through passive sensitization with allergenic proteins, inducing histamine release in situ and smooth muscle contraction.5
Among the urinary system diseases, with high prevalence of allergic sensitization, are: nephrotic syndrome,6 cystitis,7 enuresis and urinary tract infection,8 Henoch-Schönlein purpura and IgA nephropathy.9 In tubulopathies -such as renal tubular acidosis- the prevalence of allergic sensitization has not been determined, which motivated this study. The RTA is a syndrome, characterized by hyperchloremic metabolic acidosis due to a tubular dysfunction of the regulatory mechanisms of acid-base balance. It is an underdiagnosed illness. At the Instituto Nacional de Pediatría, there are about 35 cases per 10,000 medical files.10 In Holland, it is calculated a probability of 0.6 cases per 100,000 newborns.11 There are many causes for RTA, but in children most of the cases are idiopathic.10
Methods
Children with an established diagnosis of primary RTA were recruited during a four-month period from the outpatient clinic of the department of Nephrology, at a third level pediatric hospital. Upon approval by the Ethics Committee and with informed parental consent, a questionnaire was applied to investigate family history of atopy, age of onset of RTA and symptoms at the time of diagnosis. Skin prick tests were conducted with allergenic extracts (Allerquim® 1:20 w/v), with the most common allergens present in the environment (house-dust mites, cat and dog dander, pollens, molds, whole milk, yolk, white, wheat, corn, and soy). Skin tests were read after 20 minutes, and the results were considered positive if a wheal was at least 2 mm larger than the control one (histamine 1mg/ml). Total IgE, specific IgE and milk precipitins were performed. All children regularly consumed whole milk. Blood was drawn after 6 to 8 hours fasting.
Total IgE antibodies were determined using the Enzygnost-IgE micro test. The detected value was shown as International Units per mililiter (IU/ mL). The reference values were: 0 to 2 years old children: 30 IU/mL, 2 to 5 years old children: 60 IU/mL, 6 to 9 years old: 90 IU/mL. Any greater value was considered as increased.
Specific IgE for milk antigens, egg white, yolk, wheat, oats, soy, and rice, was determined by the Pharmacia CAP system. The lower limit of allergen-specific IgE detection was 0.35 kU/L. Food sensitization was defined according to the NHANES (National Health and Nutritional Examination Survey) criteria, as positive if the allergen-specific IgE was ≥0.35 kU/L for any of the tested foods.12 Milk precipitins were determined by the modified Ouchterlony technique,13 using centrifuged cow's whole milk as an antigen. On an agar slab with one mm thickness, the antigen and the serum were applied to the wells. After two days of incubation, the slabs were washed and the precipitation lines were dyed with thiazide red to be read off. Each sample was made on duplicate and compared with controls. Antigen-antibody complex precipitation was measured by comparing the number and density of the precipitation lines. The results were reported as positive or negative by an expert in the field.
The operational definitions in the present study were: Non-specific rhinitis, if the patient had obstruction and hyaline rhinorrhea without pruritus. If the children had obstruction and hyaline rhinorrhea, along with pruritus, sneezing, and positive cutaneous tests, then the diagnosis of allergic rhinitis was made.14 The diagnosis of asthma was established with cough, wheezing, respiratory distress, positive skin prick tests and pulmonary function tests.15 The diagnosis of atopic dermatitis was made based on major criteria: pruritus, eczema (facial and extensor involvement), chronic or relapsing dermatitis and/or personal or family history of atopy;16 and the diagnosis of allergic conjunctivitis was made if there was pruritus and red eye, along with positive skin prick tests.17 Quantitative variables were analyzed in terms of mean and standard deviation. Qualitative variables were analyzed in terms of the frequency and percentages. The correlation coefficients were reviewed with the Kendall, Pearson, and Spearman tests, with SPSS 10.
Results
Forty-three children with the diagnosis of RTA, aged 5 months to 9 years old (mean, 3.4 ± 1.8 years), and a male/female ratio of 1.7:1, were included. Twenty-eight of them had distal RTA (65.2%) and 15 proximal RTA (34.8%).
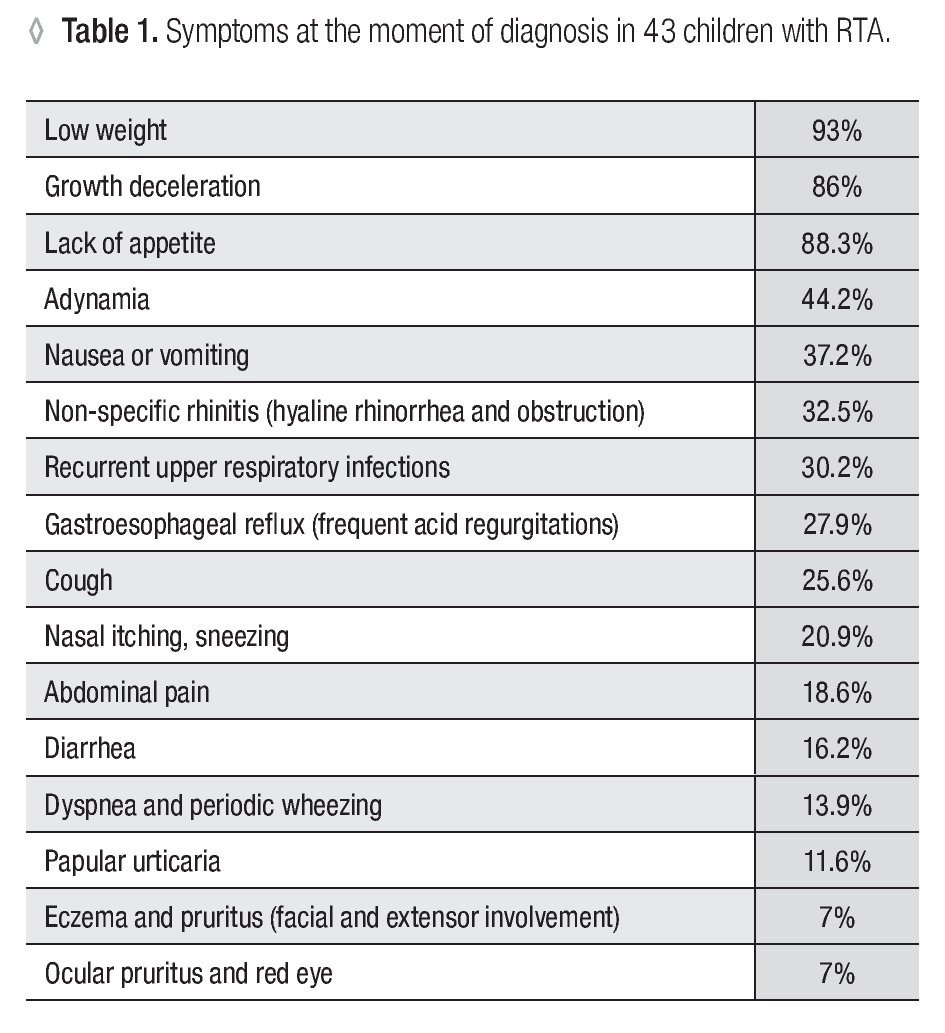
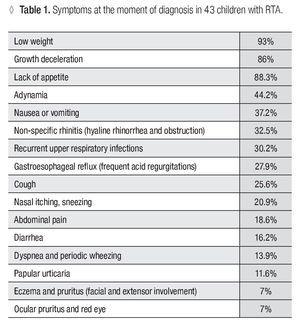
Family history of atopy in first degree was positive in 13.9%. The age of onset of disease ranged between 2 and 18 months (mean 8.6 ± 4.8 months). The frequency of symptoms as a reason for consultation is mentioned in Table 1.
Nearly a half of parents (48.8%) associated the introduction of whole milk in the child's diet, with the beginning of the symptoms; and close to a quarter (23.3%) noticed that withdrawal of some foods -suspected of being implicated in triggering ATR-, rendered improvement of symptoms (mainly in lack of appetite, nausea, vomiting, diarrhea, and growth deceleration), which allowed to reduce the dose of the alkalinizing therapy (citrate and/or sodium bicarbonate).
Blood eosinophils were > 450 cells/μL in 30.2% of the included children. In 12 cases (27.9%), skin prick tests were positive, mainly to mites in 16.3%, whole milk in 14%, egg white in 11.6%; wheat, cynodon, oak and cat in 9.3%; soy and molds in 7%, and casein in 5%. With these results the diagnosis of allergic rhinitis was established in 20.9% of the children, asthma in 11.6%, atopic dermatitis in 7%, and allergic conjunctivitis in 7%. Total IgE was increased in 34.9% ranging between 5.9 and 324 IU/mL (mean 118 ± 30.6 UI/ mL). Specific IgE was positive to sensitization in 11 children (25.6%), being to whole milk in 6, lactoglobulin in 6, wheat in 6, egg white in 4, soy in 4, lactalbumin in 3, oats in 3, rice in 3, and casein in 2. The cow's milk precipitins test was reported positive in 9 patients (21%). Increased total IgE level showed a significant correlation with positive skin prick tests (p <0.01). There was no correlation between the sensitization to whole milk, lactoglobulin, lactalbumin, or casein, and the positivity for milk precipitins.
Discussion
RTA is a low prevalence disease.10,11 In this study, primary RTA was demonstrated through serum electrolytes, gasometry and urinary studies. The proportion of RTA subtypes (distal/proximal), was similar to previous descriptions.18
Family history of atopy is the most important risk factor for the development of sensitization in children.19 Among children with RTA, the frequency of family history of atopy in siblings was low (13.9%), compared with a genetic risk study in an open population, where atopy in siblings was found in 40% of their sample.20 The frequency of symptoms enlisted in Table 1 matches with those typically described for this illness.21 The most common reasons for consultation were failure to thrive and lack of appetite. We found a high prevalence of non-specific rhinitis (32.5%), -rhinitis without pruritus, sneezing and a negative skin prick test- compared with that found in the American population, which is about 5.4%.14,22 Children with recurrent upper airway infections (RUAI) -more than 6 episodes per year- have a high risk for atopy.23 We found a high prevalence of RUAI (30.2%) in children with RTA, compared with a cohort of 693 individuals, in whom the prevalence was 23%.24 Regarding papular urticaria we found a high prevalence as well (11.6%), compared with an open study in children in a tropical climate (8.5%).25
Based on the finding of parents who associated the onset of symptoms with milk ingestion (48.8%), we suspected food intolerance or food allergy. At that moment, lactose intolerance had not been investigated in RTA. The search in Pub-Med for "lactase deficiency" or "disaccharidase deficiency" in primary RTA, was unsuccessful.26 Because a retrospective questionnaire was applied in this study, it was not possible to know if milk ingestion caused symptoms and signs which could suggest lactase deficiency, like explosive acid depositions or reducting sugars in the feces.
While alkalinizing therapy favors the increase in height and weight in RTA,27 currently there are no published reports, which associate food suppression diets with clinical improvement of RTA. Nearly a quarter of parents (23.3%) noticed a clinical improvement, as a result of withdrawal of some foods, which allowed dose reduction of alkalinizing therapy.
Eosinophilia -blood eosinophils > 450 cels/ μL- found in 30.2% of children, is frequently associated with allergic disorders, however, the mechanism of eosinophilia is neither IgE-mediated nor as yet clearly defined.28 A diversity of diseases can increase eosinophil count. One recent study of kidney disease patients, showed that there was no a correlation between eosinophilia and allergy.29
Sensitization to food or airborne allergens is a risk factor for the development of allergic diseases.19 We found a high prevalence of positive skin prick test (27.9%) among children with RTA, compared with 19.6% of skin reactivity in an open population study of 1,456 children.30 The sensitization rates found in children with RTA (mite: 16.3%; whole milk: 14%; egg white: 11.6%; wheat, cynodon, oak and cat: 9.3%; molds and soy: 7%; and casein: 5%) were higher than those described in the formerly mentioned study (mite: 11.9%, pollen: 7.8%, cat: 5.8%, and food: 3.5%), which demonstrated that testing of only four allergens (mite, pollen mix, cat and food) is enough to establish the diagnosis of allergy in 94% of atopic children.30 The sensitization found in RTA, along with some direct questions from the initial questionnaire helped us to integrate the diagnosis of allergic diseases. We found a high prevalence of allergic rhinitis (20.9%), asthma (11.6%), and atopic dermatitis (7%), compared with previous publications using the ISAAC methodology in Mexican children, in which the reported prevalence of asthma, rhinitis and eczema, were: 5.8%, 4.9% and 4.1%, respectively.31 In allergic conjunctivitis we found a lower prevalence than the previously described in Mexico (7% vs 15%).32
Total IgE was high in 34.9% of the included. Even though the increase in the total IgE value is considered useful as a screening test for the diagnosis of allergic diseases, numerous pathologic conditions could increase its levels.33 Food specific IgE was positive for sensitization in 25.6% of children for: whole milk: 14%, lactoglobulin: 14%, wheat: 14%, egg white: 9.3%, soy: 9.3%, lactalbumin: 7%, oats: 7%, rice: 7%, and casein: 4.7%. The reliability of specific IgE for diagnosis of food allergy is poor, due to its low correlation with positive skin prick tests and clinical symptoms,34 but we only search for sensitization.
Low titers of milk precipitins may be present in the serum of about 2% of normal individuals who ingest milk.35 Immaturity of gastrointestinal barrier in infants allows the passage of macromolecules (food allergens), like cow's milk, into the bloodstream,36 favoring the production of precipitating antibodies, which generally disappear with age. This antibodies persist with high titers in: chronic diarrhea, coeliac disease, Down syndrome, cystic fibrosis, IgA deficiency, Wisckott-Aldrich syndrome, familial dysautonomia, and Hurler syndrome.37 Some individuals with a genetic predisposition to atopy have a dysfunction in the intestinal barrier and immunologic tolerance, which allows sensitization to food proteins, with the consequent development of allergic inflammatory response.38 In the present study we found a high prevalence (30.2%) of cow's milk precipitins, however, we cannot assure that this fact holds a clinical significance, due to the low sensitivity and specificity of the procedure.35
Conclusions
Even though the patients with RTA displayed a high prevalence of sensitization to inhaled and food allergens, and positivity to milk precipitins, it is necessary to investigate the prevalence of sensitization to allergens in children with RTA in cohorts with larger sample size, and using diagnostic tests with greater sensitivity and specificity to determine the presence of type I, II, III and/or IV hypersensitivity.
Acknowledgment
We thank Gladys Faba Bealmount for her assistance.
Correspondence author: Blanca María Morfín Maciel.
COMPEDIA. Colegio Mexicano de Pediatras especialistas en Inmunología Clínica y Alergia. Fax: 525 55527
12740, Ignacio Esteva 107-206, Col. San Miguel Chapultepec, 11850. México, D.F.
E mail:blancamorfin@hotmail.com