This is the first report of a cutaneous infection in an immunocompromised domestic cat caused by Setosphaeria turcica. The investigation encompasses an assessment of its virulence factors and susceptibility to antifungal drugs. The isolated strain originated from a domestic cat displaying cutaneous lesions that tested positive for feline leukemia virus (FeLV) infection. Identification procedures employed both microscopic and molecular techniques, with molecular identification relying on ITS DNA sequencing. Enzymatic assays targeting lipase, phospholipase, protease, and keratinase yielded negative results, suggesting the prevalence of alternative virulence mechanisms. Successful treatment of the infection was achieved with itraconazole, and susceptibility testing confirmed its sensitivity to azoles and polyene antifungal drugs.
Este es el primer informe de infección cutánea en un gato doméstico inmunocomprometido causada por Setosphaeria turcica. La investigación abarca una evaluación de los factores de virulencia de este hongo y de su sensibilidad a los fármacos antifúngicos. El hongo se recuperó de un gato doméstico positivo al virus de la leucemia felina (FeLV). Los procedimientos de identificación emplearon técnicas microscópicas y moleculares, con identificación molecular basada en la secuenciación de ADN ITS. Los ensayos enzimáticos dirigidos a lipasa, fosfolipasa, proteasa y queratinasa arrojaron resultados negativos, lo que sugiere la prevalencia de mecanismos de virulencia alternativos. El tratamiento exitoso de la infección se logró con itraconazol; la sensibilidad a los fármacos antifúngicos azoles y poliénicos pudo ser confirmada en el laboratorio.
Feline leukemia virus (FeLV) is globally prevalent, and infection occurrences are linked to risk factors and control measures, representing a primary cause of mortality among feline infectious diseases1. FeLV transmission typically transpires through oronasal routes during prolonged and close contact between an infected cat and a healthy counterpart, primarily through saliva rich in viral particles11.
Animals affected by FeLV often exhibit compromised immune systems, rendering them more susceptible to infectious diseases and specific types of cancer. The compromised state of the immune system in these animals increases the likelihood of developing lesions and infections upon contact with potentially harmful agents, including fungi and non-pathogenic bacteria7.
Setosphaeria turcica (Luttrell) Leonard and Suggs (syn. Helminthosporium turcicum, teleomorph Exserohilum turcicum (Pass.) Leonard and Suggs), belonging to the order Pleosporales, is a heterothallic ascomycete recognized as the northern corn leaf spot fungus. This plant pathogen primarily affects corn (Zea mays), causing a foliar disease known as northern corn leaf blight, with dormant mycelia and chlamydospores found in host plant debris or soil10.
In planta infections are favored by temperatures ranging from 15 to 25°C, dew periods lasting at least 4h, and relative humidity between 90 and 100%14. Following spore germination, the appressorium penetrates the leaf cuticle and epidermis directly. Hyphae then grow intracellularly in the mesophyll, progress to vascular bundles, penetrate the xylem9, and secrete the HT toxin (from H. turcicum).
The HT toxin comprises low molecular weight water-soluble molecules that inhibit chlorophyll biosynthesis, rendering it phytotoxic3. This toxin plays an important role in pathogenicity – the pathogen's ability to infect a resistant host and virulence, reflecting its capability to overcome host-specific resistance mechanisms15.
Despite demonstrating strong pathogenic tendencies and mechanisms in plants, there have been no documented cases of animal diseases caused by this microorganism. This report represents the inaugural documentation of a domestic cat skin infection caused by S. turcica. Furthermore, the study encompasses an evaluation of susceptibility to antifungal drugs and exploration of virulence factors.
The microorganism was initially isolated on potato dextrose agar (PDA) from hair of a domestic cat admitted to Clínica Veterinária Escola do Centro Universitário – UNISEP, Dois Vizinhos, Paraná, Brazil, with four equivalent replicates. The animal was a two-year old female cat, weighing 2.3kg, with free street access, spayed and dewormed, under treatment for FeLV, unvaccinated, with severe non-pruritic hair loss as the main manifested symptom.
On physical examination, icteric oral and ocular mucosa, capillary refill time (CRT) less than 2s, heart rate (HR) 240bpm, respiratory rate (RR) 40mpm, thoracic-abdominal breathing pattern, bilateral symmetrical hair rarefaction, located, scaly, non-erythematous, were observed.
The specific examination with a Wood's lamp was negative. Hair was collected for the culture of dermatophytes and, preventively, baths with shampoo based on 2% ketoconazole and 0.5% chlorhexidine were prescribed.
On day 06, the skin lesions had evolved from localized to generalized and hyperemic. After confirmation of fungal growth on PDA, drug therapy with itraconazole (10mg/kg/d) associated with topical therapy was indicated. After a week of treatment in return, there was an improvement in the patient's clinical condition, absence of desquamation, absence of hyperemia and signs of repilation. At the end of the 28 days of treatment, the patient no longer showed clinical signs of dermatophytosis.
The isolated fungus was studied by light microscopy, associated with microculture and molecular identification. The methodology used was the amplification and sequencing of internal transcribed pacer (ITS) regions, using primers ITS-1 (GAACCWGCGGARGGATCA) and ITS-2 (GCTGCGTTCTTCATCGATGC). The libraries were sequenced using the MiSeq Sequencing System equipment (Illumina Inc., USA) and the V2 Kit, with 300 cycles and single-end sequencing.
The sequences were analyzed using the Sentinel pipeline2. Files were screened for low quality sequences (Phred<20). The software used was built in Python v.3.6, which is inspired by the features of the BioPython project. The taxonomic identification was performed with Blastn v.2.6.0+ (Neoprospecta Microbiome Technology). The hits were evaluated for the highest bit-score and lowest e-value, thus determining the species.
Virulence tests involving evaluation of the production of extracellular enzymes including lipases, phospholipases, proteases and keratinases were performed following methods previously described13, with minimal modifications. In vitro antifungal susceptibility tests were performed following a specific methodology for filamentous fungi (M38-A – CLSI, Reference method for broth dilution antifungal susceptibility testing of filamentous fungi4, with minor adjustments) and the drugs used were ketoconazole, itraconazole and nystatin in concentrations ranging from 0.02 to 100μg/ml.
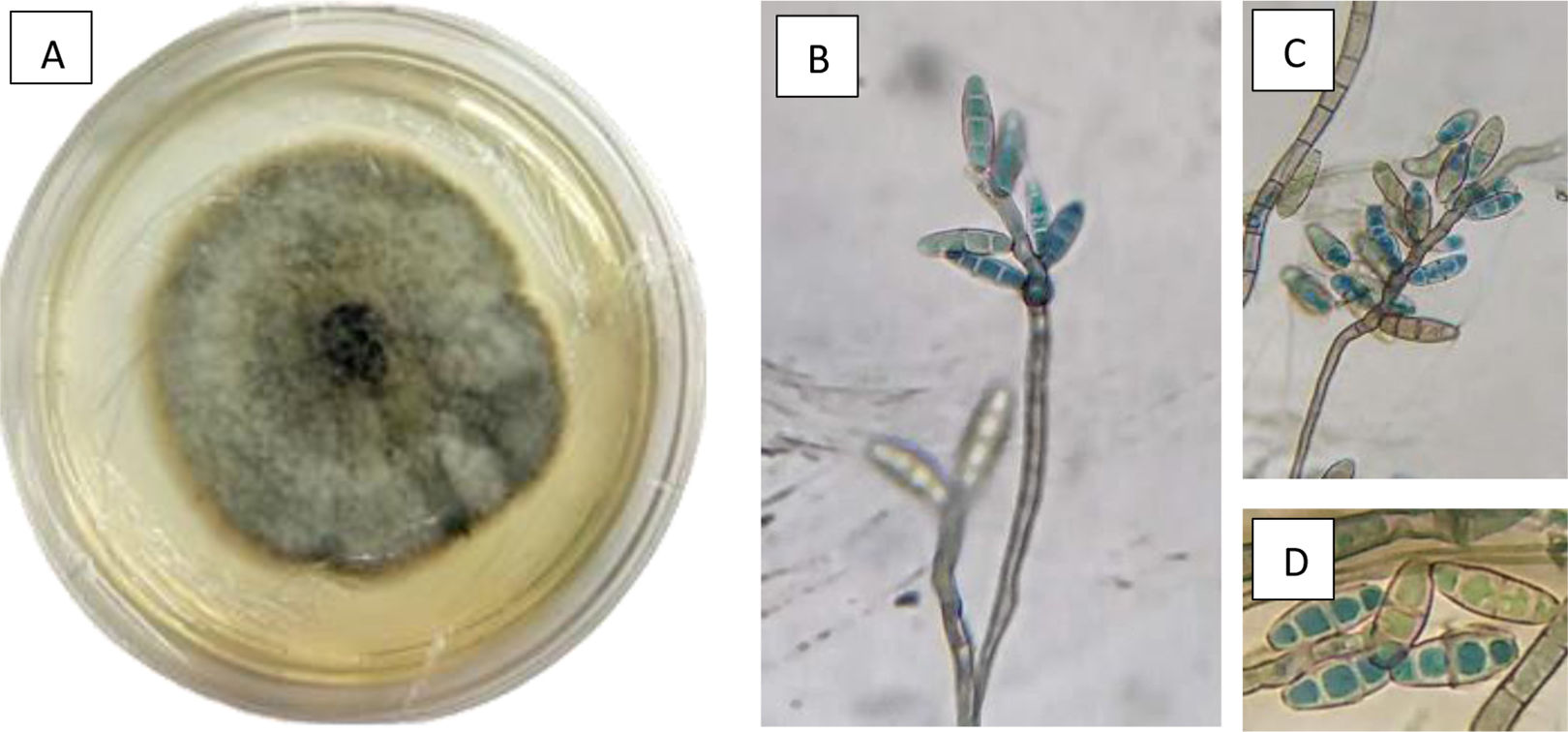
Molecular analysis, associated with the morphological characterization of the isolate, enabled the identification of S. turcica. The evaluation of the colony at a macroscopic level revealed its blackened appearance, circular in shape with irregular edges, with gray aerial hyphae, in PDA medium after sporulation (14 days at 28°C). At a microscopic level, the hyphae, characterized by septa, displayed a brown pigmentation, with flexuous or erect conidiophores characterized by a slender morphology and a nodular apex. These conidiophores serve as the origin for clusters of elongated, oval-shaped macroconidia. The macroconidia, possessing a thin and smooth outer wall, are non-septate and comprise 3–4 cells each, as illustrated in Figure 1.
Macro (A) and micro morphology (B, C and D) of colonies of Setosphaeria turcica showing a blackened colony with gray aerial hyphae with circular shape and irregular edges (A), a solitary and thin conidiophore (B), with a knotty apex (B and C) from which clusters of elongated, oval, thin-walled, smooth, non-septate macroconidia emerge, containing 3–4 cells each (D).
Cats infected with immunosuppressive viruses, such as FeLV, a retrovirus that weakens the immune system, may have an increased susceptibility to fungal diseases6. S. turcica is a fungal pathogen known to cause disease in plants, particularly in maize crops, where it causes the disease known as northern leaf blight8.
Enzymes play a crucial role in the pathogenesis of many fungal pathogens by facilitating their colonization, invasion, and nutrient acquisition within host tissues12. However, S. turcica showed no production of enzymes such as proteases, lipases, phospholipases or keratinases, with implications for its pathogenicity and interaction with the host, probably indicating that the pathogen relies on alternative mechanisms or virulence factors to establish and maintain infection. These mechanisms could include the production of different enzymes, secretion of mycotoxins, modulation of host immune responses, or manipulation of host physiology.
The results for the susceptibility assay showed sensitivity to ketoconazole and itraconazole, with minimum inhibitory concentrations of 25 and 3.37μg/ml, respectively, in addition to nystatin, also of 25μg/ml. Itraconazole is indeed commonly used as a standard antifungal drug for the treatment of various fungal infections. It belongs to the class of drugs known as triazole antifungals and is effective against a wide range of fungal species. It works by inhibiting the synthesis of ergosterol, a key component of fungal cell membranes and was previously reported as the main drug for Microsporum canis dermatophytosis treatment in cats5, thus confirming itraconazole effectiveness against dermatophytes in felines.
This is the first report of a cutaneous infection in an immunocompromised domestic cat caused by S. turcica.