The objective of this study was to estimate the prevalence of Treponema pallidum, Trypanosoma cruzi and Human immunodeficiency virus 1 (HIV-1) in five Amerindian populations of Argentina. A retrospective study was conducted among 857 Amerindian populations (112 Kollas, 298 Mbyá-guaraníes, 79 Sagua Huarpes, 368 Wichis) from 2007 to 2010. Screening and confirmation of T. pallidum, T. cruzi and HIV-1 were performed. T. pallidum and T. cruzi infections were detected in all communities with an overall prevalence rate of 4.2% and 16.8%, respectively. Although HIV was not detected, syphilis and Chagas’ disease represent a challenge for the health care system and the reinforcement of public health strategies is necessary considering the socioeconomic isolation of these populations.
El objetivo de este trabajo fue estimar la prevalencia de Treponema pallidum, Trypanosoma cruzi y virus de la inmunodeficiencia humana (HIV-1) en 5 comunidades originarias de Argentina. Para ello, se realizó un estudio retrospectivo en 857 individuos (112 kollas, 298 mbyá-guaraníes, 79 sagua huarpes, 368 wichis) desde el 2007 hasta el 2010. Se realizó el diagnóstico completo para T. pallidum, T. cruzi y HIV-1. En todas las comunidades se confirmaron infecciones por T. pallidum y T. cruzi con una prevalencia total del 4,2 y del 16,8%, respectivamente. Aunque no se detectó HIV-1, sífilis y Chagas, representan un desafío para el sistema de salud, teniendo que reforzarse las estrategias de salud pública teniendo en cuenta el aislamiento socio-económico que sufren estas poblaciones.
The total population of Argentina in 2010 was 40 117 096 people, of which 955 032 were Amerindians divided into 30 different ethnic groups3. These populations maintain their cultural and social habits; live in poor conditions and although they have access to formal education, half of them have a very limited access to the health system3.
Trypanosoma cruzi is endemic among Amerindians in Argentina, however, few cases of Treponema pallidum and no Human immunodeficiency virus (HIV) cases have been reported in this population4,8.
Syphilis, a sexually transmitted infection (STI) caused by T. pallidum, can be easily controlled due to the availability of a highly sensitive diagnostic test and a very effective and affordable treatment. Nevertheless, in the last ten years it has been raising worldwide9. The statistics show that an estimated 10 million new infections still occur every year9.
Chagas’ disease is caused by the parasite T. cruzi, and is a major cause of morbidity and mortality in Latin America. The infection is transmitted mainly by vectors triatomine bugs; however, it could also be congenital or transmitted by infected blood transfusions. Once Chagas’ disease reaches the chronic phase, anti-parasitic drugs are no longer effective and cardiomyopathy and/or megaesofagus/megacolon may develop. In the Amerindian populations from the Gran Chaco a prevalence of 43.5% for T. cruzi was reported in 20128.
With regard to HIV-1, approximately 110 000 people live with HIV-1 in Argentina, and it has been estimated that 4 of every 1000 individuals are infected with the virus, 30% of whom are unaware of their condition7. T. cruzi and T. pallidum have been detected in Amerindians of Argentina with prevalence rates ranging from 0.3% to 45%, depending on the group and few data are available regarding HIV-15,8.
The objective of this study was to estimate the prevalence of T. cruzi, T. pallidum and HIV-1 in these populations.
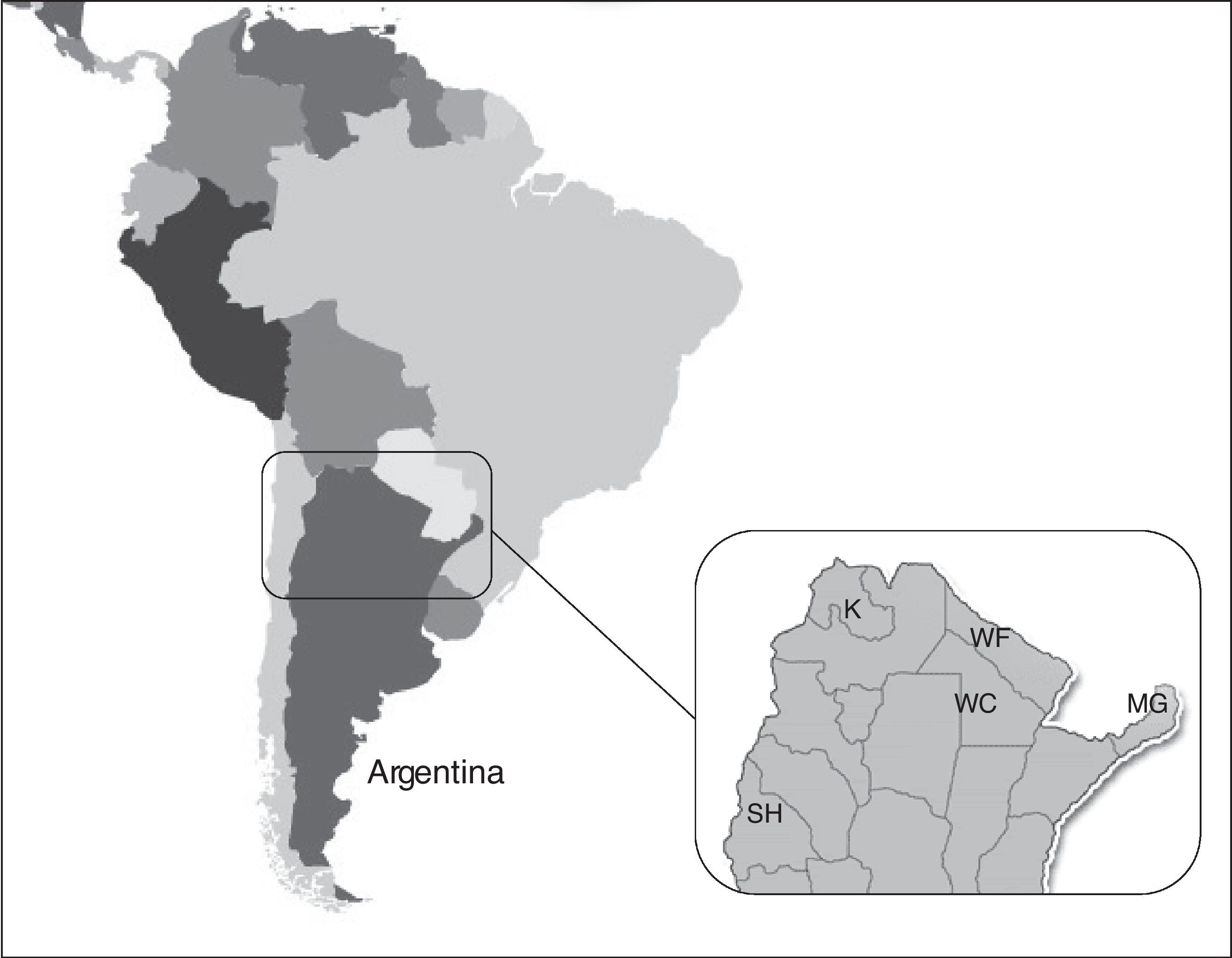
A retrospective study was conducted on samples from 857 aborigines recruited in the period 2007–2010 in four different regions and ethnic groups of Argentina. Out of the total, 298 were Mbyá-guaraní (MG) from Misiones province (Northeast), 112 Kollas (K) from Jujuy province (Northwest), 79 Sagua-Huarpes (SH) from San Juan province (Central West) and 368 Wichis (W) (95 from Formosa (WF) and 273 from Chaco (WC) province) (North) (Fig. 1). All epidemiological data were obtained by reviewing the original standardized questionnaires performed for a previous study. The original protocol was reviewed and approved by the Institutional Review Board as well as by the Scientific Ethical Committee of University of Buenos Aires (INBIRS – OHRP reference numbers: IORG #0004063 and IRB#00004817).
All procedures were performed on the plasma and blood samples preserved at the INBIRS. Screening of T. pallidum was performed by VDRL test (Wiener Laboratories S.A.I.C., Rosario, Argentina) and hemagglutination (TPHA Hemagglutination, Biosystems, Barcelona, Spain). Confirmation was performed by indirect immunofluorescence (IFI, FTA-abs Immunofluorescence, Biocientífica SA, Buenos Aires, Argentina). For HIV-1/2, an ELISA (Dade Behring; Enzygnost anti HIV-1/2 plus) and particle agglutination (SFD HIV ½ PA, Biorad Fujirebio, Japan) were performed. Reactive samples were confirmed by Western blot (New Lab Blot-1, Bio-Rad, Marnes-la-Coquette, France). For T. cruzi an indirect hemagglutination assay (Chagas’, Polychaco S.A.I.C., Buenos Aires, Argentina) and ELISA (Chagatek ELISA, bioMérieux, Buenos Aires, Argentina) were used and confirmed with an “in-house” IFI. The χ2 test and Fisher's exact test were used to compare proportions. All statistical analyses were performed using STATA V.12 (StataCorp. 2011. Stata Statistical Software: Release 12, StataCorp LP, Texas, USA).
Of the 857 individuals, the mean age was 35.8 years old and 477 (55.7%) were females. Only 74 individuals (26 MG, 12 K, 9 SH, 3 WF and 24 WC) reported being transfused with blood components.
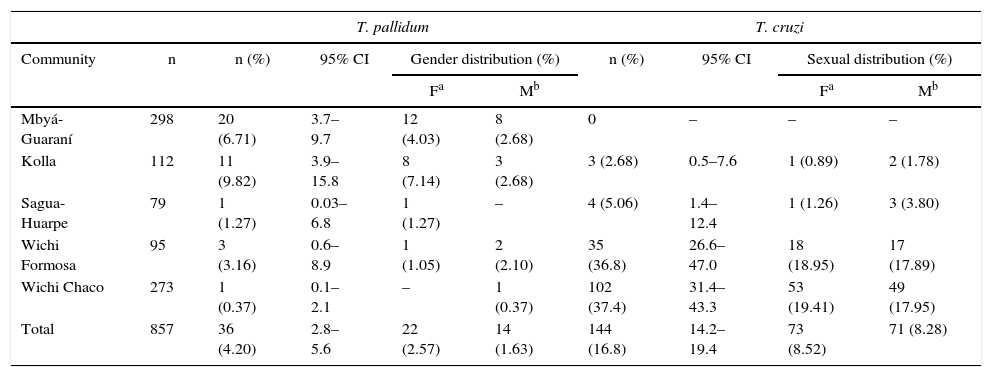
T. pallidum infection was detected in all the communities, with an overall prevalence rate of 4.2% (36/857; 95% CI: 2.8–5.6). Of the 36 positive samples, 22 were from women with no significant difference regarding gender. Prevalence ranged from 1.2% in the Wichi to 9.8% in the Kolla. T. pallidum infection in the Kolla (9.8%; 11/112; CI 95%: 3.9–15.8) was similar to that in the Mbyá-Guaraní (6.7%) (p>0.05), both significantly higher than the Wichi from Chaco (0.4%; 1/273; 95% CI.0.1–2.1) (p<0.05). Prevalence is described in Table 1.
Prevalence of T. pallidum and T. cruzi infections in five different Amerindian populations of Central and North Argentina
| T. pallidum | T. cruzi | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Community | n | n (%) | 95% CI | Gender distribution (%) | n (%) | 95% CI | Sexual distribution (%) | ||
| Fa | Mb | Fa | Mb | ||||||
| Mbyá-Guaraní | 298 | 20 (6.71) | 3.7–9.7 | 12 (4.03) | 8 (2.68) | 0 | – | – | – |
| Kolla | 112 | 11 (9.82) | 3.9–15.8 | 8 (7.14) | 3 (2.68) | 3 (2.68) | 0.5–7.6 | 1 (0.89) | 2 (1.78) |
| Sagua-Huarpe | 79 | 1 (1.27) | 0.03–6.8 | 1 (1.27) | – | 4 (5.06) | 1.4–12.4 | 1 (1.26) | 3 (3.80) |
| Wichi Formosa | 95 | 3 (3.16) | 0.6–8.9 | 1 (1.05) | 2 (2.10) | 35 (36.8) | 26.6–47.0 | 18 (18.95) | 17 (17.89) |
| Wichi Chaco | 273 | 1 (0.37) | 0.1–2.1 | – | 1 (0.37) | 102 (37.4) | 31.4–43.3 | 53 (19.41) | 49 (17.95) |
| Total | 857 | 36 (4.20) | 2.8–5.6 | 22 (2.57) | 14 (1.63) | 144 (16.8) | 14.2–19.4 | 73 (8.52) | 71 (8.28) |
T. cruzi was detected in all the communities, except in the Mbyá-Guaraní. The overall prevalence was 16.8% (144/857; 95% CI: 14.2–19.3), being significantly higher among the Wichi (37.4%) when compared to the Sagua-Huarpe (5.06%) and the Kolla (2.68%). No significant differences were observed when compared by gender (Table 1). Two cases of T. pallidum/T. cruzi co-infection were observed in the Wichi from Formosa. No HIV-1 cases were detected in these populations.
In this study, the presence of important public health pathogens is described among Amerindians of Argentina. Although the data is from samples that were preserved for years, this is the first time that T. pallidum infection is reported in 4 different aboriginal populations. T. pallidum prevalence was similar in the Kolla from the Northwest and the Mbyá-guaraní in the Northeast, and significantly higher than the ones detected in the other communities and in blood donors from the same areas and years. These data differ from two previous studies conducted in the 1990s where T. pallidum was not detected among the Kolla, the Wichi and the Mapuche from the South, with the exception of one case of a Toba from the Gran Chaco region in 19932,4. Little information is available regarding this infection, and in 2012 the Ministry of Health reported in Jujuy a prevalence of early and congenital syphilis of 12.8% and 2.82%, respectively, in concordance with our results11. In Argentina, the incidence of congenital syphilis varies significantly, reflecting the variety of social, cultural, and economic risk factors especially impacting the Northern provinces. Amerindian women are not used to undergoing prenatal checkups and the failure to detect and treat syphilitic women is directly linked to an increased risk for congenital syphilis9. This infection is considered to be endemic in Northeast Argentina. In 2006, Misiones Province was considered to account for the alarming 25% of syphilis cases in the country1. In this study, the prevalence was higher than that observed a decade before in pregnant women (2.1%) at the time of delivery when congenital syphilis was reported in newborns in 1997, and similar to the one recently reported among several Mbya-Guaranies (6.0%) along the province1.
In the Gran Chaco region, comprising Paraguay and the Argentine provinces of Chaco and Formosa, a prevalence of 1.2% was observed in this study and the few data reported for this area in 2011 were for congenital syphilis, where 0.5 cases every 1000 newborns were reported, representing a challenge for the public health system14.
In San Juan province the Ministry of Health reported a decrease in early syphilis over time, being about 0.13% by the end of 2014 and significantly lower compared to the results of this study13. It has to be considered that Amerindians are not included as a population in the reports from the Ministry of Health and there is no recent data about the prevalence of this infection in San Juan.
While very few data are available on Amerindians of neighboring countries, reports on aboriginal pregnant women from Brazil and Paraguay revealed a prevalence of syphilis of 2.8% and 1.6%; respectively6,10. Jujuy and Misiones communities showed the highest prevalence of syphilis, one possible explanation being the geographical proximity to endemic regions such as Paraguay and Brazil. Nowadays, T. pallidum rapid screening tests are available and were recently recommended for testing pregnant women by the Pan American Health Organization (PAHO), and could be easily implemented to control the infection in these communities14. Although most of the syphilis cases are found among HIV-1 infected patients, this is not the case in this study as no HIV-1 was detected in these populations.
T. cruzi infection is a major cause of morbidity in Argentina where 4% of the population has been diagnosed with Chagas’ disease. The Gran Chaco region is a known endemic area for Chagas’ disease, although no disease burden information for this region is available8. This T. cruzi infection was detected in four of the studied communities with higher prevalence in the Wichi from the Gran Chaco region compared to previous studies in blood donors and pregnant women12. The prevalence reported in 2003 (53.2%) and 2004 (57.2%) among the aborigines in Chaco was significantly higher to the one reported in this study in the same province (37.4%)8. The same was observed in Formosa in 2009 where a prevalence rate of 48.28% in the aborigines was reported, being significantly higher to that reported here. In 2015, a prevalence of 21.4% in blood donors from Chaco was reported, being significantly lower compared to the results in this study. Despite the bias of population size, and the presumable decrease in the infection in this population due to public health efforts to eradicate the vector in endemic areas, there are no data confirming this trend and there is still a need to reinforce this initiative for controlling the infection. Our results are also in concordance with the prevalence reported in rural areas of other neighboring countries such as Brazil, Bolivia and Paraguay, where the estimated numbers of T. cruzi cases are particularly high.
In this study, T. cruzi was not detected among the Mbyá-guaraní. This difference may be due to the geographic and climatic characteristics of this Eastern region and the effectiveness of the implemented measures, such as chemical treatment, vector surveillance, pregnancy controls, detection in newborns from infected mothers and blood bank control. The prevalence in Misiones is low and ranges from 2% in adults to 1.2% in children13. This region which is inhabited by the Mbyá-guraní, was declared by the World Health Organization (WHO) as being free of vectorial transmission in 2012. Although, the transmission of Chagas’ disease has demonstrated a second-generation congenital transmission route (from grandmother to mother to newborn) in vector-free areas. These data suggest that this route of transmission, other than classic vector-born spread, may occur both in endemic and non-endemic areas. In this context, a rapid screening test for T. cruzi infection in pregnant women would be useful in primary health care settings in order to provide a rapid diagnosis. Research about the risk of congenital T. cruzi infection and the effective detection of infected newborns (which is mandatory in Argentina) is also essential, as they must receive the anti-parasite treatment as soon as possible.
This study demonstrated the absence of HIV-1infection in these Amerindian populations probably due to the fact that most of the communities are still culturally isolated and have not acquired risky behaviors for HIV infection. It is important to highlight that the Mbyá-Guaraní settlement is only 5km away from Puerto Iguazú, a highly visited city, and the increasing economic needs have slowly exposed them to risky behaviors such as injecting drug use, as reported by one of its members.
On the contrary, the Kolla, despite residing in a very touristic place, strongly maintain their traditions and remain quite unaffected by the influence of urban behaviors, keeping and defending their cultural heritage. Moreover, the Wichi, live in extreme poverty, and have an almost inaccessible geographical location with very restricted interaction with other villages. The Sagua-Huarpe, despite residing close to the province capital city and having acquired the urban language and clothing, still maintain their own social organization and have minimal contact with its neighboring city. As reported in other South American countries, HIV has started to show its presence in the Amerindian populations and therefore, sooner or later, HIV-1 infection will become a problem for them6.
In summary, this study reveals a high rate of syphilis in the Amerindian communities of Misiones and Chagas’ disease in those of Chaco and Formosa. These results highlight the importance of designing and implementing an integral intervention program for the detection, clinical evaluation, treatment, control and prevention of these infections considering the cultural habits and socio-economic isolation of these communities. The health care system in these areas has to be strengthened and local personnel recruited, trained, and institutionalized.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Financial supportThis work was supported by the Institut Pasteur through Dr. Antoine Gessain, Agencia Nacional de Promoción Científica y Tecnológica (grant number PICT 0322), CONICET (grant number PIP 112 20110100644) and approved and supported by the INBIRS, UBA-CONICET.
Conflict of interestThe authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
The authors wish to thank the invaluable assistance provided by the Health Professional staff in each province and to the tribal leaders and all the individuals who voluntary participated in this study.