Percutaneous coronary intervention (PCI) has become one of the most commonly performed cardiac procedures in clinical practice. Due to improvement in outcomes, reduced acute complication rates, the need to reduce costs and the limited availability of hospital beds, elective PCI with same-day discharge has become an interesting option.
MethodsSinglecenter registry with a retrospective evaluation of all patients undergoing elective PCI who were discharged on the same day, from January 2009 to March 2012. The rates of major adverse cardiac events (death, myocardial infarction, target-vessel revascularization and stroke), in addition to stent thrombosis, vascular complications and re-hospitalization between hospital discharge and the first 30 days of follow-up were determined.
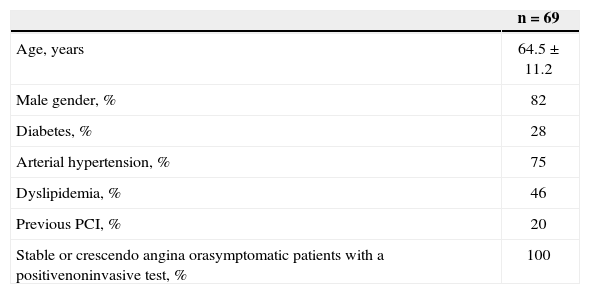
ResultsSixty-nine patients were evaluated with mean age of 64.5±11.2years, most of them were male (82%), and 28% were diabetics. All patients had stable coronary artery disease and type A or B1 lesions (36% and 36% respectively). Radial access was the most commonly used approach (89%), with 5F introducer sheaths in 56% and 6F in the remaining patients. Procedure success was obtained in 98.5%. No clinical events were observed at the 30-day follow-up.
ConclusionsOur results demonstrated that same-day discharge was safe for patients with low clinical and angiographic risk undergoing elective PCI with no procedure-related complications.
Desfechos Clínicos em 30 Dias dos PacientesSubmetidos a Intervenção Coronária Percutânea Eletiva com Alta no Mesmo Dia
IntroduçãoA intervenção coronária percutânea (ICP) tornou-se um dos procedimentos cardiológicos mais realizados na prática clínica. Em razão da melhoria dos resultados, da redução das complicações agudas, da necessidade de redução de custos e da pouca disponibilidade de leitos hospitalares, a ICP eletiva com alta no mesmo dia tornou-se uma opção interessante.
MétodosRegistro unicêntrico, que realizou avaliação retrospectiva de todos os pacientes submetidos a ICP eletiva e que receberam alta no mesmo dia, no período de janeiro de 2009 a março de 2012. Determinamos as taxas de eventos cardíacos adversos maiores (óbito, infarto do miocárdio, revascularização do vaso-alvo e acidente vascular cerebral), além de trombose do stent, complicações vasculares e reinternação no período compreendido entre a alta hospitalar e os primeiros 30 dias de acompanhamento.
ResultadosForam avaliados 69 pacientes, com média de idade de 64,5±11,2 anos, a maioria do sexo masculino (82%) e 28% diabéticos. Todos apresentavam quadros clínicos estáveis e lesões tipos A ou B1 (36% e 36%, respectivamente). A via de acesso radial foi a mais utilizada (89%), com introdutores 5F em 56% e 6F nos demais. Sucesso no procedimento foi obtido em 98,5%. No seguimento de 30 dias não foi identificado nenhum evento clínico.
ConclusõesNossos resultados demonstraram a segurança da alta no mesmo dia para pacientes de baixo risco tanto clínico como angiográfico, submetidos a ICP eletiva e que evoluíam sem complicações associadas ao procedimento.
Currently, percutaneous coronary intervention (PCI) is one of the most commonly performed cardiac procedures. The risks associated with PCI are low and generally occur within the first 24 to 48 hours after the procedure. Potential complications include abrupt vessel occlusion and its consequences, access route complications, and the management of comorbidities, such as contrast nephropathy and heart failure, among others. 1 In Brazil, patients who undergo PCI without complications are usually admitted to medical wards or semi-intensive or intensive units for 24 to 48 hours. This practice generates greater demand for hospital beds and increases costs, sometimes limiting the performance of the procedure. 2
The recent development of interventional cardiology, especially the optimization of implantable stents, the development of dual antiplatelet therapy, the reduction in the profile of materials, and the use of the transradial approach have improved PCI results and reduced complications. 3 This improvement in PCI has made it possible to have same-day discharge in select cases, after a short observation period. 4
Although same-day discharge is considered safe, and is used in other countries, 2,4 it is seldom used in Brazil. Therefore, this study aimed to evaluate the clinical outcomes of patients undergoing elective PCI with same-day discharge treated at a single center in Brazil.
METHODSStudy populationThis study included all patients undergoing PCI with same-day discharge between January 2009 and March 2012 at the Hemodynamics and Interventional Cardiology Service of Hospital Austa (Hemodinâmica AUSTACOR, São José do Rio Preto, Brazil). The patients had been previously evaluated by the haemodynamics specialist, who used the following inclusion criteria: 1) stable angina, crescendo angina, or asymptomatic patients with a positive test for ischemia; 2) absence of significant comorbidities such as heart failure, chronic renal failure (creatinine clearance<60mL/min), known coagulopathy or bleeding diathesis, chronic obstructive pulmonary disease, and allergy to contrast agents; 3) non-complex PCIs, preferentially with type A and B1 lesions according to the American College of Cardiology/American Heart Association (ACC/AHA) classification system; 4) absence of intraprocedure complications; 5) absence of prolonged chest pain or electrocardiographic alterations after PCI; 6) absence of vascular complications; and 7) PCI performed before the 13th hour of the day.
ProcedurePlatelet aggregation was facilitated with the use of clopidogrel at a loading dose of 300-600mg (with a recommendation for 600mg when the time between drug administration and intervention was less than 6 hours), followed by 75mg/day for at least 30 days for bare-metal stents (BMS) and one year for drug-eluting stents (DES). In addition, patients were prescribed acetylsalicylic acid (100-300mg/day) indefinitely. The procedure route was preferentially transradial, and femoral or brachial approaches (puncture) were alternatives in case the radial approach failed. After obtaining vascular access (5F or 6F) and introducing the catheter, unfractionated heparin was administered at a dose ranging from 70IU/kg to 100IU/kg. Glycoprotein IIb/IIIa inhibitors were not used.
Stent implantation followed the currently established technique, using direct stenting whenever possible. When necessary, predilation was performed with short balloons inflated at low pressures. The stent was implanted to ensure full lesion coverage, and when necessary, additional stents were used with overlapping edges. When needed, post-dilatation was performed with non-compliant balloons with lower extensions than that of the stent. During this process, the surgeons were careful not to overstep the stent’s edges, thereby avoiding injury to adjacent segments not covered by the stent.
After PCI, the sheaths were immediately removed. For the femoral approach, manual compression was used to prevent bleeding for 15 to 30 minutes, followed by a pressure dressing as well as resting the limb for at least four hours. In the case of the radial approach, a compressive dressing or band was used (TR Band; Terumo Medical Co. – Elkton, United States), while also resting the limb for two hours.
Post-procedural monitoring was performed with the use of an electrocardiogram (and compared to the ECG performed before the PCI), a vital sign assessment, and a physical examination of the access route. Enzyme measurement was not performed in patients without intra- or post-procedure complications. Patients who remained asymptomatic with no electrocardiographic alterations or abnormalities at the puncture site were discharged after receiving instructions on medication and possible complications and instructed to return to the cardiologist within seven days. In case of any signs or symptoms related to the procedure, patients were instructed to seek the emergency cardiology service of Hospital Austa.
Data collection and analysisData were collected by trained physicians using previously standardized forms. The collection included clinical characteristics, laboratory results, data from the invasive procedure, and clinical characteristics and changes until discharge. Information regarding later changes in patient status was recorded during ambulatory follow-ups at the involved center, review of hospital records, or telephone contact. Qualitative morphological characteristics were evaluated using standardized criteria.
Study aims and definitionsThe primary outcome assessed was the occurrence of major adverse cardiac events such as death, myocardial infarction (MI), target vessel revascularization, and stroke, as well as the rate of intrastent thrombosis, re-hospitalization, and vascular complications within 30 days.
Deaths included cardiac and non-cardiac causes. MI was defined by the presence of chest pain and persistent ST elevation>1mm in two contiguous leads or new left bundle branch blockage on the electrocardiogram. Target lesion revascularization was defined as a new intervention, surgical or percutaneous, with obstruction in lesions>50% within the implanted stent or in the segments 5mm proximal and 5mm distal to the stent. Intrastent thrombosis was defined according to the Academic Research Consortium classification based on degree of certainty as definite (angiographic or pathologic confirmation), probable (sudden death<30 days post-stenting or infarction related to the region of the treated artery without angiographic confirmation), or possible (sudden death within a period>30 days after stent implantation).
Regarding temporal occurrence, thromboses were classified as acute (0 to 24 hours) or subacute (24hours to 30 days). Angiographic success was defined as a reduction of the target lesion by<30% with maintenance or restoration of normal antegrade flow (Thrombolysis in Myocardial Infarction [TIMI] 3).5,6
Intraprocedure complications included prolonged chest pain, transient vessel occlusion, no-reflow and slow-flow phenomena, haemodynamic instability, occlusion of a major side branch (> 1.5mm), and suboptimal angiographic results. The lesions were classified into types A, B1, B2, and C, according to the ACC/AHA. Vascular complications included major bleeding according to TIMI classification (intracranial haemorrhage or decrease of haemoglobin>5mg/dL or of haematocrit by 15%), hematoma at the puncture site>5cm, pseudoaneurysm, fistula, or thrombosis requiring surgical intervention.
Statistical AnalysisData were entered and analysed in Excel spreads-heets (Microsoft Corp. – Redmond, USA). Categorical variables were described as frequencies and percentages, and continuous variables were described as the means and standard deviations.
RESULTSBetween January 2009 and March 2012, of 69 patients undergoing elective PCI with same-day discharge were found in our database. Subjects were mostly male (82%) and had a mean age of 64.5+11.2years; 28% were diabetic. Clinical presentation included stable angina, crescendo angina without biomarker elevation, or asymptomatic patients with a positive test for ischaemia (Table 1).
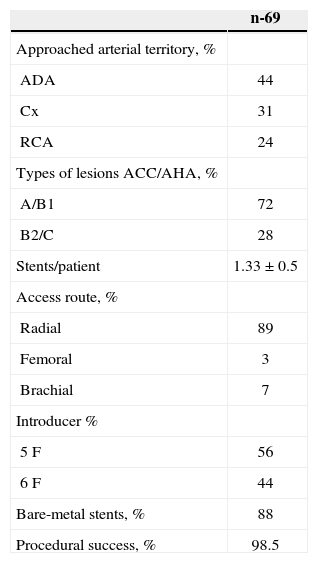
As shown in Table 2, the most frequent approach was the left anterior descending artery (44%), with a predominance of types A and B1 lesions (72%). The radial access route (89%) and 5F introducers (56%) were used in most cases. The mean number of stents per patient was 1.33±0.5; most of them were BMS. The angiographic success rate was 98.5%. There was only one case of failure, in which the lesion could not be passed with a guide wire. Bifurcation lesions, which require approaching the lateral branch and finishing with the kissing balloon technique, occurred in four patients.
Angiographic and procedural characteristics
| n-69 | |
|---|---|
| Approached arterial territory, % | |
| ADA | 44 |
| Cx | 31 |
| RCA | 24 |
| Types of lesions ACC/AHA, % | |
| A/B1 | 72 |
| B2/C | 28 |
| Stents/patient | 1.33±0.5 |
| Access route, % | |
| Radial | 89 |
| Femoral | 3 |
| Brachial | 7 |
| Introducer % | |
| 5F | 56 |
| 6F | 44 |
| Bare-metal stents, % | 88 |
| Procedural success, % | 98.5 |
ADA, anterior descending artery; Cx, circumflex artery; RCA, right coronary artery; ACC/AHA, American College of Cardiology/American Heart Association
Patient observation time was 6.8±1.3hours. After 30 days of follow-up, there were no major adverse cardiac events, intrastent thromboses, vascular complications, or re-hospitalizations.
DISCUSSIONThe risks of PCI complications, which occur in up to 5% of cases, generally include abrupt occlusion of the treated vessel and subsequent complications, such as MI, need for urgent revascularization, and/or death. This complication is associated with more complex patients, both from the clinical (acute coronary syndrome with and without ST-elevation) and angiographic points of view (very calcified lesions, bifurcation lesions, chronic occlusions, lesions in degenerated saphenous vein grafts). There are also risks of vascular access complications and contrast nephropathy. With the developments achieved by interventional cardiology, especially the improvements in techniques, materials, and medications, there has been a tendency to perform elective PCI with increasingly early hospital discharge. In these cases, patient selection is crucial, and the transradial access route is preferred. 7
Vascular access complications occur in 4% to 8% of cases, 3 and are more often associated with the use of the femoral access route, often requiring observation for at least 24 hours after the procedure. Femoral access route complications include haematoma, pseudoaneurysm, retroperitoneal haematoma, arteriovenous fistula, and vascular dissection. The choice of the radial access route reduces complications when compared to femoral access. Infrequent complications include pseudoaneurysm and compartment syndrome. 7
Contrast nephropathy after PCI affects 0% to>20% of cases, depending on the prevalence of risk factors and the definition used. Important risk factors for contrast-related nephropathy include older age, heart failure, diabetes, chronic renal failure, and volume of contrast agent used. To minimize the risk of contrastrelated nephropathy, current guidelines recommend that patients with creatinine clearance<60mL/min should receive additional hydration with intravenous 0.9% saline for three to 12 hours prior to PCI and for six to 24 hours after PCI, while also reducing the amount of contrast agent used.7
Studies evaluating same-day discharge have included over 5,000 patients, but there have only been three randomized trials that compared<2,000 total patients with same-day discharge vs. overnight stays.4 The first study evaluated 100 patients undergoing PCI via the femoral artery; it compared a group using a vascular occlusion device and discharged on the same day with a group submitted to mechanical compression that was discharged on the following day. There were no severe complications in either group, and approximately one-fifth of the patients randomized to same-day discharge needed to remain hospitalized until the following day due persistent bleeding in the access route.8
Subsequently, Heyde et al. 9 evaluated 800 patients undergoing elective PCI via the femoral approach, assessing patients four hours after the procedure to verify whether they were candidates for early discharge. Patients undergoing ad hoc PCI were excluded. The candidates for early discharge were randomized to immediate discharge vs. overnight stay. The combined incidence of adverse events (death, MI, coronary artery bypass graft surgery, PCI, or access route complications) occurred in one (0.3%) patient in the early discharge group and in two (0.6%) patients in the in-hospital group (p for noninferiority<0.0001).9
Finally, the Early Discharge After Transradial Stenting of Coronary Arteries (EASY) study compared 1,005 randomized patients successfully submitted to PCI using the transradial approach for same-day discharge vs. overnight stay. 10 All patients received abciximab in bolus, but only those who remained until the next day received the standard infusion of abciximab for 12 hours. Two-thirds of patients had clinical pictures of unstable angina, and 20% had high-risk acute coronary syndrome. Although the group with early discharge presented a numerically higher incidence of adverse events, same-day discharge was not statistically lower in comparison with the in-hospital group. The abciximab in bolus strategy used by some centers has not been adequately studied regarding its safety and efficacy. 4
The present study observed satisfactory results with low-risk patients who were evaluated and operated on by experienced surgeons with a trained staff, and who received meticulous care from the time of indication through surgery, and in the recovery room after the procedure. The post-procedure observation period of six to eight hours, with assessment of the access route and vital signs and symptoms, as well as pre- and postprocedural electrocardiogram evaluation, reinforced the safety criteria for same-day discharge. The measurement of cardiac biomarkers is no longer routinely recommended for all patients (class IIb, level of evidence C). It should be performed in patients with signs or symptoms of periprocedural MI in asymptomatic patients with angiographic complications (secondary branch occlusion, dissection, no-reflow, or stent thrombosis). 7
CONCLUSIONSSame-day hospital discharge, preceded by a short period of observation, is a safe and effective strategy for low-risk patients undergoing elective PCI that progressed without procedure-related complications.
CONFLICT OF INTERESTThe authors declare no conflicts of interest.