The transradial approach for percutaneous coronary intervention (PCI) is still not widely used in our country. We evaluated the results of transradial PCI performed at a tertiary hospital, which has progressively incorporated this technique to its daily clinical practice.
MethodsThis is a retrospective study of patients treated from 2007 to 2012 at Instituto Dante Pazzanese de Cardiologia. Clinical, angiographic and procedural profile and in-hospital outcomes of patients with stable and unstable coronary artery disease (CAD) treated with the transradial approach were compared.
ResultsWe included 2,507 patients, of which 72.6% had stable and 27.4% had unstable CAD. Patients with stable CAD had a more complex clinical profile, characterized by being older, more frequently females, with a higher incidence of comorbidities. The angiographic and procedural characteristics were not different for most of the variables analyzed. The success rate was high, but higher in the stable CAD group (94.6% vs. 92.4%; P = 0.05). The incidence of death (0.2% vs. 0.3%; P = 0.61), peri-procedural infarction (4.7% vs. 6.6%; P = 0.07), stroke (0.1% vs. 0.1%; P > 0.99), PCI (0.1% vs. 0.3%; P = 0.30), coronary artery bypass graft (0 vs. 0.4%; P = 0.06), major bleeding (0.2% vs. 0.6%; P = 0.09) or vascular complications (1% vs. 0.6%; P = 0.47) was low and did not differ between groups.
ConclusionsTransradial PCI has proved to be safe and effective in patients with stable and unstable CAD, treated at a tertiary hospital that has progressively incorporated this technique to its daily practice.
Comparação da Intervenção Coronária Percutâneapor Via Radial em Pacientes com Doença Arterial Coronária Estável e Instável
IntroduçãoA intervenção coronária percutânea (ICP) por via radial ainda é pouco utilizada em nosso meio. Avaliaram-se aqui os resultados da ICP por via radial, realizada em um hospital terciário, que, progressivamente, tem incorporado tal técnica à prática clínica diária.
MétodosEstudo retrospectivo, de pacientes tratados entre 2007 e 2012, no Instituto Dante Pazzanese de Cardiologia. Compararam-se os perfis clínico, angiográfico e do procedimento e os resultados hospitalares dos pacientes tratados por via radial com doença arterial coronária (DAC) estável e instável.
ResultadosForam incluídos 2.507 pacientes, sendo 72,6% portadores de DAC estável e 27,4% de DAC instável. Os pacientes portadores de DAC estável tinham perfil clínico mais complexo, caracterizado por serem mais idosos, mais frequentemente do sexo feminino e com maior incidência de comorbidades. As características angiográficas e do procedimento não mostraram diferenças na maioria das varáveis analisadas. A taxa de sucesso foi elevada, porém maior no grupo DAC estável (94,6% vs. 92,4%; P = 0,05). A incidência de óbito (0,2% vs. 0,3%; P = 0,61), infarto periprocedimento (4,7% vs. 6,6%; P = 0,07), acidente vascular cerebral (0,1% vs. 0,1%; P > 0,99), ICP (0,1% vs. 0,3%; P = 0,30), cirurgia de revascularização miocárdica (0 vs. 0,4%; P = 0,06), sangramento maior (0,2% vs. 0,6%; P = 0,09) ou complicação vascular (1% vs. 0,6%; P = 0,47) foi baixa e não diferiu entre os grupos.
ConclusõesICP por via radial mostrou-se segura e eficaz, tanto em pacientes com DAC estável como instável, tratados em hospital terciário que progressivamente tem incorporado essa técnica à rotina diária.
The transradial approach for percutaneous coronary intervention (PCI) was originally introduced by Kiemeneij et al.1 Its benefits, including reduced complications of the puncture site, early ambulation, and diminished hospitalisation time, have been demonstrated in several trials conducted in Brazilian centers and in other countries.2−10
Among all the potential benefits of this type of access, safety is undoubtedly the most attractive. With radial access, hemorrhagic and vascular complications (bleeding, pseudoaneurysm, arteriovenous fistula, and bruising) are rare and generally easily circumvented. However, the occurrence of complications is influenced by the learning curve.2,10
The transradial approach is still not routinely used in interventional cardiology centers for diagnostic and therapeutic procedures. Globally, less than 10% of the procedures are performed by this route.11 The Registro Central Nacional de Intervenções Cardiovasculares (Central Brazilian Registry of Cardiovascular Interventions – CENIC) showed that in 2008, only 12.6% of the procedures were performed by this technique in Brazil.2 Previous trials have shown that, in the beginning of the learning curve, technical failures and the necessity of crossover to the femoral technique are relatively frequent.12,13
Most trials evaluating the transradial approach compared to the femoral route revealed benefits in the presence of unstable coronary artery disease (CAD), especially in ST-segment elevation myocardial infarction (STEMI), because these patients have greater probability of bleeding from the access route, due to the adjunct medication used (antiplatelet, antithrombotic, thrombolytic, etc.).
The aim of this study was to evaluate the in-hospital results of PCI by transradial approach, performed in a busy tertiary hospital that has progressively incorporated this technique into daily clinical practice, comparing patients with stable and unstable CAD.
METHODSThis was a retrospective study, using the database of a consecutive series of patients with stable CAD (stable angina or silent ischemia) and unstable CAD (with or without ST-segment elevation), treated with PCI by radial approach with 6F catheter at Instituto de Cardiologia Dante Pazzanese, São Paulo, Brazil, from December of 2007 to October of 2012.
Data from hospital outcomes were entered on a standardized form, comprising clinical, angiographic, and procedural characteristics, in addition to the clinical evolution of the patient until discharge.
ProcedureThrough wrist hyperextension and infiltration of 1-2mL of 2% xylocaine, the radial artery was punctured 1cm proximal to the radial styloid process using a needle with a polyethylene catheter (Jelco® n° 20-22) and using the Seldinger technique. After the puncture, a 0.021-inch guidewire was introduced, followed by a small skin incision with a scalpel blade and insertion of a 6F sheath. A solution containing 5,000IU heparin sulphate was administered through the sheath. At the end of the procedure, the sheath was immediately removed, and hemostasis was obtained with a compression band, the TR BandTM (Terumo Medical – Tokyo, Japan). A clinical examination of the puncture site and an evaluation of the radial pulse were performed at the time of hospital discharge.
DefinitionsAngiographic success was defined as a reduction of the target lesion to a stenosis diameter < 30%, with maintenance or restoration of the normal antegrade flow (Thrombolysis in Myocardial Infarction [TIMI] 3). 14−16 Procedural success was considered when angiographic success and the absence of major clinical complications (death, nonfatal myocardial infarction [MI], or emergency coronary artery bypass graft [CABG] surgery) were obtained.
MI associated with the procedure was defined as the development of new Q waves and/or elevation of CK-MB (> three times the baseline level).
Vascular complications were defined as presence of hematoma > 10cm at the site of arterial puncture; major bleeding, characterized as a fall in hemoglobin > 3g/dL or a need for red blood cells transfusion; or a need for surgical correction of complications (hematoma, pseudoaneurysm, or arteriovenous fistula formation).
Statistical analysisThe SPSS for Windows was used for statistical analysis. Qualitative variables were presented as absolute and relative frequencies, and compared with the chi-squared or Fisher’s exact test. Quantitative variables were described as means and standard deviations. To test the groups, the Kolmogorov-Smirnov test was used to check the normality of the data. When the distribution was normal, Student’s t-test was used. Otherwise, the Wilcoxon test was used. The level of significance was set at 5%.
RESULTSDuring the study period, from December of 2007 to October of 2012, 2,507 consecutive patients were treated with PCI by transradial approach with 6F catheter; 1,821 (72.6%) had a clinical diagnosis of stable CAD, and 686 (27.4%) of unstable CAD.
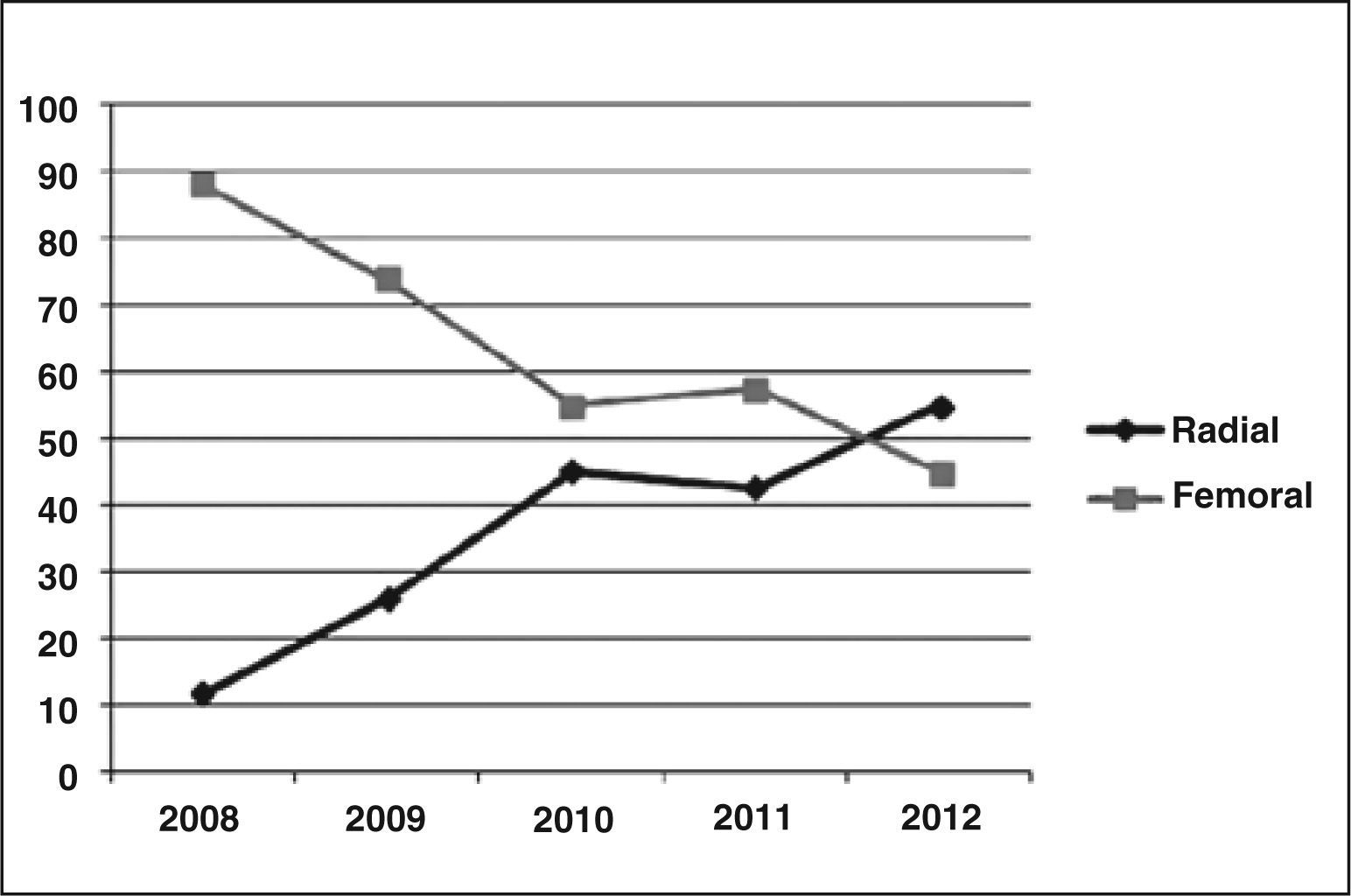
In the present service, there was a progressive increase in the use of the transradial approach for performing PCI until 2010, stabiliszing in 2010 and 2011, and surpassing the femoral approach by 2012 (11.8% in 2008, 26.1% in 2009, 45.1% in 2010, 42.6% in 2011, and 55% in 2012) (Figure 1).
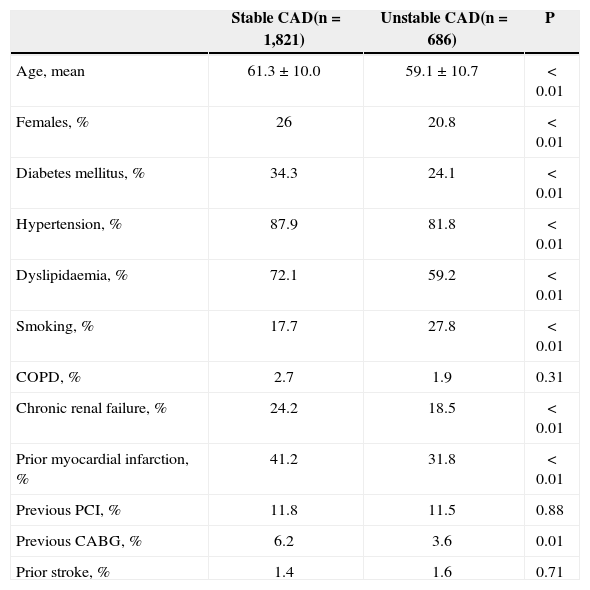
Patients with stable disease had a more complex clinical profile, characterized by older age, female gender, and higher incidence of comorbidities such as diabetes, systemic hypertension, dyslipidaemia, chronic renal failure, previous MI, and previous CABG, when compared with those of the group with unstable CAD (Table 1).
Demographic and clinical characteristics
| Stable CAD(n = 1,821) | Unstable CAD(n = 686) | P | |
|---|---|---|---|
| Age, mean | 61.3 ± 10.0 | 59.1 ± 10.7 | < 0.01 |
| Females, % | 26 | 20.8 | < 0.01 |
| Diabetes mellitus, % | 34.3 | 24.1 | < 0.01 |
| Hypertension, % | 87.9 | 81.8 | < 0.01 |
| Dyslipidaemia, % | 72.1 | 59.2 | < 0.01 |
| Smoking, % | 17.7 | 27.8 | < 0.01 |
| COPD, % | 2.7 | 1.9 | 0.31 |
| Chronic renal failure, % | 24.2 | 18.5 | < 0.01 |
| Prior myocardial infarction, % | 41.2 | 31.8 | < 0.01 |
| Previous PCI, % | 11.8 | 11.5 | 0.88 |
| Previous CABG, % | 6.2 | 3.6 | 0.01 |
| Prior stroke, % | 1.4 | 1.6 | 0.71 |
CAD = coronary artery disease; COPD = chronic obstructive pulmonary disease; PCI = percutaneous coronary intervention; CABG = coronary artery bypass grafting.
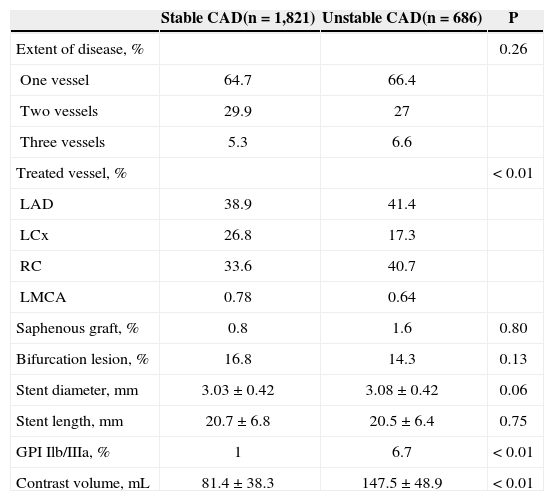
Regarding angiographic characteristics, most analyzed variables showed no differences between groups. Approximately one-third of the population had involvement of two or three vessels, and the left anterior descending artery was the most frequently treated vessel. The characteristics of the procedure also showed no differences in the diameter and length of the stent used. The use of glycoprotein IIb/IIIa inhibitors was sparse, and was more frequent in the unstable CAD group (Table 2).
Angiographic and procedural characteristics
| Stable CAD(n = 1,821) | Unstable CAD(n = 686) | P | |
|---|---|---|---|
| Extent of disease, % | 0.26 | ||
| One vessel | 64.7 | 66.4 | |
| Two vessels | 29.9 | 27 | |
| Three vessels | 5.3 | 6.6 | |
| Treated vessel, % | < 0.01 | ||
| LAD | 38.9 | 41.4 | |
| LCx | 26.8 | 17.3 | |
| RC | 33.6 | 40.7 | |
| LMCA | 0.78 | 0.64 | |
| Saphenous graft, % | 0.8 | 1.6 | 0.80 |
| Bifurcation lesion, % | 16.8 | 14.3 | 0.13 |
| Stent diameter, mm | 3.03 ± 0.42 | 3.08 ± 0.42 | 0.06 |
| Stent length, mm | 20.7 ± 6.8 | 20.5 ± 6.4 | 0.75 |
| GPI Ilb/IIIa, % | 1 | 6.7 | < 0.01 |
| Contrast volume, mL | 81.4 ± 38.3 | 147.5 ± 48.9 | < 0.01 |
CAD = coronary artery disease; LAD = left anterior descending, LCx = left circumflex artery; RC = right coronary artery; LMCA = left main coronary artery; GPI = glycoprotein receptor inhibitor.
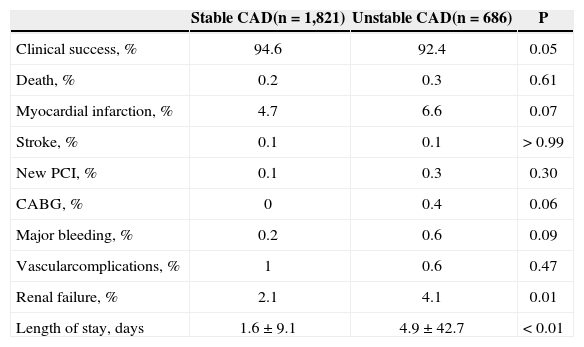
The in-hospital outcomes are shown in Table 3. The success rate was high in both groups, but higher among patients with stable CAD (94.6% vs. 92.4%; P = 0.05). The death rate was low and did not differ between groups (0.2% vs. 0.3%; P = 0.61), as did rates of periprocedural MI (4.7% vs. 6.6%; P = 0.07), stroke (0.1% vs. 0.1%; P > 0.99), PCI (0.1% vs. 0.3%, P = 0.30), CABG (0.4% vs. 0%; P = 0.06), major bleeding (0.2% vs. 0.6%; P = 0.09), or vascular complications (1% vs. 0.6%; P = 0.47). There was a lower incidence of nephropathy induced by contrast in the stable CAD group (2.1% vs. 4.1%; P = 0.01), whereas in the unstable CAD group a greater number of ad hoc interventions occurred, which justifies the higher volume of contrast in this group.
In-hospital outcomes
| Stable CAD(n = 1,821) | Unstable CAD(n = 686) | P | |
|---|---|---|---|
| Clinical success, % | 94.6 | 92.4 | 0.05 |
| Death, % | 0.2 | 0.3 | 0.61 |
| Myocardial infarction, % | 4.7 | 6.6 | 0.07 |
| Stroke, % | 0.1 | 0.1 | > 0.99 |
| New PCI, % | 0.1 | 0.3 | 0.30 |
| CABG, % | 0 | 0.4 | 0.06 |
| Major bleeding, % | 0.2 | 0.6 | 0.09 |
| Vascularcomplications, % | 1 | 0.6 | 0.47 |
| Renal failure, % | 2.1 | 4.1 | 0.01 |
| Length of stay, days | 1.6 ± 9.1 | 4.9 ± 42.7 | < 0.01 |
CAD = coronary artery disease; PCI = percutaneous coronary intervention; CABG = coronary artery bypass grafting.
The hospital stay was significantly lower in the group with stable CAD (1.6 ± 9.1 days vs. 4.9 ± 42.7 days; P < 0.01). 73% of all patients were discharged the next day after the procedure.
DISCUSSIONThe main finding of the present study was that the transradial approach used in clinical practice in a tertiary hospital is safe and effective, both in patients with stable CAD and with unstable CAD. This access point minimizes the risk of bleeding and vascular complications, equalising such different populations, despite the adjunctive medication used.
The transradial approach is associated with a dramatic reduction in the risk of complications of the approach route when compared to the transfemoral route. Growing evidence in several trials demonstrate a significant reduction in major adverse cardiovascular events when the transradial approach is used, mainly in the STEMI scenario.17 The transradial approach is particularly attractive in primary PCI, when this technique is performed by experienced surgeons, since these patients are treated with a more aggressive antiplatelet and antithrombotic regimen, resulting in a reduction of bleeding complications and, subsequently, of major adverse cardiovascular events.
Specifically in the treatment of unstable CAD, Romagnoli et al.18 demonstrated that, in 30 days, the use of the radial access reduced the cardiovascular death, incidence of bleeding, and length of hospital stay, findings similar to those observed in a meta-analysis involving 21 trials and 8,534 patients.19 The analysis of the same population, in the RIVAL trial, also demonstrated benefit in reducing the mortality, but this finding was limited to the subgroup with ST-segment elevation.17
This study also showed a reduced incidence of bleeding and vascular complications related to the radial route, as was previously demonstrated in a number of trials published recently.5,6,17
In this study of a real-world population, it was shown that the choice of the radial access for PCI still is less used than the femoral access, but now accounts for nearly half of all interventions at this institution, reflecting the progressive incorporation of the knowledge acquired with the method.
Limitations of the studyThis was a retrospective, observational, single-center study, with all the limitations inherent in this type of study, in which the decision with respect to the approach used was responsibility of the surgeon, based on the experience acquired, clinical profile of the patient, and vascular condition of the site. However, for the same reasons, this may have been the best way to reproduce the daily practice of a coronary intervention laboratory.
CONCLUSIONSThe use of percutaneous coronary intervention by transradial approach was safe and effective, both in patients with stable and unstable coronary artery disease treated at a tertiary care hospital that has progressively incorporated this technique into daily clinical practice. This entry point minimized the risk of bleeding and vascular complications, equalising such distinct populations, regardless of the adjunctive medication used.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.