The percutaneous treatment of coronary artery disease has been revolutionized by the use of drug-eluting stents (DES). However, its use in the daily practice involves patients with more complex clinical and angiographic characteristics than those found in randomized trials. This registry was designed to characterize diabetic patients and their outcomes following DES implantation in our country.
MethodsProspective single-center registry enrolling consecutive patients after DES implantation. Clinical, angiographic and procedurerelated data, as well as early and long-term outcomes were recorded. The primary endpoint, including cardiac death, myocardial infarction or target lesion revascularization, was compared between diabetics and non-diabetics.
ResultsWe evaluated 1,670 patients treated with DES from 2002 to 2012 with a follow-up of 3.2±2.5years. One third of the patients were diabetic and had lower event-free survival when compared to non-diabetic patients (79.4% vs. 82.6%; P=0.015). The adjusted odds ratio, however, was 1.22 (95% CI, 0.89-1.69) and was not significant. A significantly lower event-free survival was observed in the subgroup of patients receiving insulin, whereas it was similar for diabetic and nondiabetic patients in the subgroup not receiving insulin (68.7% vs. 83.9% vs. 82.8%, respectively; P < 0.01). The adjusted odds ratio was 1.72 (95% CI, 1.13-2.63) higher for diabetic patients receiving insulin when compared to the remaining patients.
ConclusionsThe use of DES is beneficial for all diabetic patients, especially those who do not receive insulin.
Resultados Iniciais e Tardios deDiabéticos Tratados com Stents Farmacológicos do Registro Safira
IntroduçãoO tratamento percutâneo da doença arterial coronária foi revolucionado pelo uso dos stents farmacológicos (SF). No entanto, sua utilização na prática diária envolve pacientes com características clínicas e angiográficas mais complexas dos que aquelas encontradas em estudos randomizados. Este registro se propôs a caracterizar, em nosso meio, diabéticos e seus desfechos clínicos após implante de SF.
MétodosRegistro unicêntrico, prospectivo, que arrolou pacientes consecutivos submetidos a implante de SF. Foram registrados dados clínicos, angiográficos e do procedimento, assim como os desfechos hospitalares e tardios. A avaliação do desfecho primário, composto por óbito cardíaco, infarto agudo do miocárdio ou revascularização da lesão-alvo, foi realizada comparando-se pacientes diabéticos e não diabéticos.
ResultadosAvaliamos 1.670 pacientes tratados com SF no período de 2002 a 2012, com seguimento de 3,2±2,5 anos. Um terço dos pacientes era diabético e apresentou sobrevivência livre de eventos menor que os não diabéticos (79,4% vs. 82,6%; P=0,02). A razão de risco ajustada, no entanto, foi de 1,22 (IC 95%, 0,89-1,69) - não significativa. Ao analisar o subgrupo dos pacientes em uso de insulina, encontramos sobrevivência livre de eventos significativamente menor que a dos demais, enquanto que os diabéticos que não estavam em uso de insulina mostraram comportamento semelhante ao dos não diabéticos (68,7% vs. 83,9% vs. 82,8%, respectivamente; P < 0,01). A razão de risco ajustada foi 1,72 (IC 95%, 1,13-2,63) vez maior para os diabéticos em uso de insulina em comparação aos demais pacientes.
ConclusõesO uso de SF traz benefícios para todos os diabéticos, especialmente para os que não utilizam insulina.
The technology that enabled the coating of metallic stents with drugs has revolutionized interventional cardiology. Drug-eluting stents (DES) have the ability to reduce neointimal hyperplasia, decreasing the coronary restenosis and the need for subsequent revascularizations.1 With such benefits, these new devices have expanded the indications for percutaneous treatment for lesions and in more complex patients.2
However, despite their routine use, there are still doubts about the results of DES in the population that usually presents clinical and angiographic criteria not included in randomized clinical trials. Another important aspect to note is the lack of data from the Brazilian population, whose own cultural and social characteristics influence the adherence to treatment, besides the fact that its genetic composition differs from populations assessed in the large registries of the United States and Europe.3−6
The aim of the present study was to evaluate the initial and late events of a non-selected cohort of patients undergoing DES implantation, comparing diabetic and non-diabetic patients.
METHODSThis was a single-center prospective trial of consecutive patients with coronary artery disease treated with at least one DES from July 2002 to August 2012 in the Complexo Hospitalar, Real e Benemérita Sociedade Portuguesa de Beneficência, Hospitais São Joaquim e São José, and in the Interventionist Cardiology Service Ariê, in the city of São Paulo, SP, Brazil. Patients were included in the study after explanation, reading, and signing of the informed consent. The protocol for this project was duly approved by the research ethics committee under number 778-12, as was the informed consent form.
Inclusion and exclusion criteriaPatients≥18 years old, with indication for CABG regardless of clinical or angiographic picture, and who could be treated with available DES, were included. Patients with contraindications to the use of antiplatelet medication indicated by the pharmacological protocol and those who refused to sign the informed consent were excluded.
Procedure and antiplatelet therapyPercutaneous coronary interventions (PCIs) were performed according to the technique recommended by the guidelines.7 The choice of the stent was left to the surgeons’ discretion.
The antiplatelet protocol consisted of a combination of two antiplatelet agents, acetylsalicylic acid (ASA) and a P2Y12 inhibitor. ASA was used at a loading dose of 200mg and 100mg for maintenance; clopidogrel was used at a loading dose of 300-600mg and 75mg for maintenance. With the availability of ticagrelor and prasugrel, these drugs have been incorporated into clinical practice at loading doses of 60 and 180mg, and maintenance at 90mg twice daily and 10mg, respectively. The P2Y12 inhibitors have been recommended for a minimum period of one year. The use of glycoprotein IIb/IIIa inhibitors was at the discretion of the surgeon.
Definitions and primary outcomeThe clinical follow-up was performed by medical consultation or telephone contact at 30 days, six months, one year, and annually thereafter. Adverse events were reviewed using data from medical records and reports from other hospitals where the adverse event occurred.
The diagnosis of diabetes was defined, in accordance with current consensus, as a fasting glucose≥126mg/dL, glycaemia≥200mg/dL two hours after ingestion of 75g glucose (glucose tolerance test), random blood glucose≥200mg/dL accompanied by symptoms of hyperglycaemia.8 The patients were also classified according to whether or not they needed insulin treatment.
Deaths were considered of cardiac origin, unless a noncardiac cause could be unequivocally established. Acute myocardial infarction (AMI) was defined as an increase in creatine kinase fraction MB (CK-MB) superior to three times the upper limit of normal, with or without the appearance of new Q waves.9 Target vessel revascularization (TVR) was defined as the ischemia-guided revascularization of the vessel treated at the index PCI, whether by new PCI or coronary artery bypass graft (CABG), in the presence of symptoms or ischemia during the noninvasive stratification. Angiographic success was defined as achieving a stenosis diameter < 20% and Thrombolysis in Myocardial Infarction (TIMI) 3 flow. Procedural success was considered as angiographic success free of occurrence of death, AMI, or urgent TVR. The definition of TIMI bleeding was used to classify possible bleeding.10
The primary outcome was considered as the occurrence of cardiovascular death, nonfatal AMI, or ischemia-driven TVR in the late phase.
Statistical analysisContinuous variables were presented as means and standard deviations and were compared by Student’s t-test. Categorical variables were described as frequency and percentage, and were compared by the chi-squared or Fisher’s exact test, where appropriate. Cumulative event rates were estimated by the Kaplan-Meier method, and differences were compared by log-rank test. Patients were followed-up until the occurrence of an outcome, or censored in December 2012. Statistical significance was considered at a level of 5% (P≤0.05).
Multivariate predictors of outcomes were tested using the proportional hazards model of Cox when they showed significant effects in the univariate model (P < 0.15). The predictors included in the model were age, gender, body mass index, hypertension, smoking state, dyslipidaemia, diabetes mellitus, prior AMI, previous stroke, peripheral vascular disease, previous revascularization, chronic renal failure, ventricular dysfunction, extent of coronary artery disease, treated vessel, type of injury, segmental or calcified lesions, treatment for venous and arterial grafts, stenosis diameter pre- and post-procedure, implantation technique of direct stent, and stent type.
Left ventricular dysfunction was defined according to a four-point scale (normal, mild dysfunction, moderate dysfunction, or severe dysfunction). The results are presented as risk ratio (RR) and 95% confidence interval (95% CI). The proportional hazards assumption was confirmed by testing Schoenfeld residuals; no violations were found.
All analyses were performed using Stata (StataCorp – Texas, USA), version 12.
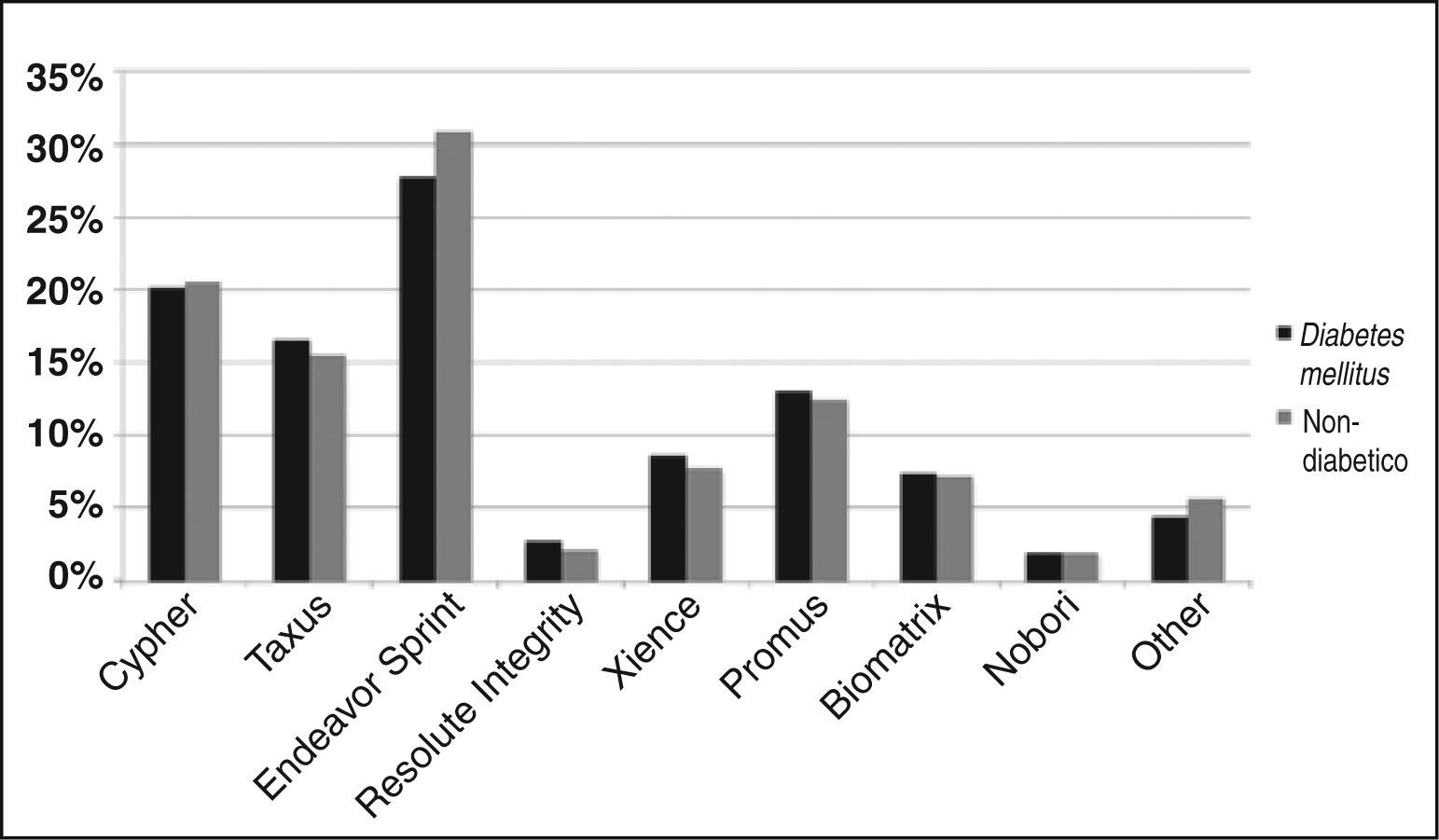
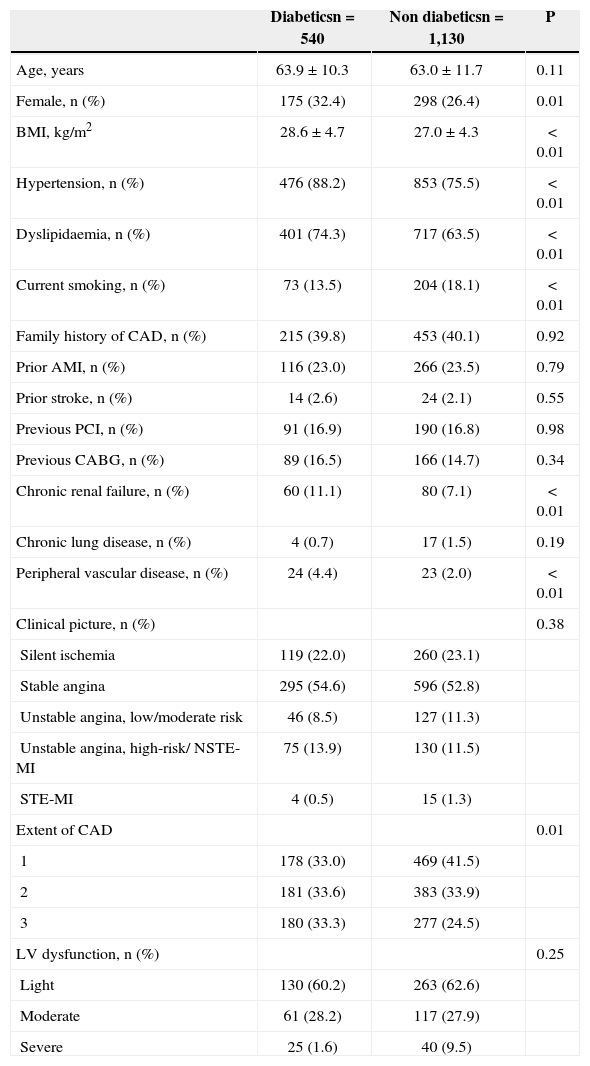
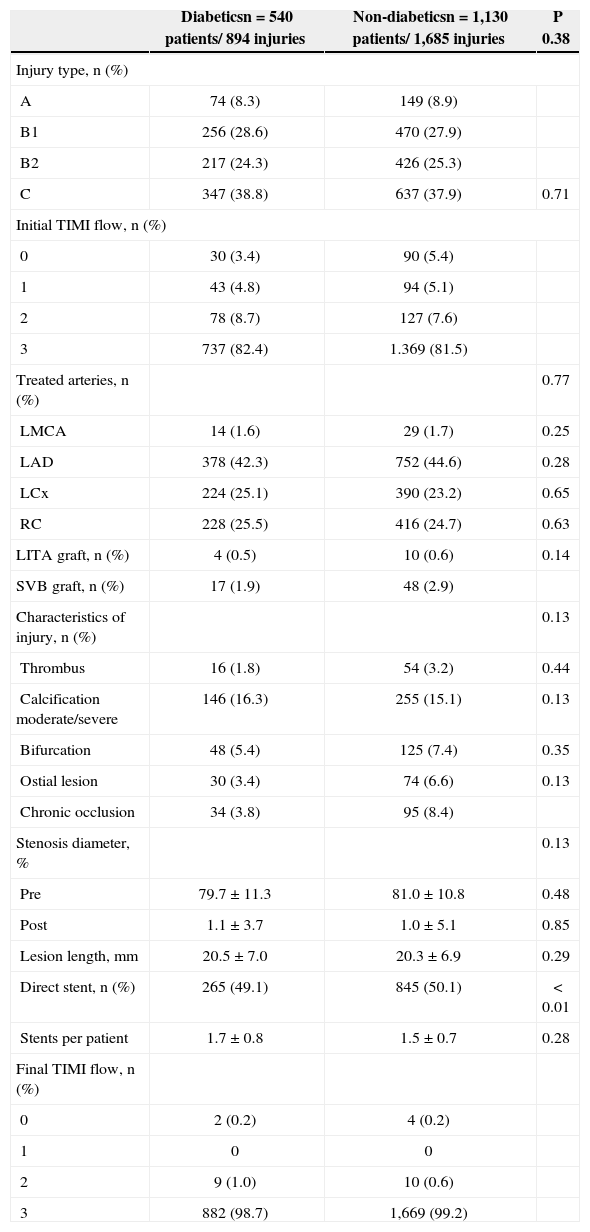
RESULTSDuring the reporting period, 1,670 patients underwent PCI only by DES implantation. Clinical, angiographic, and procedural characteristics are shown in Tables 1 and 2, and in Figure 1. Of these patients, 540 (32.3%) had diabetes mellitus; 70.2% were under treatment with oral hypoglycaemic agents and 29.8% with insulin.
Clinical and angiographic characteristics
| Diabeticsn=540 | Non diabeticsn=1,130 | P | |
|---|---|---|---|
| Age, years | 63.9±10.3 | 63.0±11.7 | 0.11 |
| Female, n (%) | 175 (32.4) | 298 (26.4) | 0.01 |
| BMI, kg/m2 | 28.6±4.7 | 27.0±4.3 | < 0.01 |
| Hypertension, n (%) | 476 (88.2) | 853 (75.5) | < 0.01 |
| Dyslipidaemia, n (%) | 401 (74.3) | 717 (63.5) | < 0.01 |
| Current smoking, n (%) | 73 (13.5) | 204 (18.1) | < 0.01 |
| Family history of CAD, n (%) | 215 (39.8) | 453 (40.1) | 0.92 |
| Prior AMI, n (%) | 116 (23.0) | 266 (23.5) | 0.79 |
| Prior stroke, n (%) | 14 (2.6) | 24 (2.1) | 0.55 |
| Previous PCI, n (%) | 91 (16.9) | 190 (16.8) | 0.98 |
| Previous CABG, n (%) | 89 (16.5) | 166 (14.7) | 0.34 |
| Chronic renal failure, n (%) | 60 (11.1) | 80 (7.1) | < 0.01 |
| Chronic lung disease, n (%) | 4 (0.7) | 17 (1.5) | 0.19 |
| Peripheral vascular disease, n (%) | 24 (4.4) | 23 (2.0) | < 0.01 |
| Clinical picture, n (%) | 0.38 | ||
| Silent ischemia | 119 (22.0) | 260 (23.1) | |
| Stable angina | 295 (54.6) | 596 (52.8) | |
| Unstable angina, low/moderate risk | 46 (8.5) | 127 (11.3) | |
| Unstable angina, high-risk/ NSTE-MI | 75 (13.9) | 130 (11.5) | |
| STE-MI | 4 (0.5) | 15 (1.3) | |
| Extent of CAD | 0.01 | ||
| 1 | 178 (33.0) | 469 (41.5) | |
| 2 | 181 (33.6) | 383 (33.9) | |
| 3 | 180 (33.3) | 277 (24.5) | |
| LV dysfunction, n (%) | 0.25 | ||
| Light | 130 (60.2) | 263 (62.6) | |
| Moderate | 61 (28.2) | 117 (27.9) | |
| Severe | 25 (1.6) | 40 (9.5) |
BMI=body mass index; CAD=coronary artery disease; AMI=acute myocardial infarction; PCI=percutaneous coronary intervention; NSTE-MI=myocardial infarction without ST-segment elevation; STE-MI=myocardial infarction with ST-segment elevation; LV=left ventricle.
Angiographic and procedural characteristics
| Diabeticsn=540 patients/ 894 injuries | Non-diabeticsn=1,130 patients/ 1,685 injuries | P 0.38 | |
|---|---|---|---|
| Injury type, n (%) | |||
| A | 74 (8.3) | 149 (8.9) | |
| B1 | 256 (28.6) | 470 (27.9) | |
| B2 | 217 (24.3) | 426 (25.3) | |
| C | 347 (38.8) | 637 (37.9) | 0.71 |
| Initial TIMI flow, n (%) | |||
| 0 | 30 (3.4) | 90 (5.4) | |
| 1 | 43 (4.8) | 94 (5.1) | |
| 2 | 78 (8.7) | 127 (7.6) | |
| 3 | 737 (82.4) | 1.369 (81.5) | |
| Treated arteries, n (%) | 0.77 | ||
| LMCA | 14 (1.6) | 29 (1.7) | 0.25 |
| LAD | 378 (42.3) | 752 (44.6) | 0.28 |
| LCx | 224 (25.1) | 390 (23.2) | 0.65 |
| RC | 228 (25.5) | 416 (24.7) | 0.63 |
| LITA graft, n (%) | 4 (0.5) | 10 (0.6) | 0.14 |
| SVB graft, n (%) | 17 (1.9) | 48 (2.9) | |
| Characteristics of injury, n (%) | 0.13 | ||
| Thrombus | 16 (1.8) | 54 (3.2) | 0.44 |
| Calcification moderate/severe | 146 (16.3) | 255 (15.1) | 0.13 |
| Bifurcation | 48 (5.4) | 125 (7.4) | 0.35 |
| Ostial lesion | 30 (3.4) | 74 (6.6) | 0.13 |
| Chronic occlusion | 34 (3.8) | 95 (8.4) | |
| Stenosis diameter, % | 0.13 | ||
| Pre | 79.7±11.3 | 81.0±10.8 | 0.48 |
| Post | 1.1±3.7 | 1.0±5.1 | 0.85 |
| Lesion length, mm | 20.5±7.0 | 20.3±6.9 | 0.29 |
| Direct stent, n (%) | 265 (49.1) | 845 (50.1) | < 0.01 |
| Stents per patient | 1.7±0.8 | 1.5±0.7 | 0.28 |
| Final TIMI flow, n (%) | |||
| 0 | 2 (0.2) | 4 (0.2) | |
| 1 | 0 | 0 | |
| 2 | 9 (1.0) | 10 (0.6) | |
| 3 | 882 (98.7) | 1,669 (99.2) | |
TIMI=Thrombolys in Myocardial Infarction; LMCA=left main coronary artery;LA D=left anterior descendent artery; LCx=artery; RC=right coronary artery; LITA=left internal thoracic artery; SVB=saphenous vein bridge.
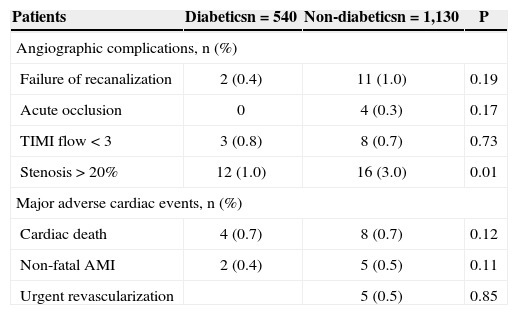
Angiographic success was achieved in 98.2% and procedural success in 96.7% of patients. The in-hospital results are shown in Table 3.
Angiographic and clinical complications in in-hospital phase
| Patients | Diabeticsn=540 | Non-diabeticsn=1,130 | P |
|---|---|---|---|
| Angiographic complications, n (%) | |||
| Failure of recanalization | 2 (0.4) | 11 (1.0) | 0.19 |
| Acute occlusion | 0 | 4 (0.3) | 0.17 |
| TIMI flow<3 | 3 (0.8) | 8 (0.7) | 0.73 |
| Stenosis>20% | 12 (1.0) | 16 (3.0) | 0.01 |
| Major adverse cardiac events, n (%) | |||
| Cardiac death | 4 (0.7) | 8 (0.7) | 0.12 |
| Non-fatal AMI | 2 (0.4) | 5 (0.5) | 0.11 |
| Urgent revascularization | 5 (0.5) | 0.85 | |
TIMI=Thrombolys in Myocardial Infarction; AMI=acute myocardial infarction.
1,578 patients (94.5% of those eligible) had clinical follow-up, with a mean time of 3.2±2.5years, and with a minimum of four months and a maximum of 10.3years. The primary outcome occurred in 192 (13.9%) patients; 130 deaths occurred (90 of cardiac causes; 5.7%), 32 AMI (2.0%), and 70 TVR (4.4%). The estimated survival free of the primary outcome was 81.6% in six years.
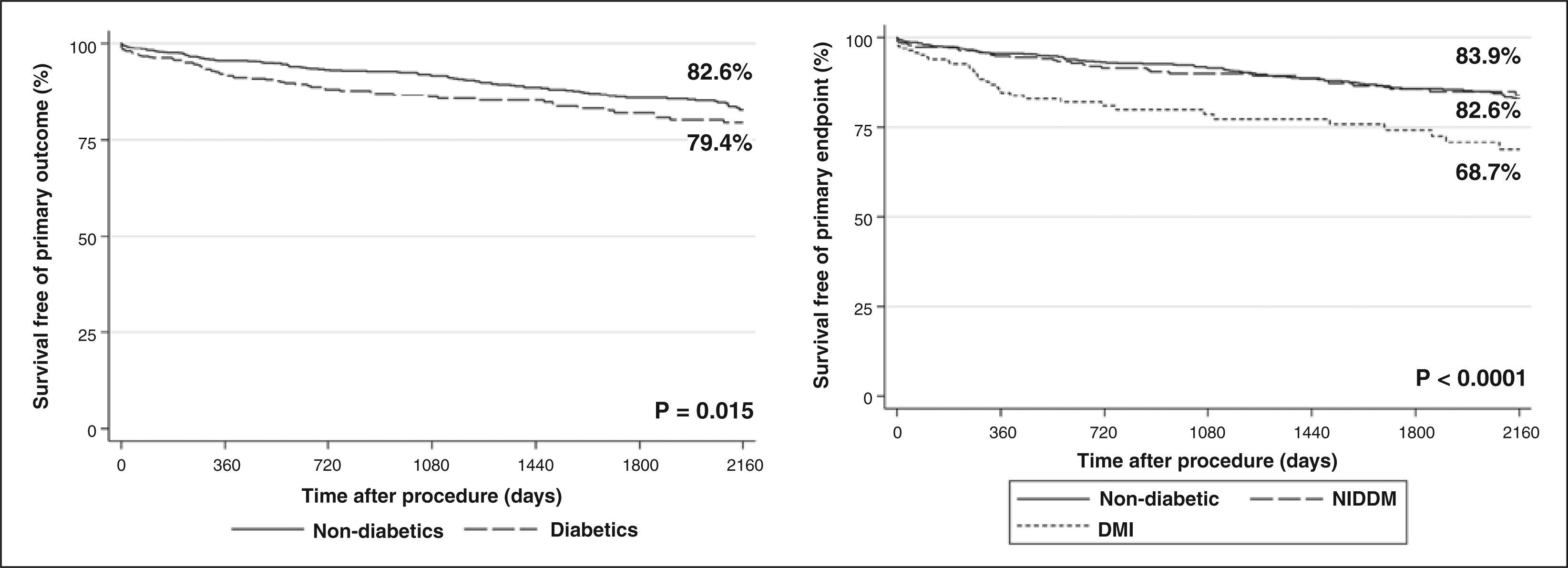
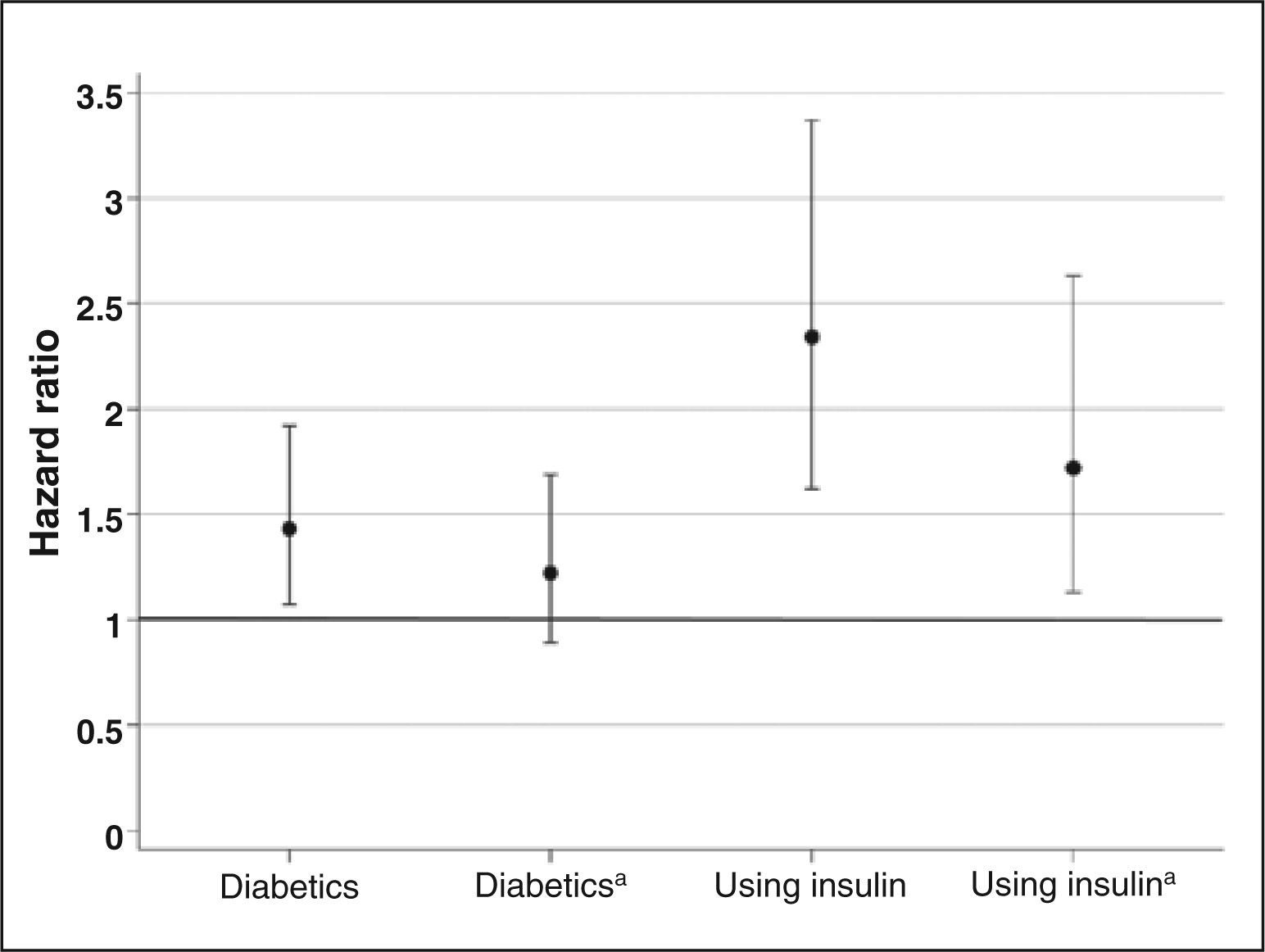
Diabetic patients had significantly lower survival free of events, compared to non-diabetic patients (79.4% vs. 82.6%; P=0.02) (Figure 2). RR was 1.43 (95% CI, 1.07 to 1.92) for events in diabetic patients (Figure 3). However, after adjusting for confounder variables, the adjusted RR was 1.22 (95% CI, 0.89 to 1.69), not statistically significant.
When comparing diabetics taking insulin, diabetics who were not taking insulin, and non-diabetics, the former showed survival free of events significantly lower than the other two groups, while diabetic patients who were not taking insulin showed similar behaviour to the non-diabetic ones (68.7% vs. 83.9% vs. 82.8%, respectively; P < 0.01). RR was 2.34 (95% CI, 1.62 to 3.37) for diabetics using insulin, compared to the other patients (Figure 3). The adjusted RR was 1.72 (95% CI, 1.13 to 2.63).
DISCUSSIONSAPPHIRE is the second published Brazilian registry evaluating the long-term follow-up of patients treated with DES. The DESIRE registry published its overall long-term results11 stratified by previous diabetes diagnosis. 12 In the latter study, major adverse cardiac events occurred in 9.8% of diabetic patients and in 7% of non-diabetics, at a mean follow-up of 2.5±1.4years (P=0.05). The observed differences in the incidence of events between the two registries are related to the different event definitions adopted, differences in clinical and angiographic profile of patients, and different follow-up times.
In the present study, diabetic patients who were not using insulin had late evolution similar to that of non-diabetic patients. The more favorable results of these less complex diabetic patients can be attributed to the use of DES. The SES-SMART trial, which compared the use of sirolimus-eluting stents versus bare-metal stents, showed lower restenosis in diabetic patients who were not using insulin (17% vs. 63%; P=0.01) – a benefit not observed in diabetic patients using insulin (40% vs. 64%; P=0.4).13
The comparison of conventional stents and DES in 440 unselected patients found a reduction of cardiac events in both groups of diabetic patients (with and without use of insulin), which was higher in the second group (1.9 times and 3.3 times, respectively).14
In another study involving 231 patients, late loss and binary restenosis were higher in diabetics using insulin, compared to non-diabetics, whereas there was no difference between the group who were not taking insulin and the non-diabetic group.15 At one year of follow-up, a mean increase in target vessel failure and a trend towards higher mortality in the group taking insulin were observed, compared to non-diabetics (P=0.06) – findings that were not present in the group that was not using insulin.
Diabetic patients have increased oxidative stress and inflammation, besides protein glycation; as a consequence, they develop more extensive atherosclerosis, coagulation disorders, and a greater number of vulnerable atherosclerotic plaques. Notably, patients using insulin also exhibit increased synthesis of plasminogen activation inhibitor-1 (PAI-1), which favors atherothrombotic events and inhibits the remodelling and proteolysis that occur after arterial injury, with consequent accumulation of extracellular matrix and neointimal hyperplasia, causing high rates of coronary restenosis.16
The SAPPHIRE registry shows rates of major adverse cardiac events consistent with other registries.12,17 According to the present results, it is concluded that the use of DES is of fundamental importance for the percutaneous treatment of coronary artery disease in diabetic patients, especially for those who do not use insulin, considering the reduction of risk of serious cardiac events to levels similar to those of non-diabetic patients.
CONCLUSIONSIn the present study, the use of DES was beneficial to all diabetics, especially those who did not use insulin.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.