Cardiogenic shock is a clinical condition of inadequate tissue perfusion due to cardiac dysfunction. The most common etiology is ST-segment elevation myocardial infarction (STEMI) leading to left ventricular failure, but it may also be caused by mechanical complications such as acute mitral regurgitation, ventricular septal rupture or rupture of the left ventricular free wall. Despite therapeutic advances, mortality rates remain high.
MethodsRetrospective, observational, single-center study, including consecutive patients admitted with a diagnosis of STEMI and cardiogenic shock treated by percutaneous coronary intervention (PCI) at a tertiary hospital specialized in cardiology. The primary objective was to evaluate in-hospital clinical outcomes.
ResultsA total of 78 patients were included, most of them were male (67.9%), mean age was 67.5 ± 13,4 years and 41.0% were diabetic. Primary PCI was performed in 46.2% of the patients, rescue PCI in 25.6% and elective PCI in 28.2% of the cases. The most frequently involved arteries were the left anterior descending artery and the right coronary artery, with 44.9% each. Intra-aortic balloon pump was used in 32.1% of cases and glycoprotein IIb/ IIIa inhibitors in 30.8% of the cases. The incidence of acute renal failure was 61.5%. The need for reintervention was observed in 9.0% and the rate of acute/subacute thrombosis was 3.8%. Death due to cardiogenic shock was observed in 46.2%.
ConclusionsCardiogenic shock remains a frequent and serious condition with almost 50% of in-hospital mortality despite the therapeutic advances.
Evolução Hospitalar de Pacientes com Choque Cardiogênico por InfartoAgudo do Miocárdio com Supradesnivelamento do Segmento ST
IntroduçãoO choque cardiogênico é uma condição clínica de inadequada perfusão tecidual devido à disfunção cardíaca. A etiologia mais comum é o infarto agudo do miocárdio com elevação do segmento ST (IMCSST) levando à insuficiência ventricular esquerda, mas também pode ser causado por complicações mecânicas, como insuficiência mitral aguda, ruptura do septo interventricular ou da parede livre do ventrículo esquerdo. Apesar dos avanços terapêuticos, a mortalidade continua elevada.
MétodosEstudo retrospectivo, observacional, unicêntrico, incluindo pacientes consecutivos internados com o diagnóstico de IMCSST e choque cardiogênico, tratados por intervenção coronária percutânea (ICP), em hospital terciário especializado em cardiologia. O objetivo primário foi avaliar os desfechos clínicos hospitalares.
ResultadosForam incluídos 78 pacientes, a maioria do sexo masculino (67,9%), com idade de 67,5 ± 13,4 anos e 41,0% diabéticos. ICP primária foi realizada em 46,2% dos pacientes, ICP de resgate em 25,6% e ICP eletiva em 28,2% dos casos. As artérias mais frequentemente acometidas foram a descendente anterior e a coronária direita, com 44,9% cada uma. O balão intra-aórtico foi utilizado em 32,1% e os inibidores da glicoproteína IIb/ IIIa em 30,8% dos casos. A incidência de insuficiência renal aguda foi de 61,5%. A necessidade de reintervenção ocorreu em 9,0%, e a taxa de trombose aguda/subaguda foi de 3,8%. Óbito, no choque cardiogênico, ocorreu em 46,2%.
ConclusõesO choque cardiogênico permanece uma entidade frequente e grave, com quase 50% de mortalidade hospitalar, apesar da evolução na terapêutica instituída atualmente.
Cardiogenic shock is a clinical condition of inadequate tissue perfusion due to cardiac dysfunction. Its definition includes the following hemodynamic parameters: persistent hypotension (systolic pressure < 80 to 90mmHg or mean blood pressure 30mmHg lower than mean baseline blood pressure), with a marked reduction in cardiac index (< 1.8 L/min perm², without hemodynamic support, or < 2.0 to 2.2 L/min perm² with hemodynamic support) and normal or elevated ventricular filling pressures. The most common etiology of cardiogenic shock isST-segment elevation myocardial infarction (STEMI), leading to left ventricular failure, but it can also be caused by mechanical complications, such as acute mitral regurgitation, or rupture of the interventricular septum or left ventricular free wall. However, any cause of severe acute ventricular dysfunction, either right or left, can lead to cardiogenic shock.1
The prevalence of cardiogenic shock appears to be decreasing since the mid-1970s. In a report from a metropolitan area in the United States (Worcester, Massachusetts), the incidence of cardiogenic shock was 7% between 1975 and 1990, decreasing to 5.5% to 6.0% since then.2 This improvement in the incidence of cardiogenic shock and associated mortality partly reflects the increasein the use of coronary reperfusion strategies, which, through correction of the infarct-related arterial patency, may limit the extentof the infarction.3−5
In this context, the mortality rates are still high, ranging in the most recent studies from 42% to 48%.2,6,7 Temporal analysis demonstrated a reduction in this outcome between the years 1995 and 2004 (60.3%vs. 47.9%; P < 0.001), mainly associated with the performance of early percutaneous coronary intervention (PCI), with the most evident benefit during the in-hospital period.2 This concept is important because, although studies have shown no differences between the mortality rates in relation to the chosen method of revascularization,8 in clinical practice more than 60% of patients admitted with STEMI and cardiogenic shock are treated by early PCI, with emergency coronary artery bypass graft (CABG) surgery performed in less than 5% of cases.
There have been few studies carried out in the Brazilian population admitted with STEMI, and the data related to cardiogenic shock were obtained from small subgroups.8−11 Thus, the present work aimed to evaluate the short-term hospital evolution and outcomes of these patients, treated in a tertiary hospital specialized in cardiology.
METHODSStudy PopulationThis study evaluated patients with STEMI who underwent PCI at Instituto do Coração do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Incor/HCFMUSP) in São Paulo, SP, Brazil, from January 2008 to March 2011. This study included all patients who developed cardiogenic shock during hospitalization and who were treated by PCI (primary, rescue, or elective).
Data collection and analysisThe in-hospital evolution data were collected by trained physicians, during the index hospitalization, following the completion of previously standardized forms. The data collected included clinical features, laboratory test results, percutaneous procedure data, and clinical outcome until hospital discharge.
DefinitionsSTEMI was diagnosed upon the occurrence of persistent ST elevation > 1mm in two contiguous leads or new left bundle branch block inthe electrocardiogram. Cardiogenic shock was defined by clinical criteria, according to the Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock (SHOCK) trial, considering the presence of hypotension (systolic blood pressure < 90mmHg for at least 30 minutes or requiring supportive measures to maintain systolic blood pressure > 90 mmHg) and organic hypoperfusion (urine output < 30 mL/minute and heart rate > 60bpm).8
Acute renal failure was considered as a 25% increase in baseline serum creatinine, or absolute increase of 0.5 mg/dL in serum creatinine between two and seven days after procedure completion.12 The evaluated vascular complications were pseudo aneurysm, arteriovenous fistula, hematoma at the access site (> 10 cm), distal embolization and/or ischaemia related to the puncture site, and bleeding at the access site, defined as a decrease in hemoglobin > 2 g/dL or one requiring transfusion. Death was defined as death from any cause.11
Continuous variables were represented as means and standard deviations, and categorical variables as absolute numbers and percentages.
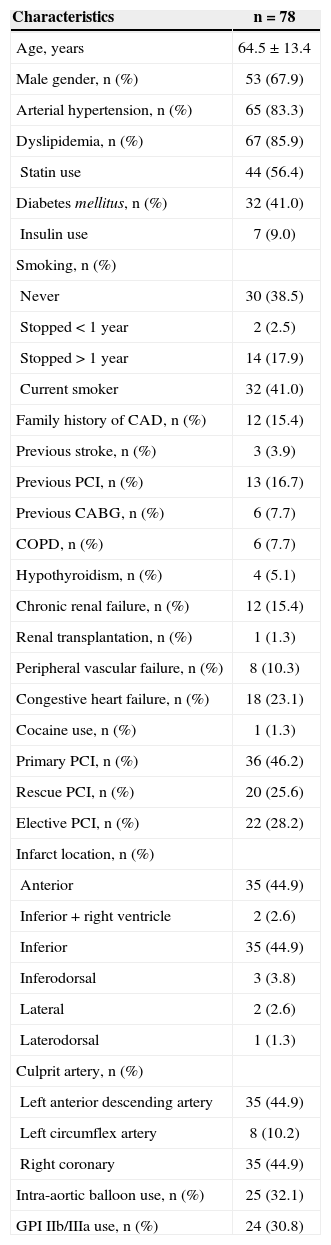
RESULTSOf a total of 513 patients diagnosed with STEMI, 78 (15.2 %) had cardiogenic shock. The clinical characteristics of the included patients are summarized in Table 1. The majority were male (67.9 %) with mean age of 67.5 ± 13.4 years. Diabetes was present in 41.0% of patients and 9% used insulin. Prior PCI had been performed in 16.7% of patients and 7.7% had undergone previous CABG. Chronic renal failure and peripheral vascular insufficiency were present in 15.4% and 10.3% of patients, respectively.
Clinical, angiographic and procedural characteristics
| Characteristics | n = 78 |
|---|---|
| Age, years | 64.5 ± 13.4 |
| Male gender, n (%) | 53 (67.9) |
| Arterial hypertension, n (%) | 65 (83.3) |
| Dyslipidemia, n (%) | 67 (85.9) |
| Statin use | 44 (56.4) |
| Diabetes mellitus, n (%) | 32 (41.0) |
| Insulin use | 7 (9.0) |
| Smoking, n (%) | |
| Never | 30 (38.5) |
| Stopped < 1 year | 2 (2.5) |
| Stopped > 1 year | 14 (17.9) |
| Current smoker | 32 (41.0) |
| Family history of CAD, n (%) | 12 (15.4) |
| Previous stroke, n (%) | 3 (3.9) |
| Previous PCI, n (%) | 13 (16.7) |
| Previous CABG, n (%) | 6 (7.7) |
| COPD, n (%) | 6 (7.7) |
| Hypothyroidism, n (%) | 4 (5.1) |
| Chronic renal failure, n (%) | 12 (15.4) |
| Renal transplantation, n (%) | 1 (1.3) |
| Peripheral vascular failure, n (%) | 8 (10.3) |
| Congestive heart failure, n (%) | 18 (23.1) |
| Cocaine use, n (%) | 1 (1.3) |
| Primary PCI, n (%) | 36 (46.2) |
| Rescue PCI, n (%) | 20 (25.6) |
| Elective PCI, n (%) | 22 (28.2) |
| Infarct location, n (%) | |
| Anterior | 35 (44.9) |
| Inferior + right ventricle | 2 (2.6) |
| Inferior | 35 (44.9) |
| Inferodorsal | 3 (3.8) |
| Lateral | 2 (2.6) |
| Laterodorsal | 1 (1.3) |
| Culprit artery, n (%) | |
| Left anterior descending artery | 35 (44.9) |
| Left circumflex artery | 8 (10.2) |
| Right coronary | 35 (44.9) |
| Intra-aortic balloon use, n (%) | 25 (32.1) |
| GPI IIb/IIIa use, n (%) | 24 (30.8) |
CAD = coronary artery disease; PCI = percutaneous coronary intervention; CABG = coronary-artery bypass grafting; COPD = chronic obstructive pulmonary disease; GPI = glycoprotein inhibitors.
Regarding the reperfusion therapy, 46.2% of patients underwent primary, 25.6% rescue, and 28.2% elective PCI. Left anterior descending artery and right coronary arteries were each the culprit arteries of STEMI in 44.9% of patients. The intra-aortic balloon was used in 32.1% of cases, and glycoprotein IIb/IIIa inhibitors in 30.8% of cases.
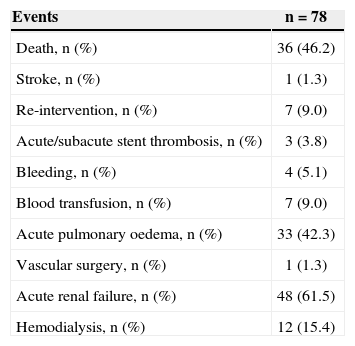
Clinical outcomes and in-hospital complications are shown in Table 2. The main complication associated with cardiogenic shock was the development of acute renal failure, which occurred in 61.5% of cases. The need for re-intervention occurred in 9.0% of the cases and the rate of acute/subacute thrombosis was 3.8%. The death rate from cardiogenic shock was 46.2%.
Clinical outcomes and in-hospital complications
| Events | n = 78 |
|---|---|
| Death, n (%) | 36 (46.2) |
| Stroke, n (%) | 1 (1.3) |
| Re-intervention, n (%) | 7 (9.0) |
| Acute/subacute stent thrombosis, n (%) | 3 (3.8) |
| Bleeding, n (%) | 4 (5.1) |
| Blood transfusion, n (%) | 7 (9.0) |
| Acute pulmonary oedema, n (%) | 33 (42.3) |
| Vascular surgery, n (%) | 1 (1.3) |
| Acute renal failure, n (%) | 48 (61.5) |
| Hemodialysis, n (%) | 12 (15.4) |
Cardiogenic shock is the leading cause of deat for patients admitted with STEMI and, despite treatment advances in recent years, including early revascularization through PCI or CABG, as well as the use of potent anticoagulant and antiplatelet agents, the mortality rateremain high.
Despite the high mortality rate observed in this study, it is very close to that reported in the literature described as between 42% and 65% of patients, especially when the intra-aortic balloon was indicate during PCI with established cardiogenic shock.13−15 In a sub-analysis of the American National Registry of Myocardial Infarction 2 (NRMI-2),16 the mortality rate from AMI complicated by cardiogenic shock, even in hospitals with extensive use of intra-aortic balloon, was 50.6%,versus 65.4% in hospitals with lower rate of use of this circulatory support device (P < 0.001).
The decrease of mortality in cardiogenic shock is related to achieving successful recanalization of the culprit vessel. In the SHOCK trial,8 a mortality rate of 39% was demonstrated in successfully treated cases, and a rate of 85% in cases thatdid not attain procedural success. All patients with TIMI flow 0 or 1 at the end of the intervention progressed to death. In the late six-year follow-up, the early reperfusion strategy showed a relative reduction in mortality of 67%, in comparison with the initial clinical compensation strategy.12 Another recent clinical trial, comparing mortality throughout 35 years of evolution of cardiogenic shock treatment, showed a significant reduction in mortality rates over-time (76% in 1980s, 65.6% in the 1990s, and 42% since 2000), which are similar values to those found in this study’s population.17
Study limitationsAmong the limitations of the present study are its observational design and lack of control group. The lack of appropriate time of ischaemia assessment is also highlighted. This was due to the fact that many patients were transferred directly from other peripheral healthcare network services to undergo PCI, which limited the appropriate evaluation of the pain-to-door and door-to-balloon time, once the data were obtained from medical records and, in many cases, this information was not obtained. These pain-to-door and door-to-balloon time variables could provide further information, as both were significantly correlated with the mortality rate in the literature.8,18,19
CONCLUSIONSCardiogenic shock remains a frequent and severe entity, with mortality rates of approximately 50% despite the currently established therapy. Therefore, it is observed that the best strategy would be the prevention of acute coronary events and, when they occur, early myocardial reperfusion measures should be attempted to prevent circulatory collapse and its unfavorable consequences.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.