Radial artery occlusion (RAO) is a clinically silent complication of transradial catheterization but may predispose to hand ischemia. Factors associated with this complication are the diameter of catheters and sheaths, the dose of heparin, repeated transradial procedures and the type of compressive dressing applied. The objective of this study was to evaluate if there is an association between reused hydrophilic vascular introducers and RAO.
MethodsPatients undergoing transradial catheterization were randomized to receive brand new introducers (Group I – GI) or reprocessed introducers (Group II – GII). The presence of RAO was evaluated at 24 hours (early) and day 30 (late) with the reverse Barbeau test.
ResultsTwo hundred and twenty-eight patients were assigned to GI (n=100) and GII (n=128). Mean age was 60.1±10.6years vs. 59.4±10.9years (P=0.64), 49% vs. 35.2% (P=0.03) were female and 25% vs. 27.3% (P=0.70) were diabetic. An total early RAO incidence of 10.5% and a late RAO incidence of 9.1% were observed. Ten GI patients (10%) had early RAO when compared to 14 (19.9%) in GII (χ2=0.05; HR: 1.09; P=0.82). On the 30-day follow-up RAO was observed in 6 GI patients (7.5%) when compared to 11 GII patients (10.4%) (χ2=0.45; HR=1.38; P=0.50).
ConclusionsIn our study no association was found between reused vascular introducers and early and late RAO in patients undergoing cardiac catheterization.
Interferência de Introdutores Reprocessados na Oclusãoda Artéria Radial após Cateterismo Cardíaco
IntroduçãoA oclusão da artéria radial (OAR) é uma complicação clinicamente silenciosa do cateterismo transradial, mas pode predispor à isquemia da mão. Fatores associados a essa complicação conhecidos são o calibre dos introdutores e cateteres, a dose de heparina utilizada, o número de reutilizações da artéria radial e o tipo de curativo compressivo aplicado. O objetivo deste estudo foi avaliar se existe associação entre a utilização de introdutores vasculares hidrofílicos reprocessados e a OAR.
MétodosPacientes submetidos a cateterismo transradial foram randomizados para introdutores novos (Grupo I – GI) ou reprocessados (Grupo II – GII). A presença de OAR foi avaliada em 24 horas (precoce) e 30 dias (tardia), por meio do teste de Barbeau reverso.
ResultadosForam alocados 228 pacientes no GI (n=100) e no GII (n=128). A idade foi de 60,1±10,6 anos vs. 59,4±10,9 anos (P=0,64), 49% vs. 35,2% (P=0,03) eram do sexo feminino e 25% vs. 27,3% (P=0,70) eram diabéticos. Observaram-se incidências totais de OAR precoce de 10,5% e de 9,1% para OAR tardia. Dez pacientes do GI (10%) apresentaram OAR precoce, comparados a 14 (10,9%) do GII (χ2=0,05; RR=1,09; P=0,82). Na avaliação de 30 dias, foi encontrada OAR em 6 pacientes do GI (7,5%) comparados a 11 pacientes (10,4%) do GII (χ2=0,45; RR=1,38; P=0,50).
ConclusõesNa casuística estudada, não foi encontrada associação entre a reutilização de introdutores vasculares e a OAR precoce e tardia em pacientes submetidos a cateterismo cardíaco.
The transradial approach in interventional cardiology has been popularized in recent years due to reduced rates of vascular complications of the access route and bleeding.1−3 This technique was described for the first time in Canada in 1989, for coronary angiography,4 and was described for angioplasty in the Netherlands in 1995.5 Regardless of the access route used, the incidence of complications related to the procedure is associated with the surgeon’s experience.6 The transradial technique requires a longer learning curve than the femoral access.7
Radial artery occlusion (RAO) is a complication that may predispose patients to ischemia of the hand. The incidence of RAO can reach 50% after prolonged catheterization of the artery in intensive therapy units.8, 9 Percutaneous coronary procedures have lower incidences. A study showed an incidence of RAO after catheterization of 5% when clinically diagnosed, and of 9% when diagnosed by duplex ultrasound.10 Multiple catheterizations of the radial artery,11 lower doses of heparin (2,000 U vs. 5,000 U),12 and larger diameter sheaths (6F vs. 5F)13 predispose to higher rates of occlusion.
In Brazil, the reprocessing of hemodynamic materials is a common practice, mainly due to economic reasons.14 This practice is regulated by the Brazilian Health Surveillance Agency (Agência Nacional de Vigilância Sanitária – ANVISA) by Resolution No. 2606, from August 11, 2006.15 This resolution lists medical products whose reprocessing is prohibited according to the current state of knowledge. Unlisted disposable products can be reused, such as vascular sheaths used in cardiac catheterization. There is no reference in the resolution regarding the acceptable number of reprocessing procedures. The use of reprocessed sheaths can cause microstructural physical changes, most evident after the fifth reuse.16 Removing the hydrophilic cover post-processing can increase friction with the intimal layer and expose sub endothelial elements, which predisposes to thrombosis.
This study was designed to determine whether there is an association between vascular sheath reuse and RAO incidence.
METHODSSampleThis was a prospective, cohort, randomized trial. Consecutive patients undergoing coronary angiography and/or transradial coronary angioplasty, in the hospitals Memorial Petrolina, in Petrolina, PE, Brazil, and Pro-Matre, in Juazeiro, BA, Brazil, from November 2010 to July 2011 were included in the study. All patients were submitted to tests to evaluate dual hand circulation before radial artery puncture in order to confirm the patency of the palmar artery arches. Patients who had been previously submitted to heart catheterization through the radial route and those incapable of returning for follow-up were not included. Patients were allocated into two groups by simple randomization, according to the year of birth. Group I (GI) was comprised by patients born in even numbered years, in whom new vascular sheaths were used, and Group II (GII) was comprised by patients born in odd numbered years, in whom reprocessed introducers were used. The maximum allowed number of reprocessing procedures was four. All sheaths were 6F Glide sheath® models, and manufactured by Terumo® (Terumo Interventional Systems – Tokyo, Japan). Sheaths lengths of 10cm, 16cm, and 25cm were used, and sheaths were considered long when length≥16cm. Patients were evaluated for the presence of RAO 24 hours after surgery (early occlusion) and 30 days after the procedure (late occlusion). All patients signed an informed consent. The study was approved by the research ethics committee of the Health Sciences Center of Universidade Federal de Pernambuco, CEP/CCS/UFPE protocol number 306/10.
Evaluation of dual hand circulationThe patients were submitted to Allen and Barbeau tests. In the Allen test, the patient is asked to make a fist. The examiner compresses the radial and ulnar arteries simultaneously. The patient is instructed to open the hand. The ulnar artery is then released, and the time required for palmar perfusion to return is noted. The test is considered normal when perfusion returns in 5 to 10 seconds, which indicates adequate collateral circulation. The Barbeau test was developed using plethysmography and pulse oximetry to improve the sensitivity of Allen test. In this protocol, a pulse oximeter is placed on the thumb and the ipsilateral radial artery is occluded (Figure 1). Constant oximetry values indicate uninterrupted artery filling during the radial occlusion.
Transradial catheterization techniquePatients with appropriate collateral hand circulation underwent radial artery puncture and a standard spasmolytic cocktail was injected through the sheath, containing 5,000 U of heparin, 10mg of isosorbide mononitrate and 1mL of lidocaine 2%. Patients undergoing percutaneous coronary intervention received additional doses of heparin, ranging from 2,500 to 5,000 U, depending on the procedure duration. At the end of the intervention, the sheath was promptly removed, and a standard compressive dressing was used,17 consisting of a wad of gauze and tape. The dressing was applied to the puncture site and secured with three strips of surgical tape, so that the radial artery was compressed, while maintaining the ulnar artery flow intact. The protocol of the services where the study was performed recommended compression for 120 minutes, which may be longer in case of persistent bleeding. All procedures were performedby the same surgeon with experience of more than 3,000 cases of transradial catheterization.
Sheath reprocessingAfter removal, all sheaths were washed with water and detergent, and sent for sterilization with ethylene oxide. The number of reprocessing procedures was controlled by means of coloured stickers placed on the sheath, with each colour corresponding to a number.
RAO AssessmentPatients were submitted to radial artery assessment within 24 hours and after 30 days using the reverse Barbeau test. In it, the oximeter was placed on the thumb and the ulnar artery was compressed. The maintenance of the oximetry values indicated radial artery patency, and its disappearance indicated the artery occlusion.
Data AnalysisSample size calculation was performed using the Stat Calc platform of Epi-Info® (Center is for Disease Control [CDC] – Atlanta, United States). Considering the expected incidence of 12% of late occlusion in GII and 2% in GI, the sample size would have 198 patients (99 in each group). Data were tabulated in Microsoft Excel® software spread sheets. Categorical variables were compared by chi-squared and Fisher’s exact tests. Continuous variables were compared by Student’s t-test. Relative risk (RR) was used as association measure, considering GII as the reference group P-value≤0.05 was considered statistically significant Variables considered to be confounders were submitted to univariate analysis within the control group (GI )When an association was found with the outcomes, the imputed variable would be included in a multivariate analysis. Statistical calculations were performed with Epi-Info® and its Stat Calc platform.
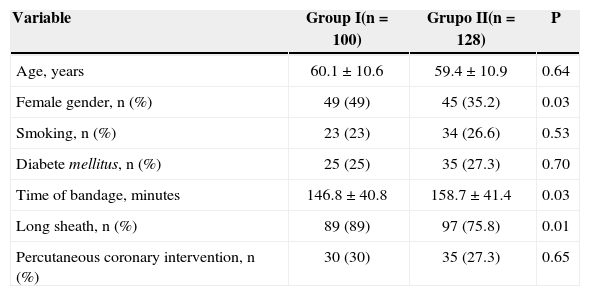
RESULTSPatients’ characteristicsA total of 228 patients were evaluated, allocated in GI (n=100) and GII (n=128). The mean age was 60.1±10.6years vs. 59.4±10.9years (P=0.64), 49 vs. 35.2% (P=0.03) were females, and approximately one-quarter of the patients (25% vs. 27.3%; P=0.7 were diabetic, for GI and GII, respectively. Percutaneous coronary intervention was performed in 30% vs. 27.3 cases (P=0.65). The time of compressive dressing us (146.8±40.8minutes vs. 158.7±41.4minutes; P 0.03) and the use of long sheaths (89% vs.75.8%; = 0.01) were greater in GII.
Of all the included patients, 186 (81.6%) were submitted to reverse Barbeau test after 30 days. Two patients in GI and one patient in GII died before the late assessment, and 39 patients did not undergo late assessment, as they were not located.
RAO incidenceIn the study, overall early RAO incidence was 10.5% (24/228 patients), and 9.1% for late RAO (17/186 patients). Ten GI patients (10%) had RAO at the 24-hour assessment, compared with 14 (10.9%) in GII (χ2=0.05; RR=1.09; P=0.82). At the 30-day assessment, RAO was found in six patients from GI (7.5%) compared to 11 patients (10.4%) from GII (χ=0.45; RR=1.38; P=0.50).
Twenty-two patients who had early RAO were re-evaluated at 30 days. It was observed that, of these, 17 (77.3%) had spontaneous artery recanalization. Of the 204 patients with patent radial arteries at the 24-houassessment, 164 were reassessed at 30 days and only ten (6.1%) showed delayed occlusion.
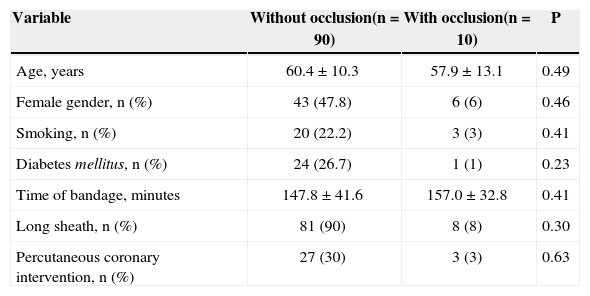
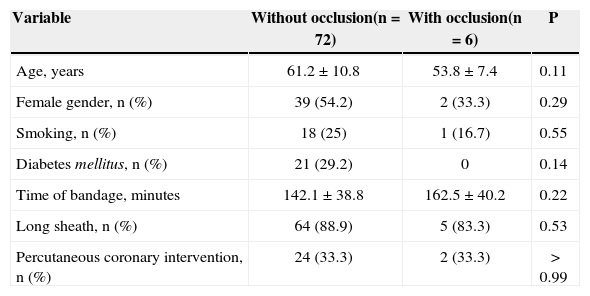
Univariate analysisDemographic characteristics and those related to the procedure shown in Table 1 were considered at potential confounders. The results of the univariate analysis performed with these variables are shown in Tables 2 and 3. This analysis was performed only in GI (new sheaths) to prevent interference with the study variable (reuse of sheaths).
Demographic and procedural profile
| Variable | Group I(n=100) | Grupo II(n=128) | P |
|---|---|---|---|
| Age, years | 60.1±10.6 | 59.4±10.9 | 0.64 |
| Female gender, n (%) | 49 (49) | 45 (35.2) | 0.03 |
| Smoking, n (%) | 23 (23) | 34 (26.6) | 0.53 |
| Diabete mellitus, n (%) | 25 (25) | 35 (27.3) | 0.70 |
| Time of bandage, minutes | 146.8±40.8 | 158.7±41.4 | 0.03 |
| Long sheath, n (%) | 89 (89) | 97 (75.8) | 0.01 |
| Percutaneous coronary intervention, n (%) | 30 (30) | 35 (27.3) | 0.65 |
Results of univariate analysis between patients with and without early radial artery occlusion in Group I
| Variable | Without occlusion(n=90) | With occlusion(n=10) | P |
|---|---|---|---|
| Age, years | 60.4±10.3 | 57.9±13.1 | 0.49 |
| Female gender, n (%) | 43 (47.8) | 6 (6) | 0.46 |
| Smoking, n (%) | 20 (22.2) | 3 (3) | 0.41 |
| Diabetes mellitus, n (%) | 24 (26.7) | 1 (1) | 0.23 |
| Time of bandage, minutes | 147.8±41.6 | 157.0±32.8 | 0.41 |
| Long sheath, n (%) | 81 (90) | 8 (8) | 0.30 |
| Percutaneous coronary intervention, n (%) | 27 (30) | 3 (3) | 0.63 |
Results of the univariate analysis between patients with and without late radial artery occlusion in Group I
| Variable | Without occlusion(n=72) | With occlusion(n=6) | P |
|---|---|---|---|
| Age, years | 61.2±10.8 | 53.8±7.4 | 0.11 |
| Female gender, n (%) | 39 (54.2) | 2 (33.3) | 0.29 |
| Smoking, n (%) | 18 (25) | 1 (16.7) | 0.55 |
| Diabetes mellitus, n (%) | 21 (29.2) | 0 | 0.14 |
| Time of bandage, minutes | 142.1±38.8 | 162.5±40.2 | 0.22 |
| Long sheath, n (%) | 64 (88.9) | 5 (83.3) | 0.53 |
| Percutaneous coronary intervention, n (%) | 24 (33.3) | 2 (33.3) | > 0.99 |
There were no statistically significant associations between these variables and the early (Table 2) and late occlusion (Table 3) of the radial artery.
DISCUSSIONTransradial access for left heart catheterization, angiography, and coronary angioplasty has a lower incidence of bleeding and vascular complications when compared to femoral access. One of these complications is the post-procedure RAO, which despite being generally silent, may predispose to ischemia of the hand. The incidence of post-catheterization RAO in the literature is variable, reaching around 10% in most recent studies.18
Individuals with RAO may present palpable pulse due to collateral circulation. For this reason, the mere presence of pulse does not indicate a patent radial artery. An effective test should be used, preferably, to determine the presence or absence of arterial occlusion. The Barbeau test is simple to perform and shows high correlation with Doppler, which is the gold standard for detecting arterial occlusion.18
The way that the compressive dressing is applied post-procedure is associated with RAO. Dressings that completely interrupt arterial flow are associated with arterial occlusion. A study comparing patients who had the artery totally occluded by the dressing, compared to those that maintained the blood flow during compressive procedures showed an almost seven-fold greater chance of occlusion in the first group. This study additionally demonstrated that these arteries undergo spontaneous recanalization, remaining occluded in only about 10% of cases when evaluated one week later.19 When compared with an occlusive dressing, a bracelet that allowed the flow during compression of the artery reduced the incidence of RAO by up to 59%.18 The dose of heparin appears to have an inverse correlation with occlusion rate.12 In the present study, the same occlusive compressive dressing was used for all patients, and the dose of heparin was at least 5,000 U.
This study did not demonstrate as significant association between reuse of vascular sheaths and early and late RAO. Regarding the late occlusion, a RR of 1.38 was obtained, which could suggest an association, but without statistical significance. Those data suggest that the practice of reprocessing vascular sheaths for cardiac catheterization is safe. Further studies with larger samples are needed to confirm these findings. In this study, the number of reprocessing procedures was not taken into account, considering only that this number was between one and four times, demonstrating that intravascular devices only show significant structural micro changes after the fifth reutilization.15 The goal was to observe the events in a real-life situation, where sheaths are used after a variable number of reprocessing procedures. The fact that the GII patients had longer duration compressive dressings may suggest that sheath reutilization increases the time of bleeding after procedures, but this hypothesis was not tested.
In this study, it was observed that some patients showing patent radial artery at the 24-hour assessment later demonstrated arterial occlusion, and other patients with early occlusion showed late arterial recanalization. Of the 186 patients assessed both early and late in this study, it was observed that in the 22 that had early occlusion, 17 (77.3%) showed later patent radial artery. Of 164 patients that had patent arteries at 24 hours, 154 (93.9%) remained with patent arteries at the 30-day assessment. This demonstrates that most of the early-occluded radial arteries indeed show later recanalization. Isolated late occlusion was an unusual event in the present study (6.1%).
This study does not intend to support the reprocessing of introducers, but these data can be used to demonstrate the safety of this practice regarding post-procedural vascular occlusion. It is suggested, however, that the number of reuses does not exceed four times, as there are no data about RAO incidence in this scenario.
Study limitationsThe following were not obtained: measures of radial artery diameter (and the sheath diameter/artery diameter ratio), assessment of antegrade flow during hemostasis, and total dose of administered heparin – known factors to be associated with RAO. The impossibility to assess the late radial artery patency in 18.4% of the study population was a limitation, which may have reduced the study power to assess this outcome. The association between the number of reprocessing procedures and the incidence of RAO was not analyzed, and it cannot be inferred whether the greater number of reuses is associated with higher incidence of RAO. Finally, the data from this research cannot be extrapolated to non-hydrophilic vascular sheaths, or to other calibres or those from other manufacturers.
CONCLUSIONSThe reuse of hydrophilic vascular sheaths is not associated with radial artery occlusion in patients undergoing transradial cardiac catheterization. The incidence of early and late RAO post-left cardiac catheterization in this study was low and comparable with that found in the literature. Most patients with early radial artery occlusion showed late arterial recanalisation. Isolated late occlusion was a rare event with low frequency.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.
To the hemodynamic teams of Memorial Petrolina and Juazeiro Pró-Matre hospitals, particularly to radiology technicians Nilton Galdino and Giovanny Jorge; nurses Patricia Garcia and Magnum Danilo; and nursing technicians Carolina, Isakella and Anny, and Luiz Antonio Vasconcelos.