Type C coronary lesions represent a complex angiographic scenario, although it is a rather common one in the daily clinical practice of percutaneous coronary intervention (PCI). Our objective was to report the national clinical practice outcomes of PCIs performed in patients with type C lesions.
METHODSRetrospective study, with information obtained from the electronic database of the National Center of Cardiovascular Interventions (Central Nacional de Intervenções Cardiovasculares – CENIC) of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista (SBHCI) which gathers information on PCI procedures in a dedicated database, entered by volunteer physicians members of different Brazilian institutions.
RESULTSBetween January 2010 and December 2011 1,693 patients with type C lesions were registered in CENIC. Most patients were male (68%), with mean age of 63±26.3years, 40.9% were diabetic and 45.4% had acute coronary syndromes. Procedure success was achieved in 95.6% of the cases, mortality was 2.1%, acute myocardial infarction was observed in 5% and target-lesion revascularization in 0.5% of the patients during hospitalization.
CONCLUSIONSPCIs in type C lesions had high success and low complication rates in a selected population group of the CENIC registry. The former morphological classification of the lesions, still adopted in the registry, does not properly stratify the outcomes of PCI currently. Updating the data collection form and measures to improve the quality control of the registry are urgently needed.
Resultados Hospitalares das Intervenções CoronáriasPercutâneas em Lesões Tipo C: Registro CENIC
IntroduçãoLesões coronárias tipo C representam um cenário angiográfico complexo embora bastante comum na prática clínica diária da intervenção coronária percutânea (ICP). Nosso objetivo foi apresentar os resultados da prática clínica nacional das ICPs realizadas em pacientes com lesões tipo C.
MétodosEstudo retrospectivo, com informações obtidas a partir dos dados inseridos no registro eletrônico da Central Nacional de Intervenções Cardiovasculares (CENIC) da Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista (SBHCI), e que agrega informações sobre procedimentos das ICPs reunidos em um banco de dados dedicado, com preenchimento voluntário por médicos associados de várias instituições brasileiras.
ResultadosEntre janeiro de 2010 e dezembro de 2011, foram incluídos 1.693 pacientes com lesões tipo C devidamente cadastrados na CENIC. Predominaram pacientes do sexo masculino (68%), com média de idade de 63 ± 26,3 anos, 40,9% eram diabéticos e 45,4% apresentaram quadros clínicos instáveis. Sucesso do procedimento foi alcançado em 95,6% dos casos, a mortalidade foi de 2,1%, infarto agudo do miocárdio ocorreu em 5% e revascularização da lesão-alvo ocorreu em 0,5% dos pacientes na fase hospitalar.
ConclusõesAs ICPs em lesões tipo C do registro CENIC apresentaram altas taxas de sucesso e baixas taxas de complicação, numa amostra da população relativamente selecionada. A antiga classificação morfológica das lesões, ainda adotada no registro, não estratifica adequadamente os resultados da ICP na era contemporânea. A atualização da ficha de coleta dos dados e medidas que intensifiquem o controle de qualidade do registro são urgentes e necessárias.
Coronary artery disease has a fairly heterogeneous aspect; the anatomically more complex lesions remain a challenge for percutaneous coronary intervention (PCI). In the pre-stent era, a greater discrepancy, with lower success rates and a greater number of complications, was observed in procedure results of these lesions when compared to less complex lesions.1 In 1988, the classification of coronary lesions by severity was created, estimating the success and complication rates during balloon PCI.2 With the advent of stents, there was a greater preponderance of immediate results after the procedure, with lower rates of acute occlusion, 3–7 especially in more complex anatomic lesions. As a consequence of better results and new techniques, the need to reformulate this classification arose as did the need for new definitions, reflecting the experience acquired in procedures of greater complexity.8
The aim of the present study was to analyse the profile and contemporary in-hospital results of patients undergoing PCI of type C lesions recorded in the database of the Central Nacional de Intervenções Cardiovasculares (National Cardiovascular Intervention Centre – CENIC) between 2010 and 2011.
METHODSThis was a retrospective study with information obtained from the CENIC electronic record, created in 1991 by the Sociedade Brasileira de Hemodinâmica e Cardiologia Intensiva (Brazilian Society of Haemodynamics and Interventional Cardiology – SBHCI), which archives information on PCI in a dedicated database voluntarily recorded by associated physicians from several Brazilian institutions.
For this study, all procedures involving type C lesions recorded between January, 2010 and December, 2011 were included. The definition of type C lesion was established from an American guideline, designating lesions as having a high risk of complications if they present at least one of the following characteristics: length of lesion > 20mm; excessive tortuosity of the proximal segment; target segment with extreme angulation (> 90 degrees); chronic occlusion (> three months); inability to protect larger lateral branches; or degenerated venous grafts. The data collected and used in this study were related to clinical, angiographic, and procedural characteristics, including in-hospital complications. Procedural success or failure definitions and in-hospital complications (death, acute myocardial infarction, stroke, and target-vessel revascularisation) included those commonly used by clinicians when completed the forms related to each procedure in the CENIC database.
Continuous variables were expressed as mean±standard deviation, while categorical variables were expressed as absolute numbers and percentages.
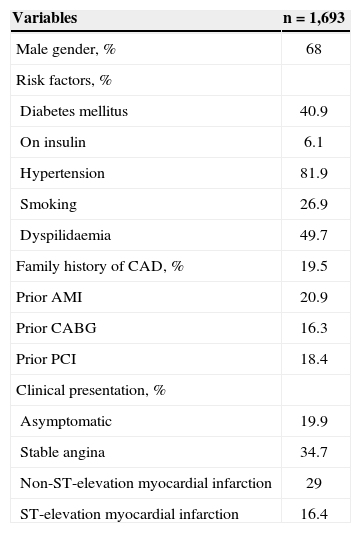
RESULTSIn this study, 1,693 patients from the CENIC electronic address (www.sbhci.org.br) for the previously mentioned study period were evaluated. Table 1 presents the clinical characteristics of the patients. Most patients were male (68%), with a mean age of 63±26.3years. High clinical complexity with an elevated incidence of diabetes (40.9%), prior acute myocardial infarction (20.9%), and prior revascularisation procedures, whether surgical (16.3%) or percutaneous (18.4%), were observed.
Clinical Characteristics
| Variables | n=1,693 |
|---|---|
| Male gender, % | 68 |
| Risk factors, % | |
| Diabetes mellitus | 40.9 |
| On insulin | 6.1 |
| Hypertension | 81.9 |
| Smoking | 26.9 |
| Dyspilidaemia | 49.7 |
| Family history of CAD, % | 19.5 |
| Prior AMI | 20.9 |
| Prior CABG | 16.3 |
| Prior PCI | 18.4 |
| Clinical presentation, % | |
| Asymptomatic | 19.9 |
| Stable angina | 34.7 |
| Non-ST-elevation myocardial infarction | 29 |
| ST-elevation myocardial infarction | 16.4 |
AMI=acute myocardial infarction, CAD=coronary artery disease; n=number of patients; PCI=percutaneous coronary intervention; CABG=coronary artery bypass graft.
Regarding the reason for the intervention, 54.6% were stable; of these, 34.7% had stable angina, and 19.9% were asymptomatic. ST-elevation myocardial infarction was observed in 16.4% of patients, and acute coronary syndrome without ST-elevation was observed in 29%. In this last subgroup, risk stratification according to the TIMI score evidenced that a majority of patients (57.3%) were classified as high risk, 24.5% as moderate risk, and 18.2% as low risk.
In patients with ST-elevation myocardial infarc-tion, 77.1% were classified as Killip I, 11.8% as Killip II, and 4.5% as Killip III. In addition, 6.6% were in cardiogenic shock. Primary angioplasty was performed in 69.1% of patients, with a door-to-balloon time of 65±110 minutes. Elective angioplasty in the same subgroup was performed in 19.8% of patients, with a mean delay for the procedure of 16±11 days. Rescue angioplasty was performed in 10.8% of the cases, with facilitated angioplasty in only 0.3% of patients. The mean in-hospital length of stay was 2.5±5 days.
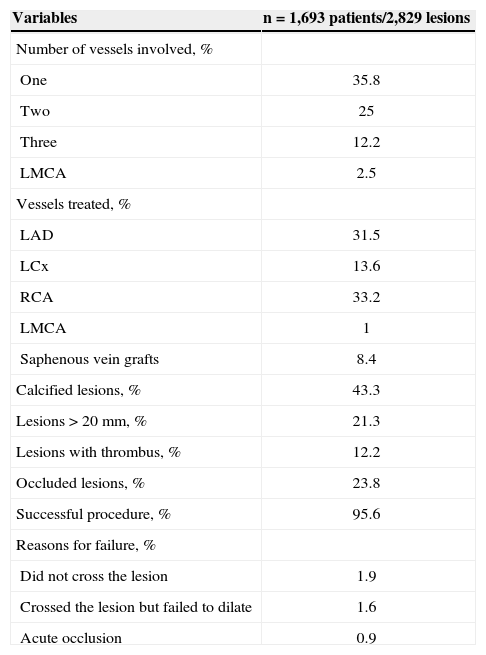
The femoral approach was used in 95.6% of cases, and the radial approach was used for the remainder (14.7%). Angiographic characteristics observed in this population demonstrated a predominance of patients with one vessel disease (35.8%), and the vessels treated most often included the right coronary artery (33.2%) and left anterior descending artery (31.5%). Among the morphologic findings of type C lesions, calcification and length > 20mm were most often reported, with an incidence of 43.3% and 21.3%, respectively. The mean stenosis of the lesions was 87.1±13.2%.
Procedural success was observed in 95.6% of the patients. Reasons for procedural failure included inability to cross the lesion (1.9%), crossing the lesion but without successful dilation (1.6%), and acute occlusion (0.9%).
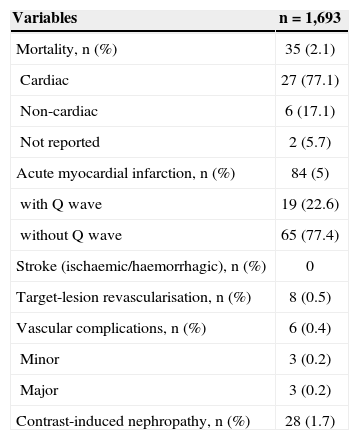
Table 3 presents the in-hospital clinical results. All-cause mortality was 2.1%, of whom 77.1% were due to cardiac causes. Acute myocardial infarction was observed in 5% of patients, of whom 77.4% did not show new Q waves on post-procedure electrocar-diograms. No episodes of ischaemic or haemorrhagic stroke were observed. Target-vessel acute or subacute occlusion was identified in 26 (1.53%) patients, of whom 18 (69.2%) were maintained on clinical treatment without mechanical intervention, seven (26.9%) returned to the cath laboratory to undergo repeat angioplasty, and one (3.85%) was referred for elective surgery. Major and minor vascular complications were observed in six (0.4%) patients, and 28 (1.7%) patients developed contrast-induced nephropathy.
Angiographic Characteristics of the Procedure
| Variables | n=1,693 patients/2,829 lesions |
|---|---|
| Number of vessels involved, % | |
| One | 35.8 |
| Two | 25 |
| Three | 12.2 |
| LMCA | 2.5 |
| Vessels treated, % | |
| LAD | 31.5 |
| LCx | 13.6 |
| RCA | 33.2 |
| LMCA | 1 |
| Saphenous vein grafts | 8.4 |
| Calcified lesions, % | 43.3 |
| Lesions>20mm, % | 21.3 |
| Lesions with thrombus, % | 12.2 |
| Occluded lesions, % | 23.8 |
| Successful procedure, % | 95.6 |
| Reasons for failure, % | |
| Did not cross the lesion | 1.9 |
| Crossed the lesion but failed to dilate | 1.6 |
| Acute occlusion | 0.9 |
LAD=left anterior descending artery; LCx=circumflex artery; LMCA=left main coronary artery; RCA=right coronary artery.
In-hospital Clinical Results
| Variables | n=1,693 |
|---|---|
| Mortality, n (%) | 35 (2.1) |
| Cardiac | 27 (77.1) |
| Non-cardiac | 6 (17.1) |
| Not reported | 2 (5.7) |
| Acute myocardial infarction, n (%) | 84 (5) |
| with Q wave | 19 (22.6) |
| without Q wave | 65 (77.4) |
| Stroke (ischaemic/haemorrhagic), n (%) | 0 |
| Target-lesion revascularisation, n (%) | 8 (0.5) |
| Vascular complications, n (%) | 6 (0.4) |
| Minor | 3 (0.2) |
| Major | 3 (0.2) |
| Contrast-induced nephropathy, n (%) | 28 (1.7) |
n=number of patients.
The classification of angiographic lesions was established in 1988 by a committee of the American College of Cardiology (ACC) and the American Heart Association (AHA), and was immediately validated by several studies.2–9 The objective of this classification was to stratify angiographic lesions according to their complexity and, thereby, estimate the success and risk of complications from angioplasties.
Initially, the division of lesions into type A (low complication rate and success > 85%), type B (moderate complication risk and success between 60% and 85%), and type C (high complication risk and success < 60%) was proposed. Subsequently, Ellis et al.1 recommended that type B lesions should be subdivided if they presented one (B1) or more (B2) severity criteria.
Notably, the first classification was based on results of procedures performed almost exclusively with balloon-catheters, which have greater complication and failure rates. With the technological evolution of the materials used in the procedures, in addition to the expressive collaboration of adjunct pharmacology, this classification needs to be re-evaluated.
Wilensky et al.10 analysed 2,839 patients in the National Heart, Lung, and Blood Institute Dynamic Registry with complex lesions, defined as lesions with evidence of thrombus, calcification, bifurcation, or in the ostium; and they compared these patients with 1,720 patients who presented with non-complex lesions. Complex lesions were associated with higher rates of dissection, distal embolisation, obstruction of secondary branches, and persistent reduction in coronary flow. Patients with complex lesions had a lower rate of success (93.8% vs. 97.3%; P < 0.001) and a greater rate of in hospital death (2% vs. 0.6%; P < 0.001), death/acute myocardial infarction (5.2% vs. 2.4%), and death/myocardial infarction/coronary artery bypass graft surgery (6.5% vs. 2.9%).
Despite the limitations of the present study, which include underreporting of cases and missing data due to voluntary contributions, it is clear that the old classification of A, B1, B2, and C types, which is still used in the CENIC registry, does not adequately stratify the success and complication rates of the procedure.
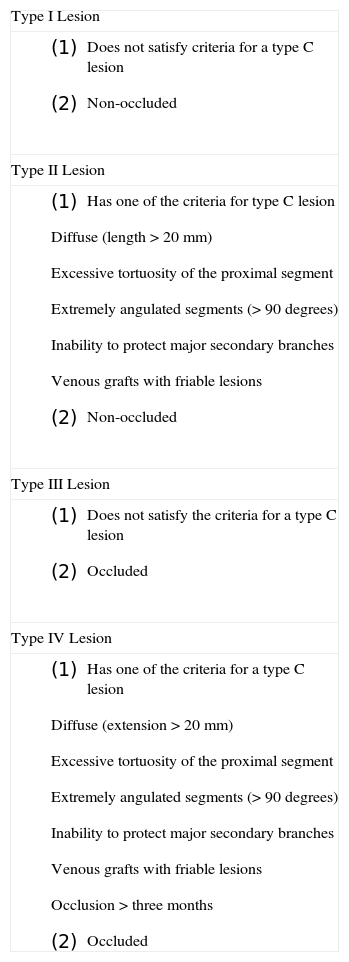
In fact, a new classification of lesions proposed by the Society for Cardiac Angiography and Intervention (SCAI), a simplified version of the 1988 ACC/ AHA classification (Table 4), has demonstrated greater discriminatory power for success and complications.11 This classification system requires only two discriminations (C/non-C lesion and occluded/non-occluded lesion) that can be reliably and reproducibly distinguished by experienced professionals.
Classification of Lesions According to SCAI11
| Type I Lesion |
|
| Type II Lesion |
|
| Type III Lesion |
|
| Type IV Lesion |
|
Thus, a reformulation of variables and their definitions used in the clinical and angiographic characterisation of patients and interventions, the inclusion of all procedures performed in a pre-specified period, an increase in the number of institutions to better reflect reality, and the collection of data are necessary measures to update the CENIC registry.
In a recent editorial, Mattos12 suggested that revitalisation measures should be applied to bring more strength to the registry, with periodic meetings of participating centres in order to maintain a united, active, and stimulated group. In addition, Mattos12 recommended independent monitoring of the data and increasing the centres of the collected data to encompass late patient follow-up.
CONCLUSIONSPCI of type C lesions, as categorised by the CENIC registry, presented high success rates and low complication rates in a relatively selective population. The old morphologic classification, still used by the registry, is no longer adequate for stratifying PCI results. Updating the data collection form and adopting measures that increase the quality control of the registry are urgent and necessary.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.