Early diagnosis and treatment of congenital heart defects have a well-known impact on patient´s quality of life. This study aimed to describe the population of patients with congenital heart disease submitted to percutaneous diagnostic or therapeutic procedures at a tertiary referral center.
MethodsRetrospective analysis of 1,002 patients submitted to cardiac catheterization between 2003 and 2009 at Instituto de Cardiologia do Rio Grande do Sul. Clinical, demographic and procedure variables were obtained from an institutional database and patient charts.
ResultsMedian age was 33 (0-73) years and median weight was 23 (9.6-52.6) kg. Patients were predominantly females (52%), with acyanotic heart disease (63.2%) and postnatal diagnosis (94.8%). Pulmonary stenosis (22.9%), atrial septal defect (22.5%) and patent ductus ateriosus (21.6%) were the most common acyanotic heart defects, whereas tetralogy of Fallot was the most frequent cyanotic heart disease (15,2%). Most of the procedures (58,6%) were therapeutic, including pulmonary balloon valvuloplasty (32.9%), atrial septal defect closure (20.9%) and ductus arteriosus closure (15%). Complications were observed in 19.2% of patients, and inguinal hematomas (7.8%) and fever (7.6%) were the most frequent findings. There were 3 procedure-related deaths (0.3%).
ConclusionsThe study results demonstrated the prevalence of therapeutic procedures in patients with acyanotic heart disease, performed with a low complication rate at a tertiary referral center.
Perfil de Pacientes com Cardiopatia Congênita Submetidosa Procedimentos Percutâneos em um Centro Terciário: Análise de 1.002 Casos
IntroduçãoO diagnóstico precoce e o tratamento dos defeitos cardíacos congênitos têm reconhecido impacto na qualidade de vida dos pacientes. Nosso objetivo foi descrever a população de pacientes com cardiopatias congênitas submetidos a procedimentos diagnósticos ou terapêuticos percutâneos em um centro terciário.
MétodosAnálise retrospectiva de 1.002 pacientes submetidos a cateterismo cardíaco no período de 2003 a 2009 no Instituto de Cardiologia do Rio Grande do Sul. Variáveis demográficas, clínicas e do procedimento foram obtidas a partir de um banco de dados institucional e dos prontuários dos pacientes.
ResultadosA mediana de idade dos pacientes foi de 33 (0-73) anos e a de peso, de 23 (9,6-52,6) kg. Houve predominância do sexo feminino (52%), de doença acianótica (63,2%) e de diagnóstico realizado no período pósnatal (94,8%). Estenose pulmonar (22,9%), comunicação interatrial (22,5%) e persistência do canal arterial (21,6%) foram os defeitos acianóticos mais comuns, e tetralogia de Fallot foi a doença cianótica mais frequente (15,2%). A maioria dos procedimentos (58,6%) foi terapêutica, incluindo valvuloplastias pulmonares (32,9%), fechamento de comunicações interatriais (20,9%) e fechamento de persistências do canal arterial (15%). Em 19,2% dos pacientes foram observadas complicações, sendo os hematomas inguinais (7,8%) ou a febre (7,6%) as mais frequentes. Ocorreram 3 óbitos (0,3%) relacionados aos procedimentos.
ConclusõesOs resultados deste estudo evidenciaram a predominância de procedimentos terapêuticos em pacientes com cardiopatias congênitas acianóticas, realizados com baixo índice de complicações, em centro terciário de referência.
Congenital heart defects affect approximately nine per 1,000 live births. 1,2 Approximately 20% to 30% of untreated children with heart disease die within the first month of life. 3 Early diagnosis is crucial to prevent and minimize the complications of rapid clinical deterioration and to reduce the high rates of morbidity and mortality. 4
Interventional cardiology offers diagnostic procedures in cases where traditional assessment methods are inadequate, and in cases in which manometric evaluation is critical. Furthermore, therapeutic percutaneous procedures postpone or even prevent the need to perform more invasive surgical procedures. 5 The growing number of congenital heart defects amenable to percutaneous treatment, together with the low number of complications, reduced hospitalization time, and reduced hospitalization costs, have made percutaneous interventions an excellent therapeutic option with good results in the short and long term. 5-8
This study aimed to evaluate the profile of patients with congenital heart disease undergoing percutaneous diagnostic or therapeutic procedures in a pediatric cardiology referral centre.
METHODSThis cross-sectional retrospective study assessed the demographic and clinical profiles and outcomes of adult and pediatric patients with congenital heart disease undergoing percutaneous diagnostic or therapeutic procedures performed between 2003 and 2009 in a referral cardiology hospital.
Initially, the interventional pediatric cardiology service’s database was searched, and information was collected to characterize the sample. Then, additional information was collected from the records of the Department of Medical Files (SAME). Variables were obtained related to clinical and demographic characteristics, including gender, age, ethnicity, origin, anthropometric measurements (weight, height, blood pressure, and heart rate), associated comorbidities, previous surgeries and hospitalizations, established medical diagnosis, number and type of percutaneous procedures performed, prostheses used, and clinical events during hospitalization.
A sample size calculation used the proportion of 50% of the total population of 1,961 patients, with a margin of error of 2.2% and a confidence level of 95%, totalling 987 patients. To account for possible follow-up losses due to incomplete records, a sample of 1,002 patients was used.
This research was developed according to the Guidelines and Standards for Research Involving Human Subjects, as stated in Resolution 196/96. The project was approved by the ethics and research committee under registration number 4.431/09. The authors signed the term form for the use of patient records and databases for research projects.
Statistical analyses were performed using SPSS, release 15.0. Categorical variables were expressed as absolute values and percentages, whereas quantitative variables were expressed as the mean and standard deviation or the median and 25 th and 75 th percentiles, when their distributions were normal or non-normal, respectively.
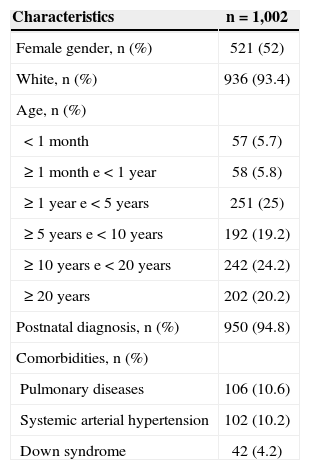
RESULTSA total of 1,002 cases of congenital heart disease submitted to percutaneous interventional and diagnostic procedures were evaluated. Among these patients, 521 (52%) were female. The median age was 33 (0-73) years. Most patients (94.8%) received a heart disease diagnosis after birth. Among the comorbidities evaluated, the most commonly found were pulmonary diseases (10.6% of patients) and systemic arterial hypertension (10.2% of patients). Down syndrome was the most frequent genetic syndrome, present in 4.2% of the cases (Table 1).
Clinical characteristics of the population with congenital heart disease
| Characteristics | n=1,002 |
|---|---|
| Female gender, n (%) | 521 (52) |
| White, n (%) | 936 (93.4) |
| Age, n (%) | |
| <1 month | 57 (5.7) |
| ≥1 month e<1 year | 58 (5.8) |
| ≥1 year e<5 years | 251 (25) |
| ≥5 years e<10 years | 192 (19.2) |
| ≥10 years e<20 years | 242 (24.2) |
| ≥20 years | 202 (20.2) |
| Postnatal diagnosis, n (%) | 950 (94.8) |
| Comorbidities, n (%) | |
| Pulmonary diseases | 106 (10.6) |
| Systemic arterial hypertension | 102 (10.2) |
| Down syndrome | 42 (4.2) |
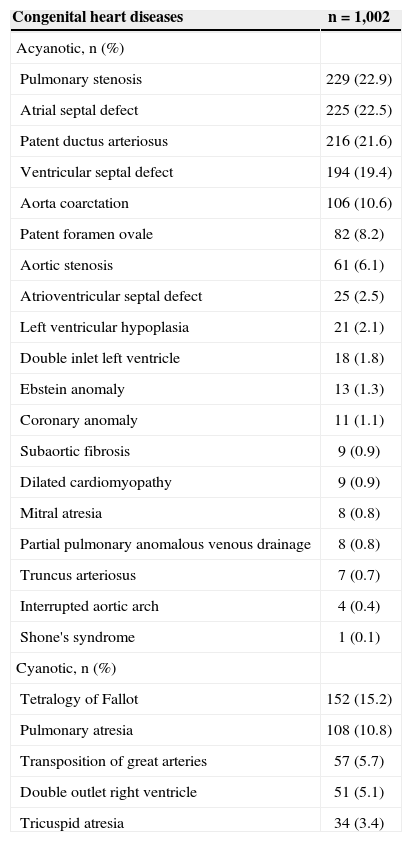
The most prevalent acyanotic congenital heart diseases were pulmonary stenosis (22.9% of patients), atrial septal defect (22.5% of patients), and patent ductus arteriosus (21.6% of patients), all evaluated separately. Among the cyanotic congenital heart diseases, tetralogy of Fallot (15.2% of patients) was the most common, followed by pulmonary atresia (10.8% of patients), and transposition of the great arteries (5.7% of patients) (Table 2).
Types of congenital heart disease diagnosed or percutaneously treated
| Congenital heart diseases | n=1,002 |
|---|---|
| Acyanotic, n (%) | |
| Pulmonary stenosis | 229 (22.9) |
| Atrial septal defect | 225 (22.5) |
| Patent ductus arteriosus | 216 (21.6) |
| Ventricular septal defect | 194 (19.4) |
| Aorta coarctation | 106 (10.6) |
| Patent foramen ovale | 82 (8.2) |
| Aortic stenosis | 61 (6.1) |
| Atrioventricular septal defect | 25 (2.5) |
| Left ventricular hypoplasia | 21 (2.1) |
| Double inlet left ventricle | 18 (1.8) |
| Ebstein anomaly | 13 (1.3) |
| Coronary anomaly | 11 (1.1) |
| Subaortic fibrosis | 9 (0.9) |
| Dilated cardiomyopathy | 9 (0.9) |
| Mitral atresia | 8 (0.8) |
| Partial pulmonary anomalous venous drainage | 8 (0.8) |
| Truncus arteriosus | 7 (0.7) |
| Interrupted aortic arch | 4 (0.4) |
| Shone's syndrome | 1 (0.1) |
| Cyanotic, n (%) | |
| Tetralogy of Fallot | 152 (15.2) |
| Pulmonary atresia | 108 (10.8) |
| Transposition of great arteries | 57 (5.7) |
| Double outlet right ventricle | 51 (5.1) |
| Tricuspid atresia | 34 (3.4) |
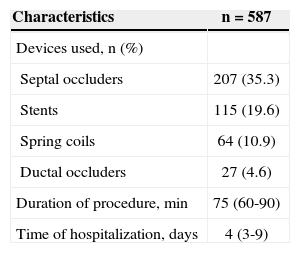
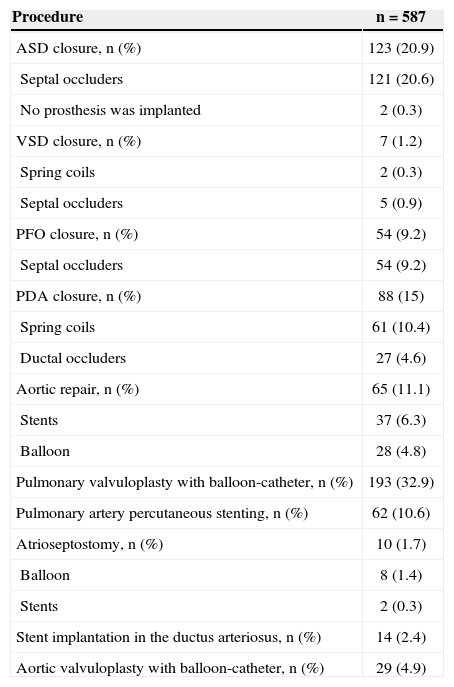
When evaluating data related to percutaneous procedures, it was observed that 587 procedures (58.6%) were therapeutic, of which 193 (32.9%) were pulmonary valvuloplasties, 123 (20.9%) were septal closures, and 88 (15%) were closures of the ductus arteriosus. The average procedure duration was 75 (60-90) minutes and the mean length of hospitalization was four (three to nine) days (Table 3). Therapeutic procedures are described in Table 4.
Treated diseases and devices used in the procedures
| Procedure | n=587 |
|---|---|
| ASD closure, n (%) | 123 (20.9) |
| Septal occluders | 121 (20.6) |
| No prosthesis was implanted | 2 (0.3) |
| VSD closure, n (%) | 7 (1.2) |
| Spring coils | 2 (0.3) |
| Septal occluders | 5 (0.9) |
| PFO closure, n (%) | 54 (9.2) |
| Septal occluders | 54 (9.2) |
| PDA closure, n (%) | 88 (15) |
| Spring coils | 61 (10.4) |
| Ductal occluders | 27 (4.6) |
| Aortic repair, n (%) | 65 (11.1) |
| Stents | 37 (6.3) |
| Balloon | 28 (4.8) |
| Pulmonary valvuloplasty with balloon-catheter, n (%) | 193 (32.9) |
| Pulmonary artery percutaneous stenting, n (%) | 62 (10.6) |
| Atrioseptostomy, n (%) | 10 (1.7) |
| Balloon | 8 (1.4) |
| Stents | 2 (0.3) |
| Stent implantation in the ductus arteriosus, n (%) | 14 (2.4) |
| Aortic valvuloplasty with balloon-catheter, n (%) | 29 (4.9) |
ASD, atrial septal defect; VSD, ventricular septal defect; PFO, patent foramen ovale; PDA, patent ductus arteriosus
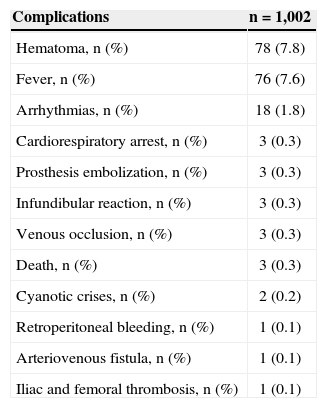
The present results demonstrated that the most prevalent complications related to percutaneous procedures were hematomas at the access route (7.8% of patients) and fever (7.6% of patients). All episodes of fever were isolated and were not associated with procedure-related infections. Complications associated with diagnostic and therapeutic percutaneous procedures are described in Table 5.
Complications associated with diagnostic and therapeutic percutaneous procedures
| Complications | n=1,002 |
|---|---|
| Hematoma, n (%) | 78 (7.8) |
| Fever, n (%) | 76 (7.6) |
| Arrhythmias, n (%) | 18 (1.8) |
| Cardiorespiratory arrest, n (%) | 3 (0.3) |
| Prosthesis embolization, n (%) | 3 (0.3) |
| Infundibular reaction, n (%) | 3 (0.3) |
| Venous occlusion, n (%) | 3 (0.3) |
| Death, n (%) | 3 (0.3) |
| Cyanotic crises, n (%) | 2 (0.2) |
| Retroperitoneal bleeding, n (%) | 1 (0.1) |
| Arteriovenous fistula, n (%) | 1 (0.1) |
| Iliac and femoral thrombosis, n (%) | 1 (0.1) |
The arrhythmias or conduction disorders observed at examination were left bundle branch block, atrial fibrillation, atrial flutter, bradycardia, atrioventricular block, supraventricular tachycardia, and ventricular fibrillation. All arrhythmias were treated or resolved spontaneously during the procedure.
DISCUSSIONThe present study observed a predominance of patients with pulmonary stenosis, atrial septal defect, or patent ductus arteriosus. Previous studies9,10 that assessed populations with similar characteristics, but in clinical and/or surgical patients, showed that ventricular septal defect (VSD) was the most frequent congenital heart disease, which is dissimilar from the present findings. However, these previous studies observed similar results regarding the incidence of cyanotic heart disease; tetralogy of Fallot was the most prevalent among these defects.
The fact that VSD was not the most common congenital heart defect is also noteworthy. Although VSD is the most prevalent, in general, this population currently requires only echocardiography for the diagnosis and does not require cardiac catheterization. Moreover, percutaneous VSD closure is not yet a reality for the patients attended to at the Brazilian Unified Health System (Sistema Único de Saúde – SUS). 7
The present results demonstrated that the congenital heart disease diagnosis was made predominantly in the postnatal period, among 1 to 5 years aged children. During this period, a congenital heart disease diagnosis is obtained more frequently, and most percutaneous therapeutic procedures are performed. 11,12 Thus, in some cases, percutaneous procedures represent a less invasive intervention, without the immediate indication of more aggressive procedures, such as surgical procedures.
Most percutaneous therapeutic procedures performed in this service setting were pulmonary valvuloplasty, closure of atrial septal defect, and closure of patent ductus arteriosus. These data are similar to those of a previously described study, 10 which aimed to define the profile of patients with congenital heart disease in a referral centre in Southern Brazil, but in that study, both percutaneous and surgical therapeutic procedures were evaluated.
In addition to these procedures, the excellent immediate and long-term results achieved by percutaneous repair of atrial septal defect are noteworthy.7 These data reinforce the importance of these therapies in reducing post-procedural comorbidities and length of hospitalization. 13 In developed countries, percutaneous repair of atrial septal defect is certainly the most economical option due to the lower rates of complications and shorter recovery time. Percutaneous repair also provides greater comfort for patients and has a similar efficacy to the surgical technique. However, in developing countries, the cost of the prosthesis is still the main obstacle to the procedure.7
An important result in the present study was the occurrence of minor complications, such as hematomas, fever, and arrhythmias, which were quickly resolved without clinical consequences for patients. The evolution of techniques and devices in paediatric interventional cardiology, such as the use of stents, balloons, and prostheses, has ensured safer procedures with fewer complications by offering other modes of cardiac structure visualization. 14,15
Percutaneous interventions improve quality of life, relieve symptoms, and increase the survival of children with greater clinical complexity in different therapeutic modalities, either as an adjunct therapy or by delaying surgical interventions. The prevention of complications after coronary interventions should be a concern of health professionals who work in paediatric interventional cardiology, as these complications have a significant impact on patients’ bed confinement, prolonging hospitalization, and increasing medical and nursing procedures. It is necessary to develop care protocols to minimize the predictors of complications and standardize multidisciplinary care for this group of patients.
CONCLUSIONSThe results of this study demonstrated the predominance of therapeutic procedures in patients with acyanotic congenital heart diseases performed with low complication rates in a tertiary referral centre.
CONFLICT OF INTERESTThe authors declare no conflict of interest.