We discuss some aspects related to the legal framework, international recommendations and training programs on radiological protection; image quality and equipment; the biological effects and risks of ionizing radiation; lesions in patients and operators; patient’s reference levels; occupational dose limit and preventive actions. The use of ionizing radiation involves risks that are justified in diagnostic and therapeutic procedures. The awareness and knowledge of these risks minimizes the damage, optimizing the quality of images and safe use of ionizing radiation. There is evidence of radiation induced cataracts in individuals who work in catheterization laboratories. Several studies suggest there may be a significant risk of lens opacity, if radiological protection devices are not properly used. Additionally, these interventional procedures are performed in Latin America, usually by medical specialists in collaboration with nurses, technologists and technicians, who often do not have adequate training in radiological protection.
Riscos da Radiação X e a Importância da Proteção Radiológica na Cardiologia Intervencionista: Uma Revisão Sistemática
Discutimos aqui aspectos vinculados ao enquadramento legal, a recomendações internacionais e a programas de formação em proteção radiológica; ao angiográfico e à qualidade da imagem; aos efeitos biológicos e aos riscos das radiações ionizantes; às lesões em operadores e pacientes; aos níveis de referência do paciente; ao limite de dose ocupacional e a suas medidas de prevenção. O uso das radiações ionizantes acarreta riscos, que, contudo, justificam-se em procedimentos diagnósticos e terapêuticos. A consciência e o conhecimento desses riscos mi minimizam o dano, otimizando a qualidade das imagens e o uso seguro das radiações ionizantes. Tem-se demonstrado a ocorrência de cataratas radioinduzidas em trabalhadores de laboratórios de cateterismo. Diversos estudos sugerem que pode haver um risco significativo de opacidade do cristalino, caso não se utilizem adequadamente os dispositivos de proteção radiológica. Adicionalmente, esses tipos de procedimentos intervencionistas são realizados na América Latina, geralmente por médicos especialistas, com a colaboração de enfermeiros, tecnólogos e técnicos, que, muitas vezes, não têm formação adequada em proteção radiológica.
Medical applications represent the main source of artificial exposure of the world’s population to ionizing radiation. The National Council on Radiation Protection and Measurements (NCRP),1 in the United States, estimated that radiation exposure aimed at the production of medical images has increased by 600% between 1980 and 2006. According to the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR),2 interventional cardiology procedures represent the third largest contribution to the collective dose (a collective dose characterizes radiological impact of a procedure or ionizing source), after computed tomography and nuclear medicine.
The introduction of new imaging technologies in the diagnosis and therapeutic field and the ongoing modernization of X-ray machines have broadened the spectrum of interventional cardiology activity, currently responsible for several procedures in coronary, valvular, and congenital diseases. To ensure that equipment functions adequately and to properly manage the radiological risks, quality assurance and control programs should be established in interventional cardiology services, as recommended by the International Atomic Energy Agency (IAEA).
Due to high levels of exposure that can be produced by some interventional cardiology procedures, it is possible to observe secondary effects in patients submitted to high doses (deterministic), or proportional to the received doses without limit (stochastic). However, as the procedure requires the presence of the physician at the patient’s side, it is also possible that these deterministic effects occur in the professionals, such as cataracts and epilation.
International recommendations and legal framework for radiation protectionUnlike the scenario in Europe and the United States,3−7 there is not enough legal framework to regulate the safe use of ionizing radiation in medicine in Latin America generally. The awareness that there are interventional procedures that can result in high radiation doses to the patient and the technician has motivated the international organizations to publish recommendations to help combine the needs of interventional cardiology and high safety standards. Thus, the 97/43/Euratom European Directive5 on medical exposures determines requirements for the practice of interventional cardiology. A guide published by the European Commission, aiming at the education and training in radiation protection for medical exposures, also contains recommendations on training and accreditation programs.6−8
The document “Radiation Safety in the Practice of Cardiology”,4 published jointly by the American College of Cardiology (ACC), the North American Society of Pacing and Electrophysiology (NASPE), the Society for Cardiac Angiography and Interventions (SCAI), and the American Society of Nuclear Cardiology (ASNC), establishes recommendations on radiation protection, so that cardiology procedures can be performed with appropriate safety levels. Likewise, the publication “Normas de Seguridad del OIEA No GSR Part 3”9 and publications 60, 103, and 105 of the International Commission on Radiological Protection (ICRP)10−12 institute the basic criteria for radioprotection by establishing principles of justification, optimization, and limitation of doses for occupationally exposed individuals (OEI), as well as dose reference values for medical practices.
Chambers et al.,13,14 who were members of SCAI, published an article whose practical approach was to assist interventional cardiology services to establish safety and radiation protection programs. They reviewed the following: basic terminology for planning the dose before the procedure; managing the dose in real time; documentation of radiation dose in the records; notification of high dose to the patient and the referring physician; protection elements and imaging equipment; and training. The article also stated that the doctors and medical staff involved in catheterization should be trained in the basic principles of radiation physics, safety, and radiation protection. A medical physicist should participate, together with the medical staff, in the selection of equipment, staff education, and dose measurement. Better image quality with optimized radiation exposure ensures the best patient care, as well as improves practice.
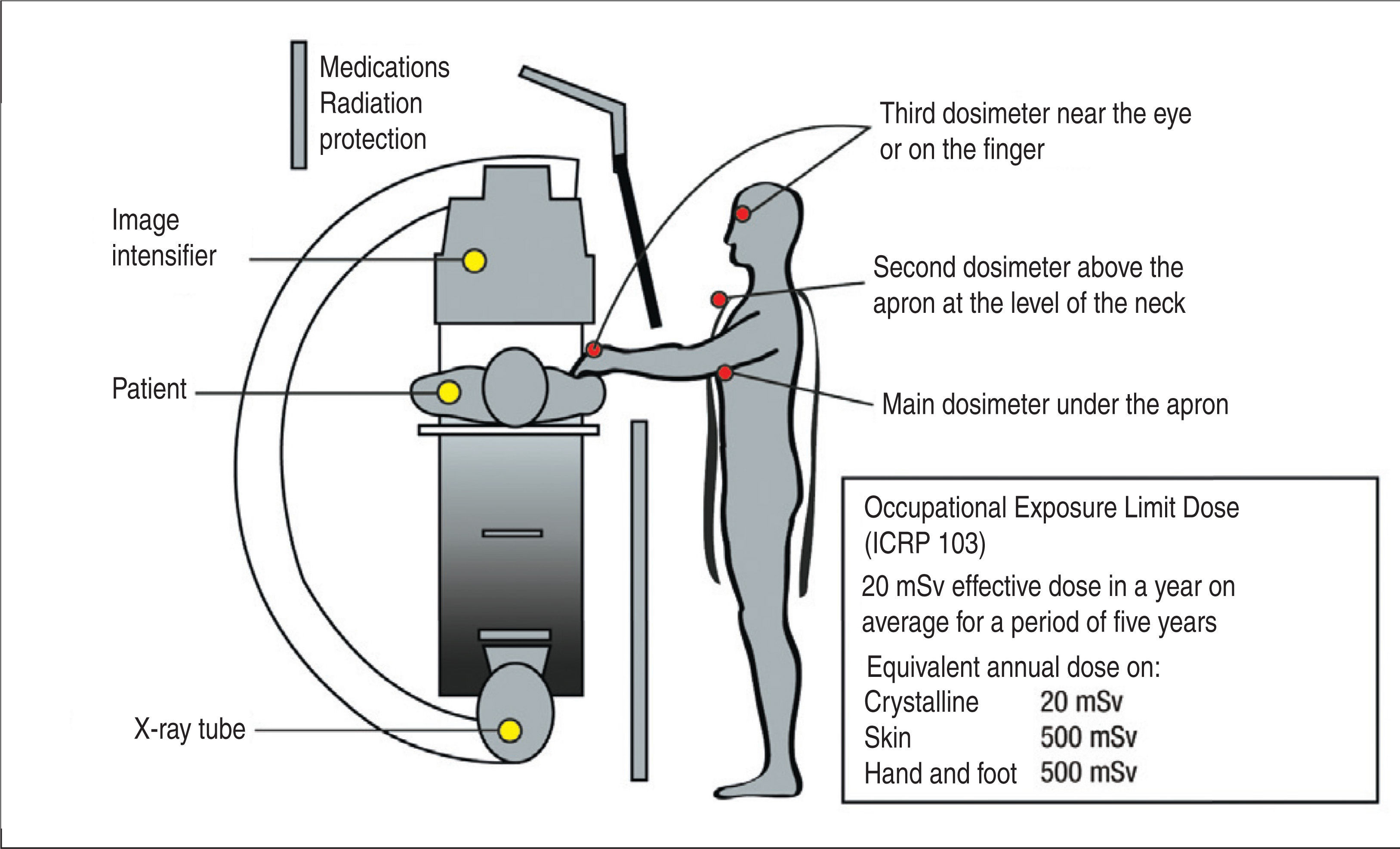
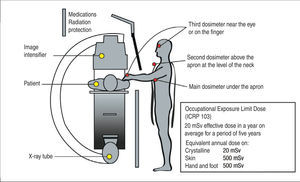
The ICRP Publication 8515 recommends the use of three dosimeters for more exposed individuals. It is suggested to place a main personal dosimeter under the lead apron at chest level, directed to the radiation source; a second dosimeter should be located above the apron at the neck level; and a third near the eye (crystalline lens) or the hand (Figure 1) region. The Brazilian normative rules require the use of a dosimeter at chest level, outside of the lead apron.16
– Position of dosimeters to describe the exposure of staff during interventional procedures. The main personal dosimeter must be under the lead apron, at the level of the chest, directed towards the radiation source. The second dosimeter can be located above the apron at the level of the neck, and the third close to the eye or hand.
The IAEA recommends including in radiation protection legislation the implementation of quality assurance and control programs, with acceptance tests and “commissioning” or characterization of systems that produce ionizing radiation used during interventional procedures. In Brazil, in 1998 the Brazilian National Health Surveillance Agency (Agência Nacional de Vigilância Sanitária – ANVISA) of the Ministry of Health published the SVS/MS 453/98 Administrative Rules,16 which establishes requirements for radiation protection and quality control for medical, dental, and interventional radiology.
Although there is not yet a specific regulation for the use of ionizing radiation in interventional cardiology, a regulatory standard – Safety and Health at Work in Healthcare Services, known as NR-32,17 establishes the basic guidelines to protect the health of healthcare workers. It establishes that the fluoroscopy equipment must have “an inferior and lateral lead curtain or apron to protect the technician against scattered radiation.” In Europe and other countries,5−7 it is not allowed to commercialize angiography equipment without the external elements of radiation protection, nor without the kerma-area product measurement device (or dosearea product – PKA), which indicates the dose of radiation that the patient receives, and is an indispensable tool for the safety and optimization of interventional procedures. In Brazil, devices to measure PKA, and external elements of radiation protection, such as the apron and ceiling screen are still unusual, but should be considered an indispensable part of the acquisition of angiographic equipment.
Training in radiological protectionIn Latin America, the interventional procedures are performed by medical experts accompanied by nurses, medical technologists, and technicians, who often do not have adequate training in radiation protection. Research conducted by Vano et al.18 in ten centers of interventional cardiology in Latin American countries – including Brazil – observed that only 64% of the OEIs used the individual monitor (dosimeters), and only 36% acknowledged knowing what their dosimetry meant. Regarding the knowledge and use of the angiographer, only 14% demonstrated adequate knowledge of the equipment, and only 27% were aware of the quality control results. In another survey conducted by the IAEA, which was answered by cardiologists from more than 56 countries, the results showed that between 33% and 77% of interventional cardiologists regularly used their dosimeters.19
In 2005, a joint publication of the ACC, the American Heart Association, and the American College of Physicians (ACC/AHA/ACP)20 defined the clinical competences in medical knowledge, in order to improve patient safety and image quality. Other publications of the ACC, especially those dealing with safe performance of procedures, led to the publication of the document “Cardiac Catheterization Laboratory Standards: a Report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents”,21 which set the technical standards for cardiac catheterization laboratories and has one of its chapters devoted to radiation protection.
The regulation of ionizing radiation in medical exposures of the European Commission6 and the UK (the Ionising Radiation [Medical Exposure] Regulation – IRMER)7 established the proper training, both theoretical and practical, that an interventional procedure technician should receive. Currently, in Spain, interventional cardiologists should have accreditation in radiation protection, especially focused on the interventional area.22
The angiographer and image qualityInterventional medical doctors and physicists should participate in the purchase and setup of angiography equipment. It must be determined which procedures will be performed, so that the most appropriate angiographer can be chosen, according to the demand. The wide variety of procedures that can be performed and the great differences between the hardware components, software, and settings required for different applications make the angiographer a highly-complex device.
To perform the procedures in interventional cardiology, an angiographer especially designed and configured for such medical practice is needed. The equipment must be installed in a room to allow free movement of the C arch, staff circulation, and the installation of all devices required for interventional practice, such as monitors, ceiling screen, defibrillator, pumps, injectors, anesthesia devices, and physiological monitors, among others. The room must allow for patient care procedures and minimize risks to the patient and clinical team.
The desirable characteristics for an angiographer used in interventional cardiology are:
- 1.
Geometry: the X-ray tube and image receptor revolve around a point called “isocenter”, which must be positioned on the anatomical region of interest in the study;
- 2.
Fluoroscopy modes: the choice of different pulse rates must be available to the technician. The incorporation of pulsed fluoroscopy was an important advance in reducing the dose to the patient;
- 3.
Filters: different filter thicknesses are available, depending on the patient’s tissue thickness and density. The filters help in image quality and dosimetric control of the patient;
- 4.
Collimation adjustment: virtual collimation shows the position of the collimator blades on the image, while the blades are adjusted. This feature eliminates patient irradiation during the collimator adjustment. Appropriate collimation reduces patient and technician dose and improves image quality;
- 5.
Anatomical programming: allows for the control of the dose management and image quality by selecting the body region and the size of the patient to be irradiated;
- 6.
Digital acquisition: the processing of non-digital images is very limited, compared with that of digital images. The Digital Images and Communications in Medicine (DICOM) format represents the main file type used for the acquisition, management, and manipulation of images in interventional cardiology. The DICOM header provides important information about the protocols used in the center for each procedure;
- 7.
Fluoroscopy storage: this feature shows the last fluoroscopic image and enables retrospective storage of the last seconds of fluoroscopy. The feature allows the technician to store up to 300 images of the fluoroscopy sequence and allows the recording of cardiac anatomy without the need to irradiate the patient again;
- 8.
Radiation monitors: allows real-time visualization of air kerma (Ka) and PKA. This monitor enables the assessment of radiation risk of the patient during the procedure. The interventional cardiology service must record patients’ doses and implement a follow-up system to overcome the alert dose;
- 9.
Shielding/external radiation protection elements: these shields consist of lead curtains mounted on the rail of the patient table (skirt) and another shield fitted with a articulated arm, attached to the roof of the procedure room (ceiling screen). The typical equivalent thickness is 0.5 mmPb. The ceiling screen has an advantage compared to goggles as, besides protecting the crystalline lens, it also protects the head, thyroid, arms, and entire upper torso of the technician;
- 10.
Audible alerts: an audible alert shall be activated in the procedure room whenever X-ray s are produced. Different sounds for different modes of operation are desirable.
An angiographer for complex examinations that lacks most of the above-mentioned characteristics should not be used in invasive cardiology.23
Appropriate adjustment of all parameters of the angiographer, such as the pulse rate and width, tube current and voltage, filtration, and size of the focal point and field of view contributes to the optimization of patient exposure and image quality improvement.
Currently, fluoroscopic systems used in interventional cardiology procedures utilize two types of technology for image detection: the image intensifier with coupled charge device, and flat panel detectors, which came to replace the image intensifier. Several studies have compared both technologies, emphasizing that there are no significant differences in the dose level and image quality between them.24,25 Moreover, they also emphasize the great potential to reduce doses and improve the image quality of flat panel detectors.
In Brazil, the work of Medeiros et al.26 and Vargas et al.27 demonstrated that the angiographer with flat panel showed the highest rate of maximum Ka entering the patient’s skin, reaching 65% higher compared to systems using an image intensifier. Therefore, dose reduction is not inherent to the flat panel system and dose optimization by a qualified medical physicist is required.
Image quality and dose are strongly related. Dose reduction causes a decrease in image quality, so that overcautious steps to obtain low doses can result in angiographers generating low-quality images.
Good-quality images are essential in guiding the clinical procedure. Thus, the evaluation of image quality can be made objectively or subjectively.28 A specific phantom is required for systems using fluoroscopy to evaluate image quality. Subjective evaluation requires an observer to report the number of groups of visible high resolution and low-contrast objects. This type of evaluation is subject to observer variability. The objective evaluation (numerical) can be performed with DICOM images. Evaluations may include modulation transfer function, noise, contrast, and signal-to-noise ratio. The numerical evaluations of image quality are more time-consuming than the subjective evaluations, but are very consistent.
The verification of image quality and dose for different exposure modes is the basis of consistency (performance verification tests) and commissioning tests. This process is critical to improve the quality of clinically acceptable images obtained with dose rates that are as low as reasonably achievable. Thus, it is essential to fully characterize the X-ray system during commissioning and after major changes. If this task is not yet accomplished, it is the first step in the optimization process.
Biological effects of ionizing radiationMost unwanted effects resulting from ionizing radiation exposure can be grouped into two categories:
- 1.
Stochastic effects: those whose probability of occurrence is proportional to the radiation dose received without the existence of limits. The development of cancer in exposed individuals due to mutation of somatic cells or by hereditary disease in their offspring is an example;
- 2.
Deterministic effects: those caused by total or localized irradiation of a tissue, leading to a degree of cell death not counterbalanced by replacement or repair, with detectable damage in tissue or organ function. There is a dose limit, below which cell loss is insufficient to damage the tissue or organ in a detectable manner.
The ICRP 10311 warns that some effects associated with radiation, different from cancer, are not yet sufficiently understood to be placed in either of the afore-mentioned categories.
The two most common examples of tissue reactions (deterministic effects) of interest in interventional cardiology are the formation of cataracts in physicians, and skin lesions in patients.29
The study of deterministic effects is based on the analysis of the spatial and temporal distribution of doses on the tissue. A single dose of 6 to 8Gy on a 5cm2 field results in the appearance of erythema, which increases during the first week, but gradually disappears after ten days. With an increasing dose, erythematous reaction reaches a maximum at two weeks and lasts 20 to 30 days. In case of even larger doses, dry or moist desquamation and even necrosis may occur.30
The appropriate magnitude to plan patient exposure and risk-benefit assessments is the equivalent dose or the absorbed dose in irradiated tissues (whose unit is the Sievert – Sv, and Gray – Gy, respectively). The effective dose may be valuable to compare the doses of different diagnostic procedures, as well as to establish a parallel of the use of similar technologies and procedures in different hospitals and countries.11
Reviews of biological and clinical data performed by the ICRP 103 have estimated that for an absorbed dose of 100mGy, no tissue shows clinically relevant functional damage.11 This estimate applies to single acute doses or situations in which the dose is received in a prolonged manner, such as annual exposures. In the case of cancer, the studies have shown evidence of radiation risk at doses around 100mSv or possibly smaller.
In the case of hereditary diseases, there is still no direct evidence that radiation exposure of parents results in greater prevalence of hereditary diseases in their offspring, although the ICRP 103 has considered that radiation causes hereditary effects in experimental animals. These experimental observations were sufficient for risks to future generations to be included in protection systems. In accordance with ICRP 103, there is a risk of tissue reaction and malformation of the irradiated embryo and fetus in utero. In the case of embryo, there may be lethal effects during the pre-implantation period. Regarding malformations, radiosensitivity patterns in utero depend on the gestational age. The limit for malformation induction is approximately 100mGy; below this value, malformations are not expected.
The practical system of radiological protection recommended by ICRP 103 is based on the assumption that, for doses>100mSv, an increase in the dose produces a directly proportional increase in the probability of developing cancer or hereditary effects of radiation.11 This model of dose response is known as “linear-non-threshold” (LNT). This criterion was shared by UNSCEAR 2000,31 NCRP 2001-2009,1,32 and NAS/ NRC 2006.33 Publication 99 of ICRP 2005 considered that the adoption of the LNT model, combined with an estimated value of the effective dose and dose rate factor, provides a prudent basis for the practical purposes of radiation protection, i.e., the management of risks from exposure to low doses of radiation.34
Lesions in patients and techniciansUnfortunately, some patients undergoing interventional procedures have suffered radiation damage (Figures 2 and 3).35,36 One of the earliest records of skin necrosis caused by fluoroscopy-guided catheterization dates from 1976.37 However, it was only in the 1990s that the Food and Drug Administration (FDA) issued a warning drawing attention to the risks of skin lesions caused by radiation in patients undergoing medical procedures with fluoroscopy.3
– Skin lesion in a 40-year-old man submitted to multiple coronary angiograms. Approximately 18 to 21 months after the procedure, there is evidence of tissue necrosis.
– 17-year-old adolescent with a history of cardiac arrhythmia, submitted to two ablations, with a 13-months interval between them. Picture taken two years after the last intervention, showing a hardened plaque and atrophy on the lateral chest, affecting the right breast. The hardening resulted in movement limitation of the right arm. There is an increased risk of breast cancer.
In Chile, with the support of the IAEA, a survey was performed at an interventional cardiology laboratory. Of the respondents, 90% declared they were unaware of cases of lesions secondary to radiation, and 84% said they had never seen excessive exposure of patients.38 In Brazil, the authors found it difficult to find such cases.
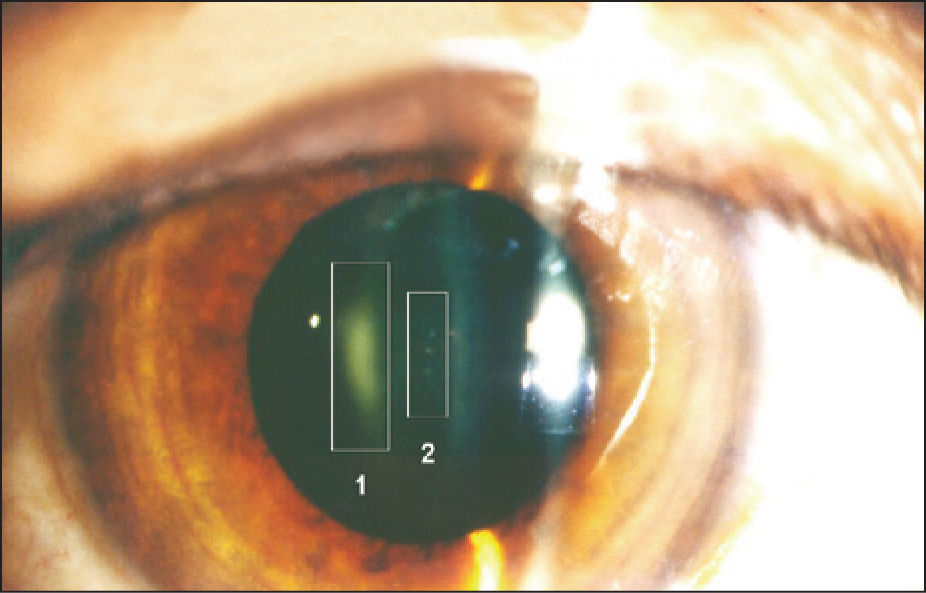
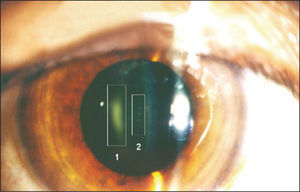
The occurrence of radiation-induced cataracts among workers in interventional radiology laboratories has been demonstrated (Figure 4).15,39−41 Vano et al.42 revealed that 50% of cardiologists exposed to ionizing radiation showed crystalline lens opacity. Studies aiming to evaluate crystalline lens lesions retrospectively and the radiation dose, as the Retrospective Evaluation of Lens Injuries and Dose (RELID), of IAEA,43 contributed to the reduction of dose limits for that region. Because interventional physicians and their teams remain near the X-ray source for several hours each day, even under normal working conditions, the levels of exposure to the eyes may still be quite high.
– Radio-induced crystalline lens opacity in an interventional radiology specialist submitted to high levels of radiation spread using a non-optimized angiographer with an X-ray tube above the table. Region 1 indicates posterior subcapsular opacity; region 2, perinuclear punctate opacities.
The study by Russo et al.44 demonstrated that interventional cardiologists have increased somatic DNA damage, i.e., chronic exposure to low doses of ionizing radiation induces adaptive, biochemical, and cell responses to low doses, even at levels considered as safe exposure; thus, the use of radiation protection measures is essential.
Almeida Junior et al.45 showed that annual doses of OEIs in the intervention lab easily exceeded the legal limit allowed to workers exposed to ionizing radiation if radiation protection devices were not used during the interventional procedures.46
The occurrence of cataracts is considered a deterministic effect. The ICRP observed epidemiological evidence and issued, in April 2011, a statement that lowered the dose limit for which this effect is expected to occur.47 According to this statement, the absorbed dose limit for lesions in the crystalline lens became 0.5Gy (500mGy), and the occupational dose-equivalent limit for the lens became 20mSv per year. Estimates indicate that the doses accumulated by interventional physicians and medical teams during the professional life can exceed these values established by international standards.
Reference levels for patient and occupational dose limitsLarge differences in exposures in the same therapeutic or diagnostic test indicate that there is great potential for dose reduction.28 The concept of reference levels was developed as a tool for optimization of protection regarding patient exposure. Reference levels are defined as the measured values, above which a specific action or decision must be made. They are used to identify situations in which patient doses are often out of the ordinary. If it is verified that exposures during procedures are consistently different from the reference level, procedures and equipment should be revised to determine whether they were properly adjusted. The reference levels are intended for use in quality assurance programs, serving as guides to determine the detailed assessment of the equipment, and also to ensure the best performance of the technician.
In countries that have implemented reference levels, physicians and medical teams have an easy-to-use tool to compare radiation doses delivered to patients. This has resulted in greater awareness of professionals regarding radiation doses associated with practices, stimulating corrective actions in each institution.11,28,48 In these countries, a significant reduction has been observed in radiation doses to patients.18,49 Reference levels, therefore, are well established for common procedures, and are required by international recommendations.9,11,28,48
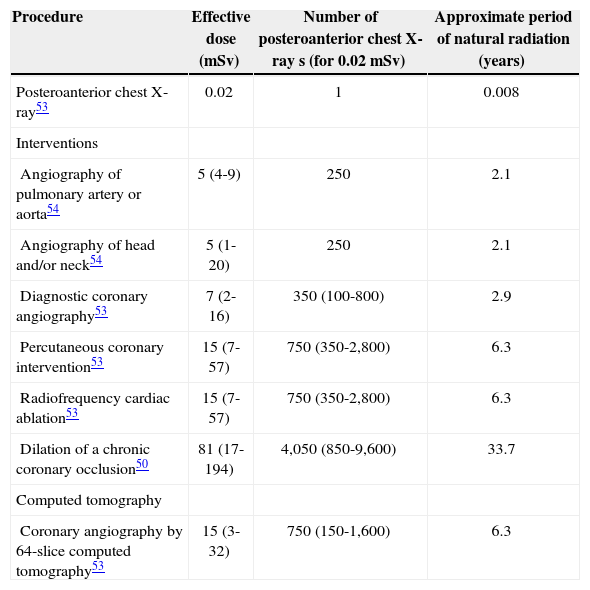
Doses in interventional cardiology procedures can vary by a factor of ten (Table 1) in complex procedures, such as intervention in chronic coronary occlusion,50 transthoracic aortic valve replacement,51 or the endovascular repair of a thoracic-abdominal aneurysm,52 which may exceed the effective dose of 100mSv.
Effective dose for common evaluations in cardiology29 associated with the equivalent chest radiography number and the approximate period of natural radiation that an individual receives in one year
| Procedure | Effective dose (mSv) | Number of posteroanterior chest X-ray s (for 0.02mSv) | Approximate period of natural radiation (years) |
|---|---|---|---|
| Posteroanterior chest X-ray53 | 0.02 | 1 | 0.008 |
| Interventions | |||
| Angiography of pulmonary artery or aorta54 | 5 (4-9) | 250 | 2.1 |
| Angiography of head and/or neck54 | 5 (1-20) | 250 | 2.1 |
| Diagnostic coronary angiography53 | 7 (2-16) | 350 (100-800) | 2.9 |
| Percutaneous coronary intervention53 | 15 (7-57) | 750 (350-2,800) | 6.3 |
| Radiofrequency cardiac ablation53 | 15 (7-57) | 750 (350-2,800) | 6.3 |
| Dilation of a chronic coronary occlusion50 | 81 (17-194) | 4,050 (850-9,600) | 33.7 |
| Computed tomography | |||
| Coronary angiography by 64-slice computed tomography53 | 15 (3-32) | 750 (150-1,600) | 6.3 |
The kerma-area product (KAP) is a figure that represents the radiation energy transmitted to the patient during the procedure, expressed as Gy×cm2. This magnitude is calculated by angiography system and displayed on the room monitor during the procedure. Knowing the patient’s KAP, it is possible to estimate the dose that the technician receives. The IAEA, in their publication Safety Report Series No 59,28 established reference levels of 50Gy×cm2 for diagnostic coronary angiography and 125Gy×cm2 for percutaneous coronary intervention (PCI), considering the fluoroscopy time, the number of images, and procedure complexity.
The national literature has scarce reports of patient doses in interventional cardiology. Surveys conducted in the State of Rio Grande do Sul showed that KAP in Interventional Cardiology procedures varied between 41-55Gy×cm2 and 62-103Gy×cm2, for diagnostic and therapeutic procedures, respectively (third quartile values).26,27,55
The study by Azevedo et al.55 determined the impact of complex lesions in radiation exposure during PCI. It was concluded that radiation exposure is significantly higher in patients undergoing PCI in type B2/C complex lesions, when compared to type A/B1, and that patient weight and the type of lesion (B2/C) are predictors of increased radiation exposure. They also reported that 14% of patients undergoing PCI exceeded the dose level of 2Gy, which can potentially produce lesions in the patient.
Vargas et al.27 also reported that, in some patients, the dose exceeded the reference level by 2Gy. The study showed that radiation exposure was>2Gy in 3.6% of procedures in the group weighing less than 79kg, 16.3% in the group between 80 and 99kg, and 10.7% in the group greater than 100kg. Thus, the patient’s weight has a significant impact on radiation exposure.
On the other hand, Mattos et al.56 demonstrated that patients undergoing invasive cardiology procedures, both diagnostic and therapeutic, were exposed to higher levels of radiation via the radial approach, and suggested that the technician’s experience can significantly reduce the dose level of the procedure.
These studies demonstrated the great potential for dose optimization of interventional procedures. International recommendations state that, if the dose is>2Gy, this should be recorded in the medical file and the patient should be notified for further follow-up.23,28
An experienced interventional cardiologist, who performs a large volume of catheterizations, has an approximate equivalent exposure of 5mSv per year and a cumulative risk by work activity of one in 100.57,58 The risk is cumulative for the patient and the physician; this means that the greater the number of procedures performed, the greater the dose and the risks. According to current risk estimates, if 100 individuals were exposed to 100mSv, 42 will develop a spontaneous cancer (regardless of radiation exposure), and one will develop a radiation-induced cancer (with a range of uncertainty of one in 30 to one in 300). The risk is three- to four-fold higher in children and 50% lower in populations aged>80 years, when compared with a group of patients aged 50 years, and is 38% higher in women than in men.29,57
In Brazil, the limits of doses for OEIs are established by Decree 453.16 It was established that the mean annual effective dose should not exceed 20mSv in any 5-year consecutive period, and may not exceed 50mSv in any year. The annual equivalent dose should not exceed 500mSv for extremities and 150mSv for the crystalline lens.
Dose limits do not apply to patients, because the objective is diagnosis or treatment. Reference levels are applied, which can be compared to the radiation doses between groups to verify whether the recommended values for certain practices are being respected. If the dose result is greater, equipment review is required, as well as a review of how the work is performed; if lower levels are obtained, the review of image quality is required, which may be inadequate.
RecommendationsIn general, education and training of professionals and society should be mandatory. It is necessary to introduce the teaching of radiation protection at the undergraduate level in medical schools. Hospitals should provide systematic radiation protection courses. Investing in security is investing in health.
One of the objectives of radiation protection is to avoid the unnecessary use of ionizing radiation, adequately justifying each procedure (justification principle).59 This principle states that exposure to radiation should produce enough benefit to compensate the damage that it can cause.6−13 Procedures should be performed with minimal radiation dose.
The training of professionals involved in the field of interventional cardiology should emphasize radiation protection;19−23 furthermore, the equipment emitting ionizing radiation must undergo quality assurance programs that allow for the reduction of exposure to ionizing radiation to levels as low as reasonably achievable (ALARA principle),9−13 minimizing risks to the patient and the medical team.
The principle of optimization advocates a balance between risk and benefit. Potential radiation risks are accepted provided there is proper dose management for all imaging procedures. 59−61 There are several international and some national publications on recommendations and methodologies for dose management, protection of patients and staff, and tutorials in radiation physics, which are fundamental for the practice of safety and dose administration.9−15,20−23,59−64 All OEIs in procedures using fluoroscopy should become familiar with these documents and other relevant literature in this area.
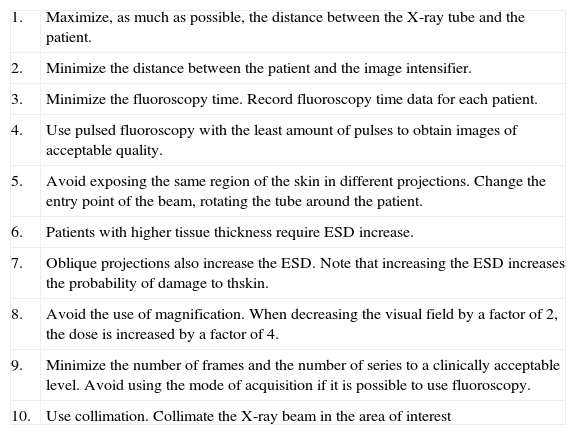
In general, the use of practices that protect the patient also minimizes the risks for the medical team. The physician is responsible for the interventional procedure and must be aware of ionizing radiation risks. Charts 1 and 2, published by the IAEA in 2010,62,63 present recommendations for radiation protection in the interventional cardiology laboratory.
Ten recommendations for the protection of patients in fluoroscopy62
| 1. | Maximize, as much as possible, the distance between the X-ray tube and the patient. |
| 2. | Minimize the distance between the patient and the image intensifier. |
| 3. | Minimize the fluoroscopy time. Record fluoroscopy time data for each patient. |
| 4. | Use pulsed fluoroscopy with the least amount of pulses to obtain images of acceptable quality. |
| 5. | Avoid exposing the same region of the skin in different projections. Change the entry point of the beam, rotating the tube around the patient. |
| 6. | Patients with higher tissue thickness require ESD increase. |
| 7. | Oblique projections also increase the ESD. Note that increasing the ESD increases the probability of damage to thskin. |
| 8. | Avoid the use of magnification. When decreasing the visual field by a factor of 2, the dose is increased by a factor of 4. |
| 9. | Minimize the number of frames and the number of series to a clinically acceptable level. Avoid using the mode of acquisition if it is possible to use fluoroscopy. |
| 10. | Use collimation. Collimate the X-ray beam in the area of interest |
ESD: entrance surface dose.
Ten recommendations for the protection of staff working in fluoroscopy63
| 1. | Wear protective devices |
| 2. | Make good use of the principles of time – distance – shielding: minimize time, maximize the distance as much as clinically possible, and use the shield. |
| 3. | Use the ceiling screens, lateral shields, and lead curtains below the table or apron. |
| 4. | Keep your hands away from the primary X-ray beam at all times. |
| 5. | Only 1% to 5% of the radiation that is incident on the patient entrance goes to the image sensor. |
| 6. | Keep the X-ray tube under the table, not on it. |
| 7. | Use your personal dosimeter. |
| 8. | Periodically update your knowledge on radiological protection. |
| 9. | Expose your questions on radiation protection to experts in radiological protection. (medical physics expert) |
| 10. | Remember: |
| – | Quality control of fluoroscopy equipment allows you to work safely. |
| – | Know your equipment. Using the characteristics of the equipment helps to properly reduce the dose to the patient and staff. |
| – | Use automatic contrast injection pumps. |
All individuals participating in the interventional procedure should have personal protection elements. There is an apron specially designed for the practice, which may be tubular with a belt for weight distribution, and a set (jacket and skirt), with protection equivalent to 0.5 mmPb, which attenuates approximately 95% of the spread radiation to 70kV. Goggles are necessary for crystalline lens protection, with protection equivalent to 0.25 mmPb and lateral shielding. Additionally, the thyroid shield should be incorporated, with a protection of 0.35 mmPb.15
Personal protection garments need daily care, which involves proper storing, cleaning, and periodic inspection for damage in protection suits.
Another shielding system for technician protection is the external protection elements, such as the apron and the ceiling screen, which are also provided by the manufacturers of angiographers. The mobile screen provides protection for medical staff inside the procedure room. These elements provide significant protection against scattered radiation, although some technicians consider them cumbersome. The apron provides efficient protection to the technicians’ lower torso, particularly the gonads, and its use is customary in all interventional procedures.
The transparent ceiling screen provides significant protection for the technician’s upper torso, particularly the head, thyroid, and crystalline lens.23 When positioning the ceiling screen, the source of scattered radiation caused by the patient must be considered, and the protection should be placed to attenuate this radiation. A ceiling screen of 1 mmPb and glasses with a protection equivalent to 0.5 mmPb can reduce the scattered radiation that reaches the crystalline lens by a factor of 0.015 and 0.03 respectively,39 i.e., only 2% to 3 % (98% to 97% attenuation) of the scattered radiation would be transmitted to the crystalline lens. These factors can vary according to the dynamics of the procedure, mainly by modifying the quality of the scattered radiation.
Other studies show that glasses with 0.75 mmPb protection can attenuate between 30% to 88% of the scattered radiation due to the backscattering of the head and the angle of radiation incidence. The study by McVey et al.64 confirmed that the backscatter caused by the technician’s head is the main limitation for dose reduction provided by the goggles. Thus, the use of a ceiling screen is strongly recommended.
The adequate use of radiation protection elements can significantly reduce radiation exposure for the interventional cardiology staff, preventing, for instance, crystalline lens opacity. However, variability in the attenuation power of the radiation protection elements and the fact that the way a particular procedure is performed is technician-dependent mean that the main sources of protection are the awareness and knowledge that the technician has of the radiation risk – which is often undervalued.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.
FUNDING SOURCESNone.
To physicians Carlos Ubeda, from the University of Tarapaca in Chile, and Alejandro Nader, Technical Officer of Radiation Protection in Medicine at the International Atomic Energy Agency, for intellectual and technical input. The author F. L. thanks the postgraduate course of the Center for Development of Nuclear Technology (CDTN) and the National Nuclear Energy Commission (CNEN) for a PhD scholarship.