Percutaneous balloon mitral valvotomy is safe and effective in patients with severe symptomatic mitral stenosis with immediate and long-term results comparable to those of surgical intervention. This study was aimed at reporting the very late follow-up results of the first percutaneous balloon mitral valvotomies performed at our institution and at identifying predictive factors of restenosis.
MethodsFrom 1987 to 1991, 200 consecutive patients were submitted to percutaneous balloon mitral valvotomy. Clinical and echocardiographic evaluations were performed prior to the procedure, 48 hours after the procedure and annually thereafter.
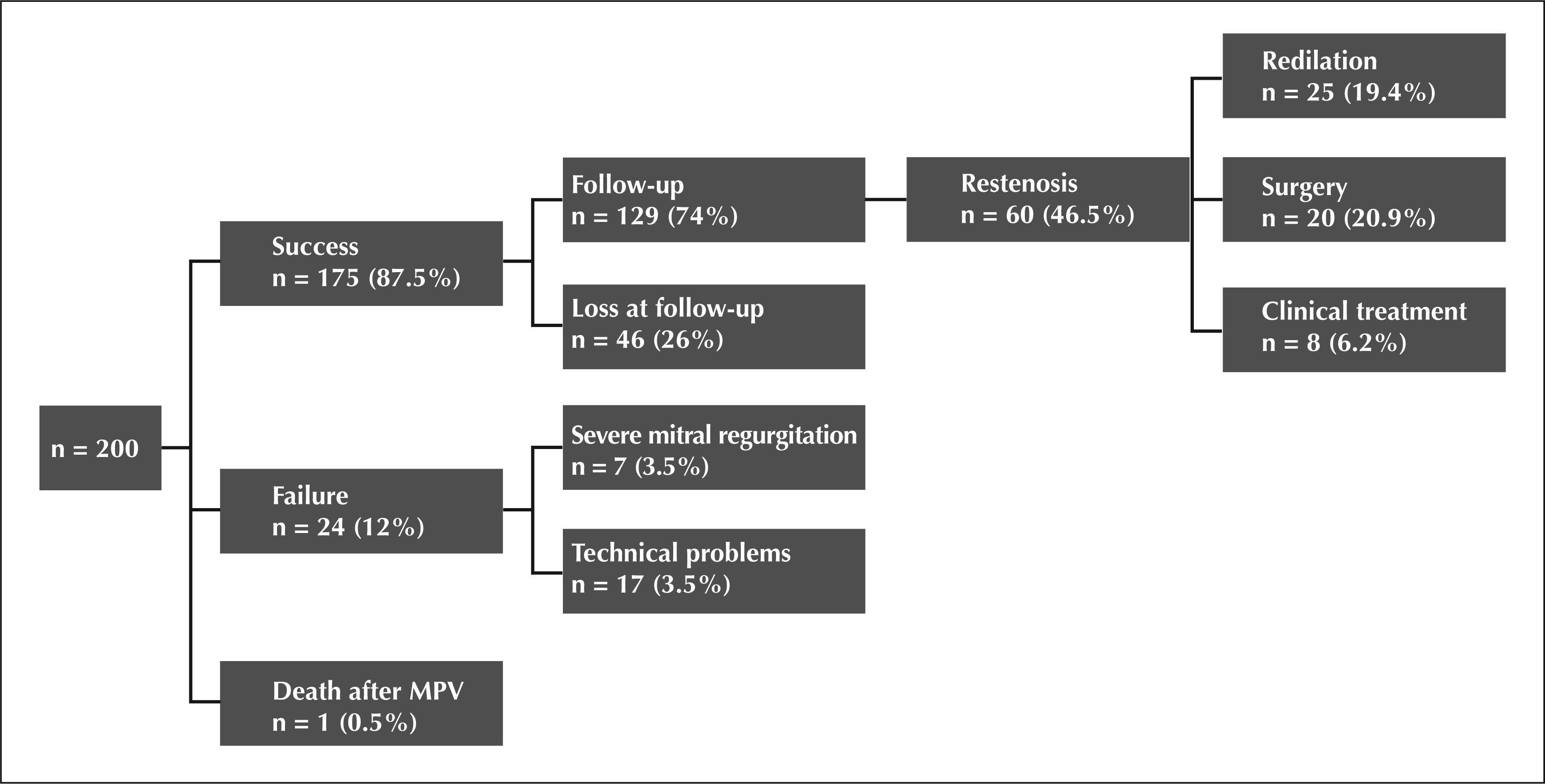
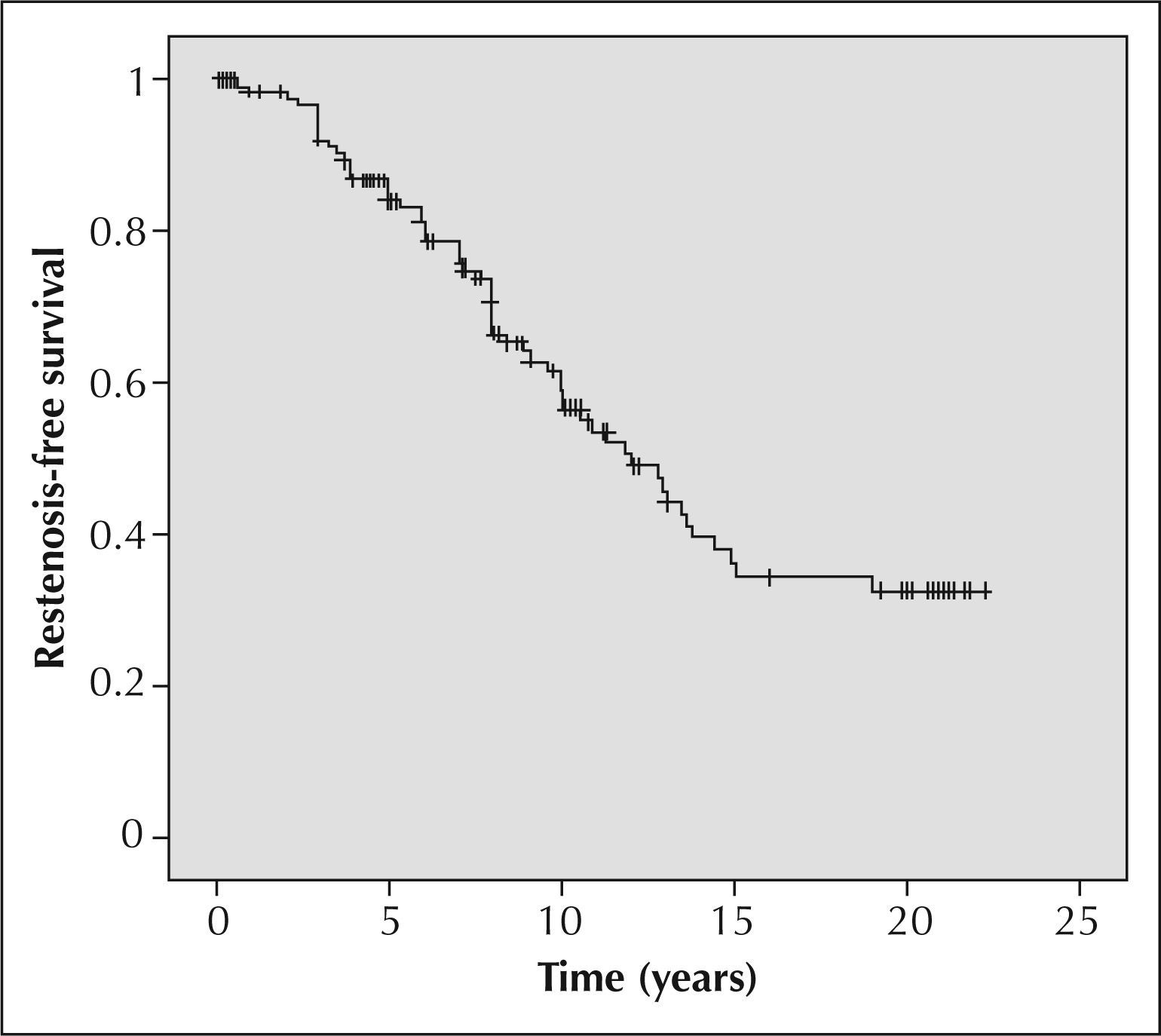
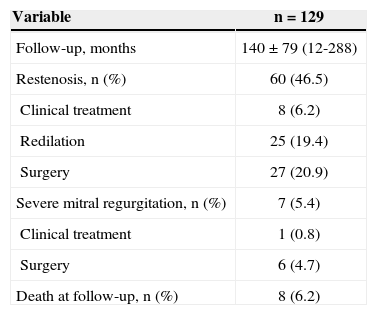
ResultsMean age was 32 ± 12 years; 86.5% were female and 80.5% were in New York Heart Association functional class III or IV. Mean Wilkins score was 7.6 ± 1.2 and procedure success was observed in 87.5% (175/200) of the patients. During follow-up, 129 patients (74%) were followed up for 140 ± 79 months. Restenosis was observed after the first procedure in 46.5% (60/129) patients and a second percutaneous balloon mitral valvotomy was performed in 25 patients, a third one in 4 patients and a fourth one in 1 patient. The probability of being restenosis-free was 85% at 5 years, 60% at 10 years and 36% at 20 years. Left atrial diameter (P = 0.034), and preoperative (P = 0.013) and postoperative (P = 0.038) transvalvar gradient were predictors of restenosis.
ConclusionsIn a very late clinical follow-up, percutaneous balloon mitral valvotomy provided long-lasting results in over one-third of the patients and showed that repeated procedures may be performed safely in selected patients. The identification of restenosis predictors is useful for patient selection.
Evolução Muito Tardia daValvotomia Percutânea por Balão na Estenose Mitral Grave
IntroduçãoA valvotomia mitral percutanea por balao e um procedimento seguro e eficaz em pacientes com estenose mitral grave sintomatica selecionados, com resultados imediatos e a longo prazo semelhantes aos da intervencao cirurgica. Este estudo tem o objetivo de descrever os resultados muito tardios das primeiras valvotomias mitrais percutaneas por balao realizadas em nossa instituicao e identificar os fatores preditores de reestenose.
MétodosNo periodo de 1987 a 1991, 200 pacientes consecutivos foram submetidos a valvotomia mitral percutanea por balao. Avaliacoes clinica e ecocardiografica foram realizadas antes do procedimento, 48 horas apos e, entao, anualmente.
ResultadosA media de idade foi de 32+12 anos, 86,5% eram do sexo feminino e 80,5% encontravam-se em classe funcional III ou IV da New York Heart Association. A media do escore de Wilkins foi de 7,6+1,2 e o sucesso do procedimento ocorreu em 87,5% (175/200) dos pacientes. Durante o seguimento, foram acompanhados 129 pacientes (74%) por 140+79 meses. Reestenose apos o primeiro procedimento ocorreu em 46,5% (60/129) dos pacientes, sendo realizada uma segunda valvotomia mitral percutanea por balao em 25 pacientes, uma terceira em 4 pacientes, e uma quarta em 1 paciente. Em cinco anos, a probabilidade livre de reestenose foi de 85%, em 10 anos foi de 60% e em 20 anos, de 36%. O diametro do atrio esquerdo (P=0,034) e o gradiente transvalvar mitral tanto pre (P=0,013) como pos-procedimento (P=0,038) foram preditores de reestenose.
ConclusõesEm seguimento clínico muito tardio, a valvotomia mitral percutânea por balão mostrou que os resultados são duradouros em mais de um terço dos pacientes e que a repetição do procedimento pode ser realizada com segurança em pacientes selecionados. A identificação dos preditores de reestenose é útil para guiar a seleção de casos para o procedimento.
Percutaneous mitral valvotomy with balloon catheter was first described in 1984 by Inoue et al. 1 as an option for treating patients with severe mitral stenosis. In 1986, Al Zaibag et al. 2 started using the double balloon technique for the transseptal route, and McKay et al. 3 and Palacios et al. 4 simplified the technique by performing only a septal puncture and subsequent dilation of the orifice to accommodate the passage of the two balloons.
Currently, percutaneous mitral valvotomy is considered to be the method of choice in the treatment of mitral stenosis. 5,6 When compared with surgical mitral commissurotomy, mitral balloon valvotomy presents similar or higher success rates; 7,8 the restenosis rates are equivalent to that of conventional surgical treatment. 8
The techniques available for mitral balloon angioplasty include the conventional double balloon, 9,10 which was most frequently used in the past; the Cribier metal commissurotome; 10,11 the double balloon with single guidewire approach (MultiTrack); 10,12,13 and the Inoue balloon, 1,9,10 which is currently the most frequently used device. This technique has some advantages compared to the double-balloon technique, since it requires a shorter procedural time and is simpler. The Inoue balloon procedure may be performed by a single surgeon and provides a more stable positioning of the balloon in the mitral annulus. It has been demonstrated that the post-valvotomy mitral valve area is similar regardless of the technique used. 14−16
When assessing a patient with mitral stenosis, the following factors must be considered to indicate the procedure: the New York Heart Association (NYHA) functional class; the mitral valve area; the mitral valve anatomy, which is determined by the echocardiographic score proposed by Wilkins et al.; 17 and the associated valve lesions. The following factors may promote better outcomes: young patients, valve anatomy with Wilkins echocardiographic score ≤ 8 points, sinus rhythm, absence of mitral regurgitation prior to the procedure and prior surgical commissurotomy.
The aim of this study was to evaluate the immediate and long-term results of the first 200 percutaneous mitral balloon valvotomies performed at this institution. The baseline characteristics of the patients, the restenosis predictors, and the need for new interventions were also assessed.
METHODSThis observational, longitudinal and retrospective study represents a cohort of 200 consecutive patients with mitral stenosis submitted to percutaneous mitral balloon valvotomy at this institution from August 1987 to July 1991. Early and late outcomes and predictive factors of restenosis were evaluated.
The patients who underwent percutaneous mitral valvotomy were symptomatic, with a mitral valve area ≤ 1cm 2 and favourable anatomy according to Wilkins echocardiographic score.
Contraindications to the procedure included patients with mobile thrombus or at-risk positions (septum or mitral annulus) in the left atrium, associated mitral regurgitation ≥ 2/4+ according to the classification of Sellers et al.,18 or other valve or coronary diseases or congenital heart diseases associated with surgical indication.
DefinitionsSuccessful procedure: obtaining final mitral valve area ≥ 1.5cm2 with no regurgitation and when present, < 2/4+.
Failure: procedural interruption due to technical difficulties, cardiac tamponade, or severe mitral regurgitation that required surgical intervention.
Echocardiographic restenosis: mitral valve area assessed at echocardiography by planimetry and/or pressure half-time < 1.5cm 2 and/or loss ≥ 50% of the initial gain 19,20 at late follow-up.
Clinical restenosis: symptom recurrence with worsening of functional class confirmed by echocardiography.
Clinical follow-upMedical consultation 30 days after the procedure was performed in patients with procedural success, followed by annual assessments. Symptom onset during followup was indicative of the need for earlier revaluations. Transthoracic echocardiography was recorded 48 hours after the procedure and annually with electrocardiograms and chest X-rays. The indication for a new intervention was based on the presence of clinical restenosis at the echocardiography, with observation of the same indication criteria used for the first procedure.
Statistical analysisThe Statistical Package for Social Sciences (SPSS) software was used for statistical analysis. Values were expressed as mean ± standard deviation. The variation of the mitral valve area mean and maximum diastolic gradients, the left atrial diameter, and the ejection fraction of the left ventricle were evaluated by Student’s t-test. The restenosis-free probabilities during the study were analysed by Kaplan-Meier curves. The Cox regression model was used to identify predictors of restenosis. P-values < 0.05 were considered to be statistically significant.
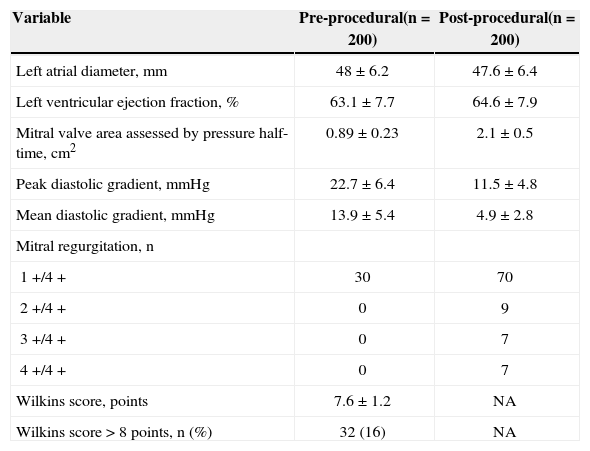
RESULTSPatient characteristics are described in Table 1. The mean age of the patients was 32 ± 12 years, and 173 (86.5%) were females. A total of 39 patients (19%) were classified as NYHA functional class II, and 161 patients (80.5%) were classified as functional class III or IV. Atrial fibrillation was present in eight patients (4%), and five (2.5%) underwent previous surgical commissurotomy. The conventional double balloon technique was applied in 198 patients (99%), and the Inoue technique was used in only two patients (1%). When evaluating the pre-procedural echocardiographic characteristics (Table 2), the mean Wilkins score was 7.6±1.2 points, and only 32 patients (16%) had a score > 8 points. The mean left atrial diameter was 48±6.2mm, the mean ejection fraction of the left ventricle was 63.1±7.7%, the previous mitral valve area measured by pressure half-time corresponded to 0.89±0.23cm 2, and the peak and mean valvular gradients were 22.7±6.4mmHg and 13.9±5.4mmHg, respectively. A total of 30 (15%) patients experienced pre-procedural mitral regurgitation.
Patients’ Clinical Characteristics
| Variable | n = 200 |
|---|---|
| Age, years | 32 ± 12 |
| Female gender, n (%) | 173 (86.5) |
| Sinus rhythm, n (%) | 192 (96) |
| NYHA FC, n (%) | |
| II | 39 (19.5) |
| III or IV | 161 (80.5) |
| Pregnant patients, n (%) | 14 (7) |
| Previous commissurotomy, n (%) | 5 (2.5) |
NYHA FC = New York Heart Association Functional Class.
Pre- and Post-procedural Echocardiographic Characteristics
| Variable | Pre-procedural(n = 200) | Post-procedural(n = 200) |
|---|---|---|
| Left atrial diameter, mm | 48 ± 6.2 | 47.6 ± 6.4 |
| Left ventricular ejection fraction, % | 63.1 ± 7.7 | 64.6 ± 7.9 |
| Mitral valve area assessed by pressure half-time, cm2 | 0.89 ± 0.23 | 2.1 ± 0.5 |
| Peak diastolic gradient, mmHg | 22.7 ± 6.4 | 11.5 ± 4.8 |
| Mean diastolic gradient, mmHg | 13.9 ± 5.4 | 4.9 ± 2.8 |
| Mitral regurgitation, n | ||
| 1+/4+ | 30 | 70 |
| 2+/4+ | 0 | 9 |
| 3+/4+ | 0 | 7 |
| 4+/4+ | 0 | 7 |
| Wilkins score, points | 7.6 ± 1.2 | NA |
| Wilkins score > 8 points, n (%) | 32 (16) | NA |
n = number of patients; NA = not available.
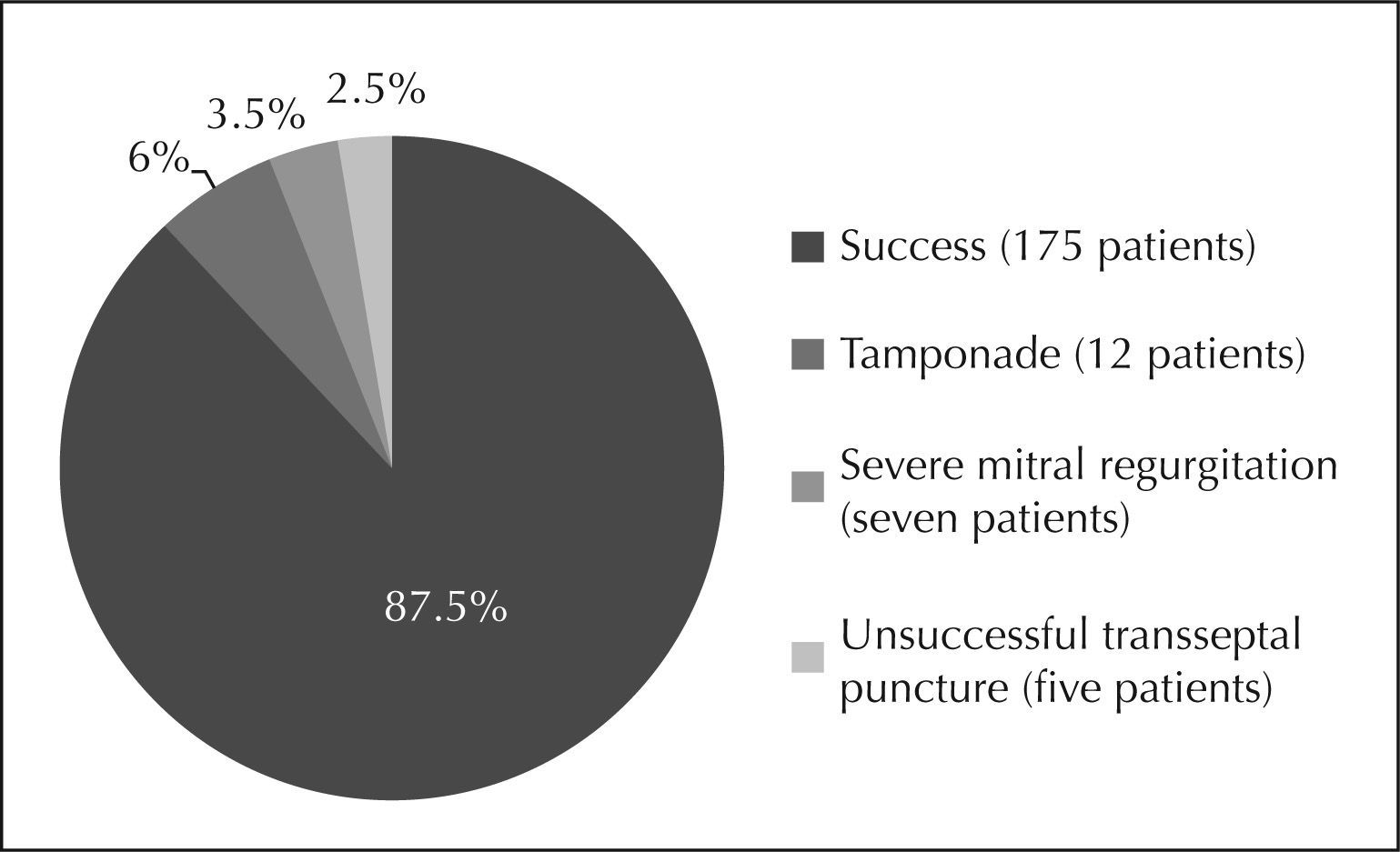
The procedure was successful in 175 patients (87.5%). Failure occurred in 24 patients (12%); in seven (3.5%) patients it was due to severe mitral regurgitation, and in 17 (8.5%) patients it was due to technical problems related to the learning curve (12 cases of cardiac tamponade). It was not possible to perform the transseptal puncture in five patients (Figures 1 and 2). There was one death (0.5%) in the studied population.
The echocardiographic results obtained after the procedure showed a final mitral valve area of 2.1 ± 0.5cm 2, with post-procedural peak and mean diastolic gradients of 11.5 ± 4.8mmHg and 4.9 ± 2.8 mmHg, respectively. The mean left atrial diameter was 47.6 ± 6.4mm. After the procedure, 70 patients experienced mitral regurgitation 1+/4+, and 9 patients experienced mitral regurgitation 2+/4+ (Table 2).
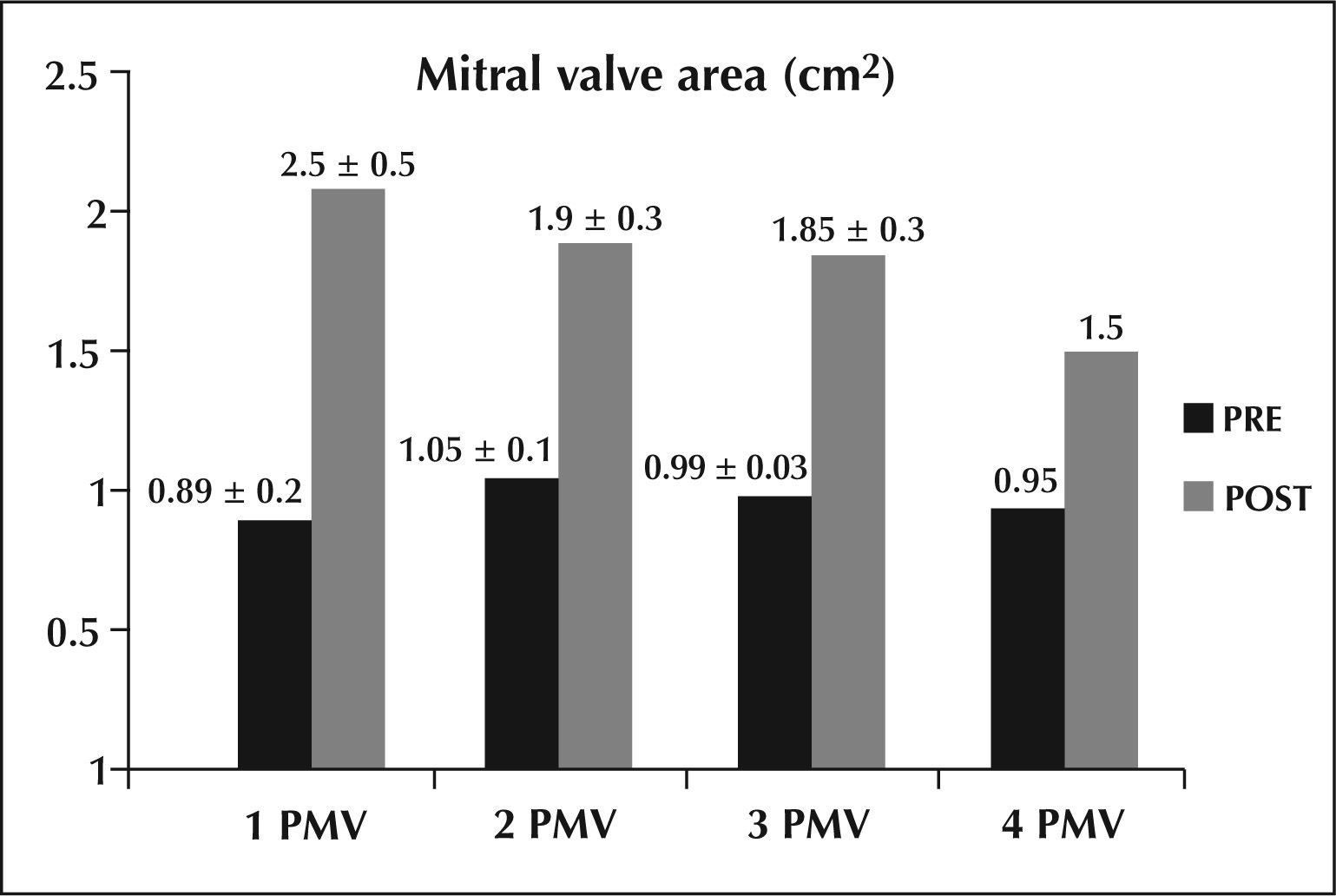
During the follow-up, 129 patients (74%) were followed for a mean time of 140 ± 79 months. Restenosis occurred in 60 patients (46.5%), a second percutaneous balloon mitral valvotomy was performed in 25 patients, a third valvotomy was performed in four patients, and a fourth one was performed in one patient. In the other patients who developed restenosis, 27 required surgery, and eight remained in the clinical follow-up (Table 3). The mitral valve area gain declined progressively after the second, third, and fourth valvotomies, as shown in Figure 3.
The probability that restenosis would not occur was 85% after five years, 60% after ten years, and 36% after 20 years, as shown in the Kaplan-Meier curve (Figure 4).
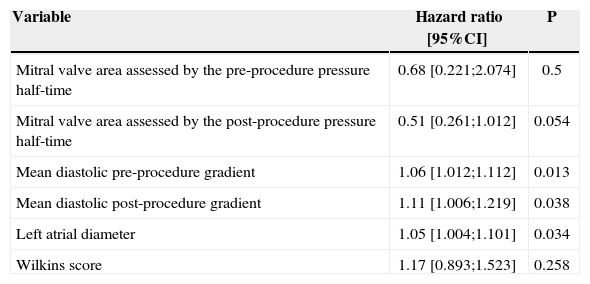
The left atrial diameter (P = 0.034) and pre- and post-procedure mitral transvalvular gradients (P = 0.013 and P = 0.038, respectively) were independent predictors of restenosis, but the Wilkins score (P = 0.258) and the pre- and post-procedure mitral valve areas (P = 0.5 and P = 0.054, respectively) were not independent predictors of restenosis (Table 4).
Restenosis predictors
| Variable | Hazard ratio [95%CI] | P |
|---|---|---|
| Mitral valve area assessed by the pre-procedure pressure half-time | 0.68 [0.221;2.074] | 0.5 |
| Mitral valve area assessed by the post-procedure pressure half-time | 0.51 [0.261;1.012] | 0.054 |
| Mean diastolic pre-procedure gradient | 1.06 [1.012;1.112] | 0.013 |
| Mean diastolic post-procedure gradient | 1.11 [1.006;1.219] | 0.038 |
| Left atrial diameter | 1.05 [1.004;1.101] | 0.034 |
| Wilkins score | 1.17 [0.893;1.523] | 0.258 |
95% CI = 95% confidence interval.
The long-term results of the treatment of mitral stenosis by balloon catheter are well established. Balloon catheter procedures allowed up to 90% of treated patients to remain asymptomatic or mildly symptomatic over a seven-year interval, 8,21 with results similar to surgical treatment 22 but with lower costs. 23 Thus, balloon catheter procedures are considered to be the first choice in patients with favourable anatomy.
In late follow-up studies, 24,25 the study populations differ regarding socioeconomic, ethnic, cultural, age, clinical and echocardiographic characteristics and the aetiology of the mitral disease. 26 Therefore, it is crucial to define therapeutics, estimate risks, and evaluate the prognosis to recognize the determinants of immediate and long-term success.
Patients in the present study had a mean age of 32 years when the procedure was performed. Patients demonstrated a low prevalence of atrial fibrillation, which was similar to the prevalence found in patients from developing countries, 27 but different from that observed in developed countries, in which patients were older and had a higher incidence of arrhythmias. 28,29 This difference can be attributed to different aetiologies of mitral stenosis: rheumatic stenosis is more common in the Brazilian population, and degenerative stenosis is more prevalent in developed countries.
Fawzy et al. 22,30 demonstrated an event-free survival of 79% at ten years and 43% at 15 years in a population with a mean age of 31 years; the survival was even higher in patients with favourable anatomic features (88% at ten years and 66% at 15 years). The following factors were related to a better prognosis: age, postprocedure valve area, and previous valve anatomy. Age is a predictor of restenosis because it is associated with a longer time of disease evolution and, consequently, a higher possibility of valve degeneration. 31
In Brazil, Cardoso et al. 26 demonstrated an event-free survival of 61% at ten years in patients with a mean age of 35 years, with predictors of age, echocardiographic score, and immediate procedural outcome. The magnitude of the long-term benefit is strongly influenced by the immediate outcome, and mitral insufficiency with severe regurgitation is a factor of poor prognosis related to the need for surgery. 31,32
Other factors are related to late success, such as the functional class (NYHA), the mean diastolic gradient, and the presence of atrial fibrillation. 32 However, these factors characterise patients with more severe anatomic features and a lower probability of procedural success. 32 In cases of restenosis, percutaneous mitral valvotomy can be performed as the first choice; 32 there have been reports of patients submitted to up to four procedures with good results. 33
CONCLUSIONIn selected cases, percutaneous balloon mitral valvotomy demonstrates high procedural success and good late follow-up results, with over a third of the patients being restenosis-free. The identification of restenosis predictors is useful to select patients who will benefit from intervention.
CONFLICT OF INTERESTThe authors declare no conflicts of interest.