Although systemic lupus erythematosus (SLE) is more common in adults, when it is diagnosed before the age of 16, it has a worse prognosis. Depressive and anxious symptoms are common in this population but few studies have examined anxiety or its relationship with manifestations of the disease or type of treatment received.
ObjectiveTo determine the frequency of anxious and depressive symptoms in children and adolescents with SLE, as well as their relationship with disease activity and the immunosuppressive treatment used.
MethodsA cross-sectional study in which paediatric patients with SLE from 9 to 17 years of age from a paediatric referral centre in the city of Bogota were included. Each patient was interviewed and immunosuppressive treatment, time to diagnosis and disease activity were recorded. The frequency of depressive and anxious symptoms and quality of life were measured with validated questionnaires. The relationship between anxious or depressive symptoms and disease activity and immunosuppressive treatment was sought.
Results40 patients with a mean age of 14 ± 2 years were interviewed. 52% of cases had active disease. 60% presented scores indicating anxiety and one patient a score suggesting depression. 37% reported suicidal thoughts following the diagnosis of SLE. No relationship was found between disease activity and psychiatric manifestations. Of the different drugs used, only prednisone was associated with higher anxiety symptom scores (p = 0.002).
ConclusionsAnxiety was more prevalent than depression in patients with paediatric SLE. This disorder and the use of corticosteroids were factors of vulnerability to manifest psychopathology. Lupus activity is not related to psychiatric symptoms. SLE has a significant impact on the quality of life of patients.
El lupus eritematoso sistémico (LES) es más frecuente en adultos; sin embargo, cuando se diagnostica antes de los 16 años, es de peor pronóstico. Los síntomas depresivos y ansiosos son frecuentes en esta población, pero pocos estudios examinan la ansiedad o su relación con manifestaciones de la enfermedad o el tipo de tratamiento recibido.
ObjetivoDeterminar la frecuencia de aparición de síntomas ansiosos y depresivos en niños y adolescentes con LES, así como su relación con la actividad de la enfermedad y el tratamiento inmunosupresor utilizado.
MétodosEstudio de corte trasversal en el que se incluyó a pacientes pediátricos con LES de 9 a 17 años de un centro de referencia pediátrico de la ciudad de Bogotá. Se entrevistó a cada paciente y se exploraron el tratamiento inmunosupresor, el tiempo hasta el diagnóstico y la actividad de la enfermedad. Se midieron con cuestionarios validados la frecuencia de síntomas depresivos y ansiosos y la calidad de vida. Se buscó la relación entre los síntomas ansiosos o depresivos y la actividad de la enfermedad y el tratamiento inmunosupresor.
ResultadosSe entrevistó a 40 pacientes, con una media de edad de 14 ± 2 años. El 52% de los casos tenían enfermedad activa. El 60% presentó puntuaciones que indicaban ansiedad y 1 paciente, de depresión. El 37% informó de ideas suicidas tras el diagnóstico de enfermedad lúpica. No se encontró relación entre la actividad de la enfermedad y las manifestaciones psiquiátricas. De los diferentes medicamentos utilizados, solo la prednisona se asoció con puntuaciones más altas de síntomas de ansiedad (p = 0,002).
ConclusionesLa ansiedad fue más frecuente que la depresión en los pacientes con LES pediátrico. Este trastorno y la utilización de corticoides fueron factores de vulnerabilidad a sufrir psicopatología. La actividad lúpica no se relaciona con síntomas psiquiátricos. El LES tiene un gran impacto en la calidad de vida de los pacientes.
Systemic lupus erythematosus (SLE) is a multisystemic inflammatory autoimmune disease of unknown aetiology, characterised by the production of a range of antibodies and deposition of complement-fixing immune complexes, which results in inflammation and tissue damage.1 SLE is most common in adults; just 15–20% of cases are diagnosed before 16 years of age, and the early onset of the disease has a worse prognosis.2
Depressive and anxious symptoms associated with SLE are common in the paediatric population. Most studies have focussed on depressive symptoms3, while very few have examined the anxiety that these patients can experience4,5 and its impact on quality of life, the manifestations of the disease itself or the type of treatment received.
The objective of this study is to determine the frequency of onset of anxious and depressive symptoms in children and adolescents with SLE, and to explore the relationship of these symptoms with disease activity and the immunosuppressive treatment used.
Material and methodsA cross-sectional study was designed in patients treated by the Psychiatry Department of the Fundación Hospital Pediátrico de la Misericordia [Misericordia Children's Hospital Foundation], Universidad Nacional de Colombia [National University of Colombia] (Bogotá, Colombia). Patient between 9 and 17 years of age diagnosed with SLE and in follow-up with the hospital's Paediatric Rheumatology Department were enrolled. Patient with cognitive disabilities and those less than one month from diagnosis were excluded, as were those who did not assent or whose guardians did not consent to their participation.
Medical records were used to obtain basic demographic data such as age and gender, time since diagnosis of the disease (SLE), most recent pharmacological treatment plan offered by the Rheumatology Department and type of organ involvement. The Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) was used to measure disease activity at the most recent assessment by the treating rheumatologist. This scale has adequate construct validity, performance similar to other scales and is sensitive to change. It is the shortest of the SLE activity scales, with just 24 items, and is widely used in clinical practice and research studies. The cut-off point for disease activity was defined as >5.6
Presence of anxious and depressive symptoms and quality of life were reported using specialised questionnaires, followed by clinical interviews with patients and family members conducted by a psychiatrist. The Children's Depression Inventory (CDI), created by Kovacs for children 8-17 years of age, was used to detect depressive symptoms. It consists of 27 items (cognitive, emotional and behavioural), each with 3 options. The CDI covers 5 dimensions of depression in children and adolescents: dysphoric mood; "acting out"; loss of personal and social interests; negative self-concept and somatic symptoms. It is scored from 0 to 54; 19 is generally accepted as a cut-off point.7
The Screen for Child Anxiety Related Disorders (SCARED) was used to describe anxiety. It consists of 41 items, for children 9–18 years of age. Its 5 dimensions are based on the DSM-IV criteria: generalised anxiety disorder, separation anxiety disorder, social phobia, school phobia and somatisation/pain. Each item has 3 statements, with a total score from 0 to 82 and a cut-off point of ≥25 points.8
Finally, the Paediatric Quality of Life Enjoyment and Satisfaction Questionnaire (PQ-LES-Q) was used to explore quality of life. This 15-question scale assesses attitude with regard to general health, well-being and the patient's feelings about their life. It can be self-administered, asks about the last week, giving a score from 1 to 5 (1 being very bad; 5 being very good). It is a qualitative scale and provides a general image of various emotions in disease conditions. This questionnaire was translated in Colombia.9 In brief, its maximum score is 75, which indicates that there are no difficulties. The minimum is 15, which indicates significant distress.
With the data collected, a database was created in Excel and the variables of interest were grouped. This was then imported into the statistics software SPSS for a descriptive analysis, calculating frequencies and percentages for the qualitative variables and measures of central tendency and distribution for the quantitative variables. Once the frequency of depressive and anxious symptoms had been established, an exploratory analysis of each disorder and its relationship with the drug received and disease activity was performed. A p-value of <0.05 was considered significant for each test using Fisher's exact test. This research was approved by the Institutional Research Ethics Committee of Universidad del Bosque [Bosque University] (Document no. 007-2014).
ResultsA total of 41 patients with a diagnosis of SLE were assessed during the period June-December 2014. Just one patient with cognitive disabilities was excluded.
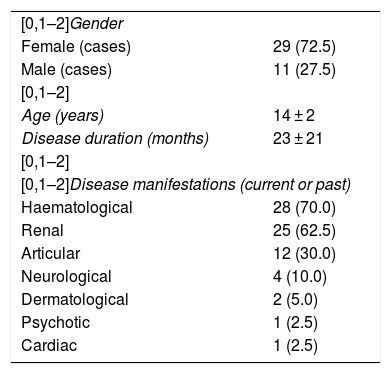
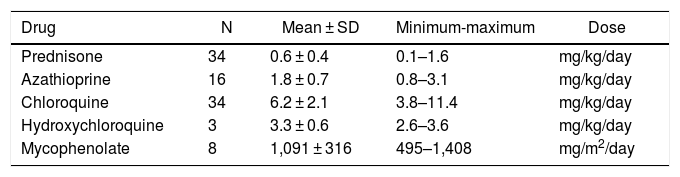
The main demographic and clinical characteristics are summarised in Table 1. It should be noted that age was in the upper part of the range (14 ± 2 years). Gender had the usual distribution, with a female to male ration of 2.6:1. The average time since diagnosis of the disease was 23 ± 21 months. The systems most frequently affected were the haematological (70%), renal (62%) and osteoarticular systems (30%). With regard to lupus activity, the general SLEDAI average was 7.85 ± 8 points and active disease (SLEDAI > 5) was observed in 52% (n = 21) of cases. With regard to treatment received, different types of immunosuppressants were used, the most common being antimalarials (92%) and corticosteroids (85%). The mean, maximum and minimum doses used are shown in Table 2
Clinical characteristics of patients with SLE.
| [0,1–2]Gender | |
| Female (cases) | 29 (72.5) |
| Male (cases) | 11 (27.5) |
| [0,1–2] | |
| Age (years) | 14 ± 2 |
| Disease duration (months) | 23 ± 21 |
| [0,1–2] | |
| [0,1–2]Disease manifestations (current or past) | |
| Haematological | 28 (70.0) |
| Renal | 25 (62.5) |
| Articular | 12 (30.0) |
| Neurological | 4 (10.0) |
| Dermatological | 2 (5.0) |
| Psychotic | 1 (2.5) |
| Cardiac | 1 (2.5) |
Values are expressed in terms of n (%) or mean ± standard deviation.
Drugs and dose administered.
| Drug | N | Mean ± SD | Minimum-maximum | Dose |
|---|---|---|---|---|
| Prednisone | 34 | 0.6 ± 0.4 | 0.1–1.6 | mg/kg/day |
| Azathioprine | 16 | 1.8 ± 0.7 | 0.8–3.1 | mg/kg/day |
| Chloroquine | 34 | 6.2 ± 2.1 | 3.8–11.4 | mg/kg/day |
| Hydroxychloroquine | 3 | 3.3 ± 0.6 | 2.6–3.6 | mg/kg/day |
| Mycophenolate | 8 | 1,091 ± 316 | 495–1,408 | mg/m2/day |
SD: standard deviation.
The mean SCARED score was 26.9 ± 10.35 points, with 24 scoring over 25 points (60%). For depression, the CDI average was 9.3 ± 5.4 points, with just 1 patient scoring over 19 points, which means that 39 patients did not have depressive symptoms. Some 37% (n = 15) reported suicidal ideation from diagnosis of the disease. For quality of life, the PQ-LES-Q returned an average score of 57 ± 7.32 out of 75 (minimum, 46; maximum, 75). The individual analysis reported a tendency toward low scored in questions 3 and 14, which relate to scholastic performance and feelings about oneself; the weighted average of these questions was <3, equivalent to the norm. All other scores on this scale were higher.
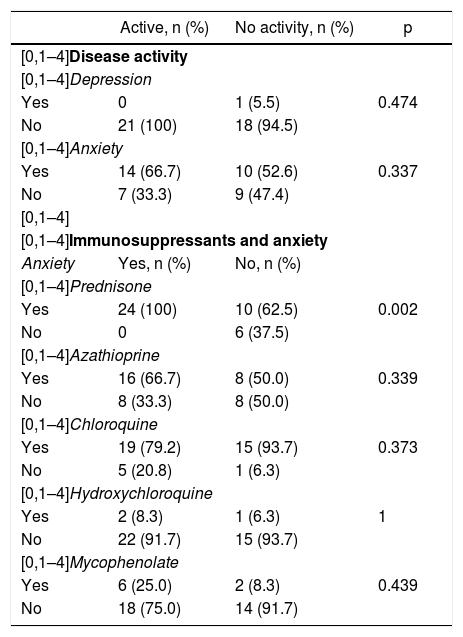
Bivariate analysisThe bivariate analysis of psychiatric manifestations is detailed in Table 3. No association was found between disease activity and the presence of anxious or depressive symptoms. With regard to anxious symptoms and drugs, a significant link was revealed between prednisone use and the presence of anxious symptoms (p = 0.002).
Bivariate analysis of psychiatric manifestations in patients with SLE
| Active, n (%) | No activity, n (%) | p | |
|---|---|---|---|
| [0,1–4]Disease activity | |||
| [0,1–4]Depression | |||
| Yes | 0 | 1 (5.5) | 0.474 |
| No | 21 (100) | 18 (94.5) | |
| [0,1–4]Anxiety | |||
| Yes | 14 (66.7) | 10 (52.6) | 0.337 |
| No | 7 (33.3) | 9 (47.4) | |
| [0,1–4] | |||
| [0,1–4]Immunosuppressants and anxiety | |||
| Anxiety | Yes, n (%) | No, n (%) | |
| [0,1–4]Prednisone | |||
| Yes | 24 (100) | 10 (62.5) | 0.002 |
| No | 0 | 6 (37.5) | |
| [0,1–4]Azathioprine | |||
| Yes | 16 (66.7) | 8 (50.0) | 0.339 |
| No | 8 (33.3) | 8 (50.0) | |
| [0,1–4]Chloroquine | |||
| Yes | 19 (79.2) | 15 (93.7) | 0.373 |
| No | 5 (20.8) | 1 (6.3) | |
| [0,1–4]Hydroxychloroquine | |||
| Yes | 2 (8.3) | 1 (6.3) | 1 |
| No | 22 (91.7) | 15 (93.7) | |
| [0,1–4]Mycophenolate | |||
| Yes | 6 (25.0) | 2 (8.3) | 0.439 |
| No | 18 (75.0) | 14 (91.7) | |
This study reveals a high frequency of anxious symptoms in patients with SLE. These results differ from those published previously by our group, which reported prevalences of anxiety and depression of 53% and 37% of such patients in a 2007-2013 cohort at the same site.10 This difference can be explained by the fact that this study used age-specific tools to collect symptoms, which were then confirmed in a specialist psychiatric interview. It is worth noting that these scales have not yet been validated in our country, but they are used very frequently in our clinical practice to study these symptoms in other populations. It is possible that the previous studies reflect the significant emphasis that adult psychiatry places on the diagnosis of depression. In child psychiatry practice, this emphasis is notably less. In recent years, reports have indicated that anxious symptoms are more common than depressive symptoms. Knight et al.5 found rates of anxiety of 22%, versus 20% for depression. These data differ from those published previously, which had higher rates of depression (15-55%) than anxiety (15–20%).11,12
In this study, the most common form of organ involvement in SLE was haematological and the least common was psychosis; just one case had a history of psychotic disorder as part of the evolution of their disease. These data contrast with the work by Lim et al.,13 who found that psychotic symptoms, specifically hallucinations, were the most common psychiatric symptom in adolescents with SLE. That research was carried out by means of a retrospective analysis of patients' medical records, unlike our study, which was conducted directly with patients. Moreover, in our experience, psychosis in children and adolescents is a very rare event in patients medicated with corticosteroids, one of the most commonly used treatment in SLE and other paediatric diseases.
Patients with SLE have always been considered a population a greater risk of suicide. During this study, the frequency of suicidal ideation from diagnosis of the disease was assessed, observing a high rate of suicidal ideation, although none of the cases had a history of suicidal behaviour. These figures are slightly higher than those reported previously. Nassi et al.14 found a prevalence of suicidal ideation of 19% in the paediatric population with SLE. Lim13 reported suicidal ideation in 18 (34%) out of 53 paediatric patients with SLE, while Knight's group5 reported suicidal ideation in 14% of a sample of 40 patients with SLE. At the other extreme, Kohut11 recorded no suicidal ideation in 38 patients with SLE. These data indicate that the risk of suicide is latent in this population and needs to be explored. As SLE is a chronic disease with which anxiety is associated, suicidal ideation is a crucial risk, since it may be precipitated by this combination.
Quality of life measured with the PQ-LES-Q revealed a tendency toward low score, with most patients falling between the 5th and 25th percentiles. In an individual analysis, a tendency toward low scores was observed in 2 items in this scale, the first of which relates to low scholastic performance. There are two hypotheses that might explain this result; first, high rates of absenteeism as a consequence of the disease; and second, an additional disinclination to attend classes due to changes in appearance caused by the drug, resulting in taunting by classmates. These changes have a direct impact on the patient's feelings about themself, which is the second item in the scale with low scores. Similar studies that have analysed quality of life in patients with SLE have reported similar results, and consider changes to a patient's appearance to negatively impact their quality of life.5
In this study, the vast majority of patients had active disease, but in spite of this, no link whatsoever was found with psychiatric manifestations. Neither is such a link clear in the literature, with many authors reporting ambiguous conclusions.11,15,16
With regard to the type of treatment used to treat SLE and the presence of anxiety or depression, a positive correlation was found between corticosteroid use and the presence of anxiety. The link may be due to corticosteroids being required during flare-ups of the disease, leading the adolescent to suffer damage to their physical appearance linked to the drug. Kohut11 recorded an association between high doses of corticosteroids (> 0.4 mg/kg/day) and increased depressive symptoms. It is important to continue to explore this relationship in larger groups with different drug doses.
ConclusionsAnxiety is the predominant psychopathology in children and adolescents with SLE due to their chronic disease status, the use of steroids and the changes in bodily appearance these cause. The results demonstrate that in this group of patients, the treatment of psychopathological changes in order to improve quality of life and thus facilitate compliance with SLE-related interventions is justified. It was also revealed that the SLE activity index (SLEDAI) is not necessarily indicative of the presence or absence of psychopathology.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Hernández C, Díaz A, Vásquez R. Psicopatología en lupus eritematoso sistémico pediátrico. Rev Colomb Psiquiat. 2021;50:29–33.