A case is presented on a 47-year-old man with chronic lead poisoning with typical symptoms after 5 years of occupational exposure. He consulted for generalized muscle weakness, early dysphagia, cephaloparesia, and paresthesias in upper and lower limbs. He also had atrophy and decreased proximal muscle strength (deltoid and medial vast) and in both flexor and extensor muscles of the neck. He had a history of high blood lead levels and peripheral neuropathy documented by electromyography. In addition to the diagnosis of lead poisoning, inflammatory myopathy was confirmed based on muscle enzyme elevation, muscular inflammation in magnetic resonance imaging, and typical findings in a muscle biopsy. To the best of our knowledge, this is the first report where both conditions are documented in one patient.
Se reporta el caso de un hombre de 47 años con intoxicación crónica por plomo, secundaria a exposición laboral de 5 años, con sintomatología típica de saturnismo. Consultó por debilidad muscular generalizada, disfagia y parestesias en extremidades. Se documentaron altos niveles de plomo en sangre, asociados a neuropatía periférica, confirmada por electromiografía, y disminución de la fuerza muscular en cintura escapular y pélvica (deltoides y vasto medial), así como atrofia de músculos del cuello (flexores y extensores) manifestada como cefaloparesia. Adicional al cuadro de saturnismo se diagnosticó miopatía inflamatoria con base en la elevación de enzimas musculares, miositis por resonancia magnética nuclear y biopsia muscular compatible, siendo, hasta donde se sabe, el primer reporte conocido de la coexistencia de estas 2 enfermedades.
Exposure to lead, as a result of the industrial activity and its massive use in household products, emerges as one of the problems of higher prevalence and impact on public health.1–4 Currently, the main sources of exposure are circumscribed to an occupational setting (manufacturing of paint, glass, ceramics, among others) and in the environment they are derived from the combustion of gasoline, industrial emissions and food contamination; both sources can generate toxicity in human beings.5 Patients with lead poisoning may have clinical manifestations of acute or late onset; in adults, the clinics becomes more evident when the lead serum levels are within moderate or high ranges (between 40 and 80μg/dL), with gastrointestinal symptoms (abdominal pain, vomiting, constipation) being the most frequent.6–8 In individuals with plumbemias exceeding 100μg/dL, serious manifestations such as nephropathy, hepatic necrosis and anemia, and varied neurological manifestations such as peripheral neuropathy, carpal tunnel syndrome and encephalopathy occur.9 Regarding other symptoms, for example musculoskeletal, those which have been more often mentioned in the different case series are: arthralgia (14–28%) and weakness of the extensor muscles of wrists and ankles (13%).10 After an extensive literature search, as far as is known, no clinical articles reporting the simultaneous presence of inflammatory myopathy and peripheral neuropathy in patients with lead poisoning were found.
Case reportA 47-year old-man with chronic lead poisoning secondary to occupational exposure for 5 years, with typical symptoms of saturnism: headache, hyporexia, diffuse abdominal pain and persistent decreased libido despite multiple treatments, among them: BAL dimercaprol, succimer and ethylenediaminetetraacetic acid. He consulted for generalized muscle weakness and paresthesias in upper and lower limbs, associated with high dysphagia for solids and liquids. On physical examination was found decreased muscle strength, symmetrical, with proximal predominance, accompanied by significant atrophy of the deltoid and vastus medialis muscles, as well as of the neck flexors and extensors, with secondary cephaloparesia.
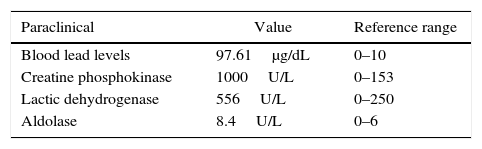
The main findings in the laboratory tests carried out are in Table 1. It drew the attention, clinically, the weakness as cardinal symptom, the inability of the patient to get up from sitting position, not being able to raise his arms above his head and the cephaloparesia; these characteristics compelled to explore causes of weakness of muscle origin. Toxic (no consumption of alcohol, glucocorticoids or lipid lowering agents), endocrine (hormonal and electrolytic profiles without alterations), malignant (normal thoracoabdominal CT scan, digestive endoscopy and colonoscopy; serum and urine immunofixation with no evidence of monoclonal gammopathy) and infectious (negative serologies for bacteria and fungi) causes were ruled out.
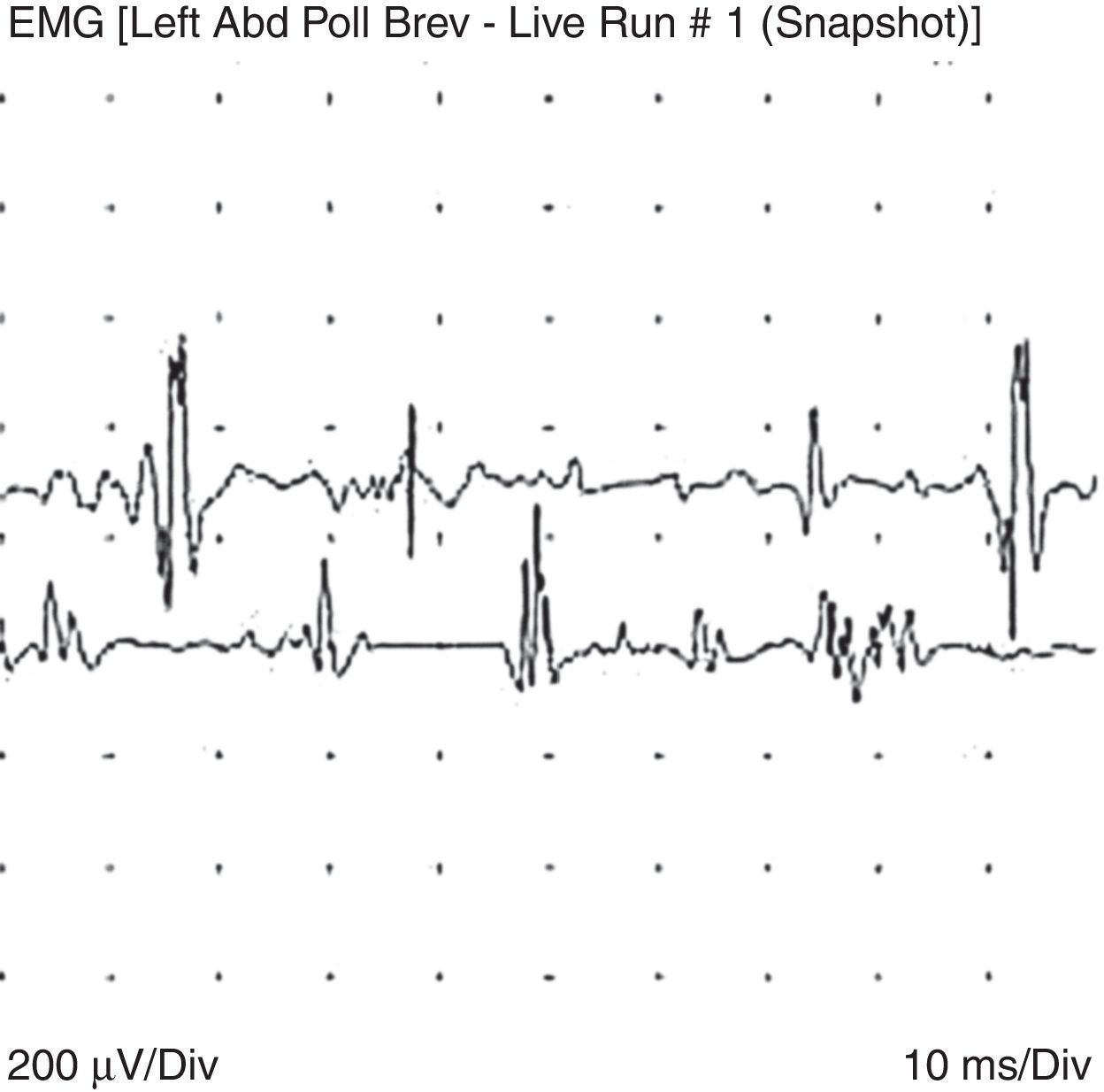
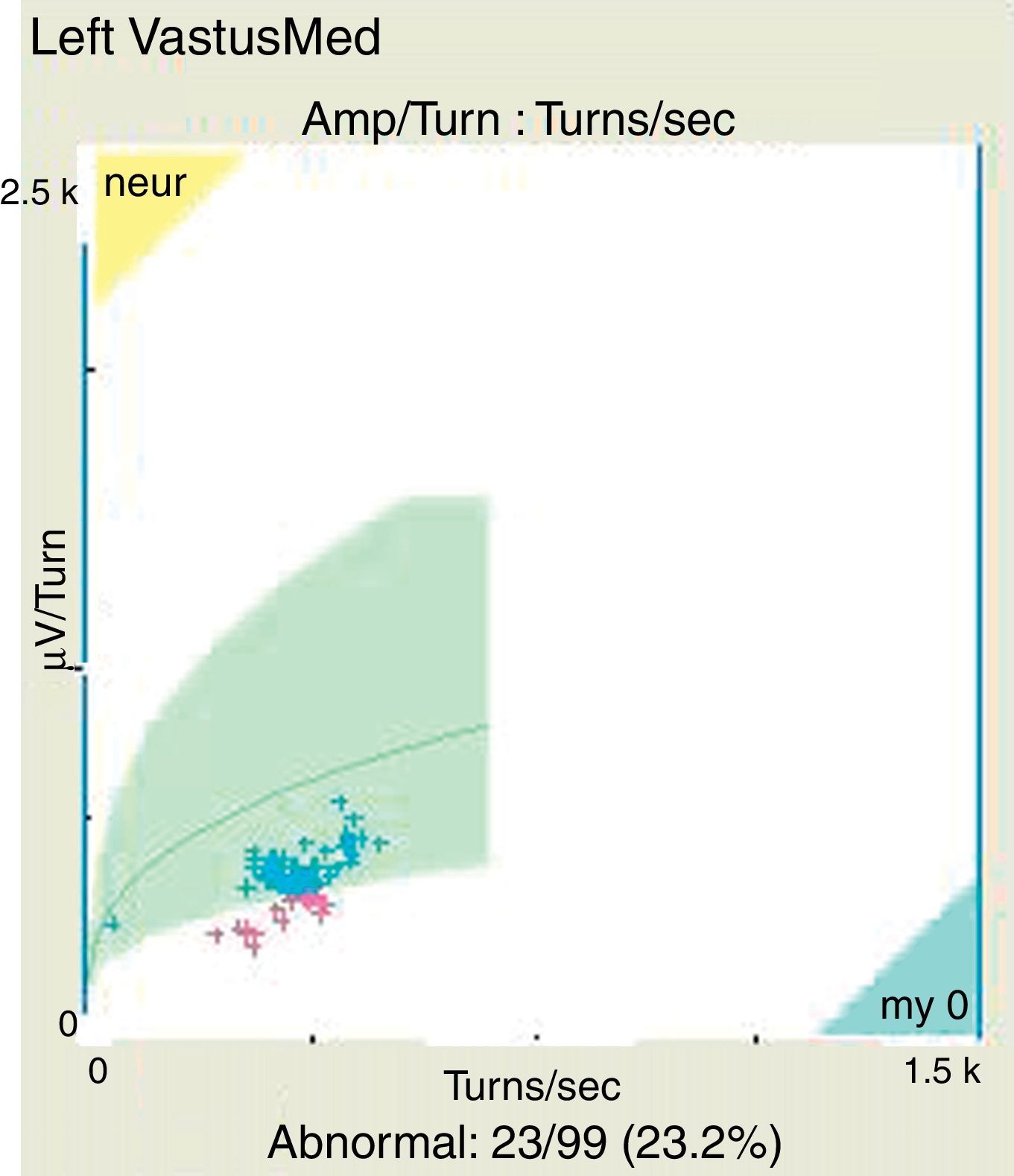
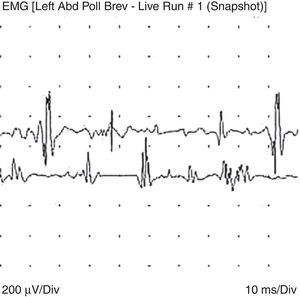
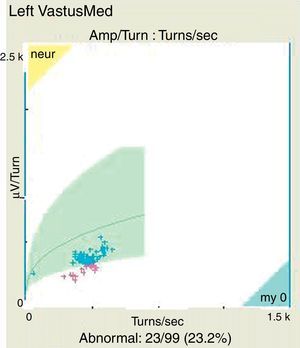
An electromyography was performed as part of the diagnostic process, finding, in addition to the expected neuropathic pattern, polyphasic potentials, early recruitment and membrane irritability, findings highly suggestive of muscle fibers disease (Figs. 1 and 2).
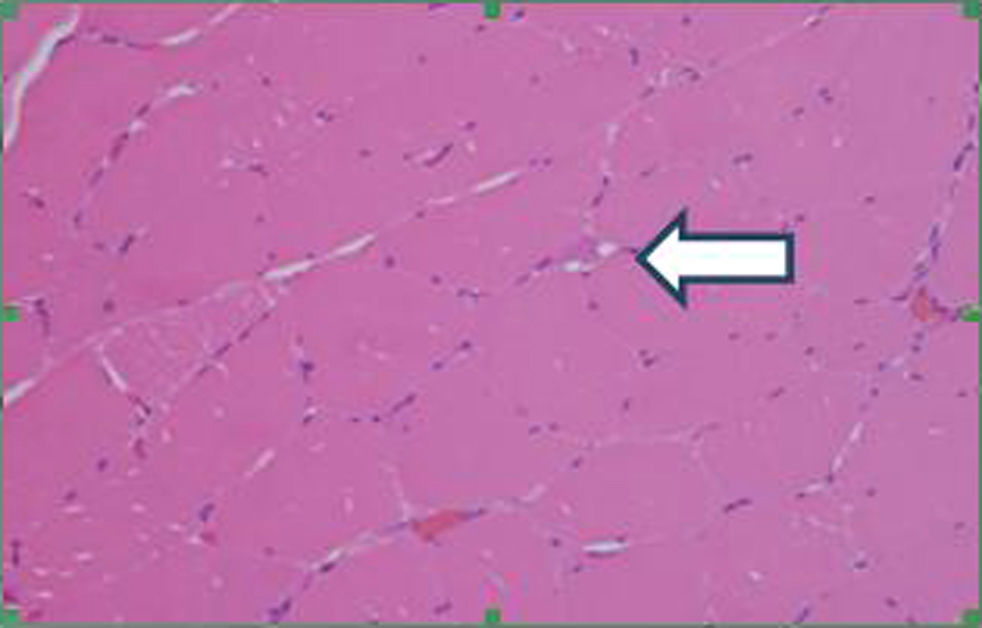
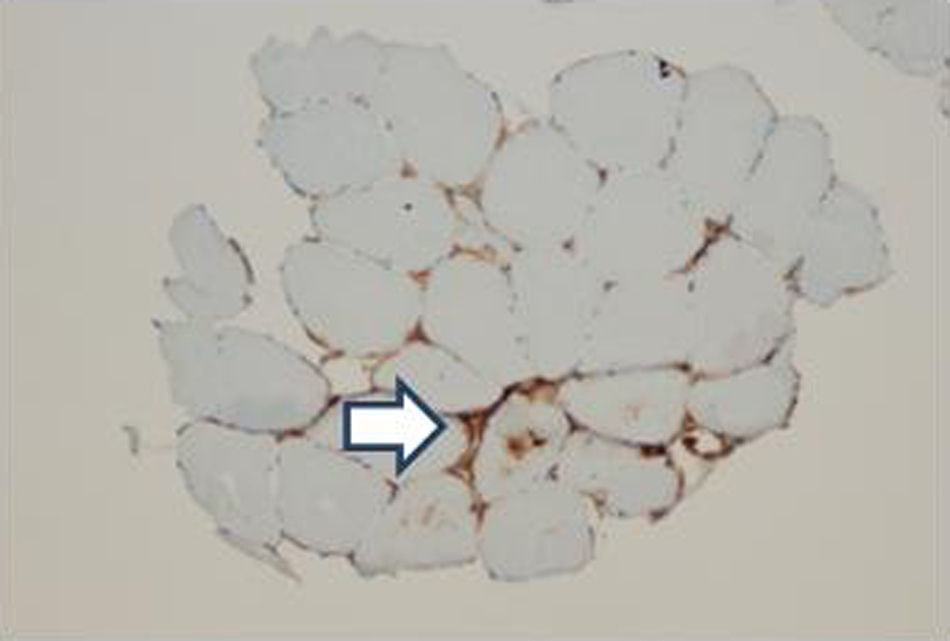
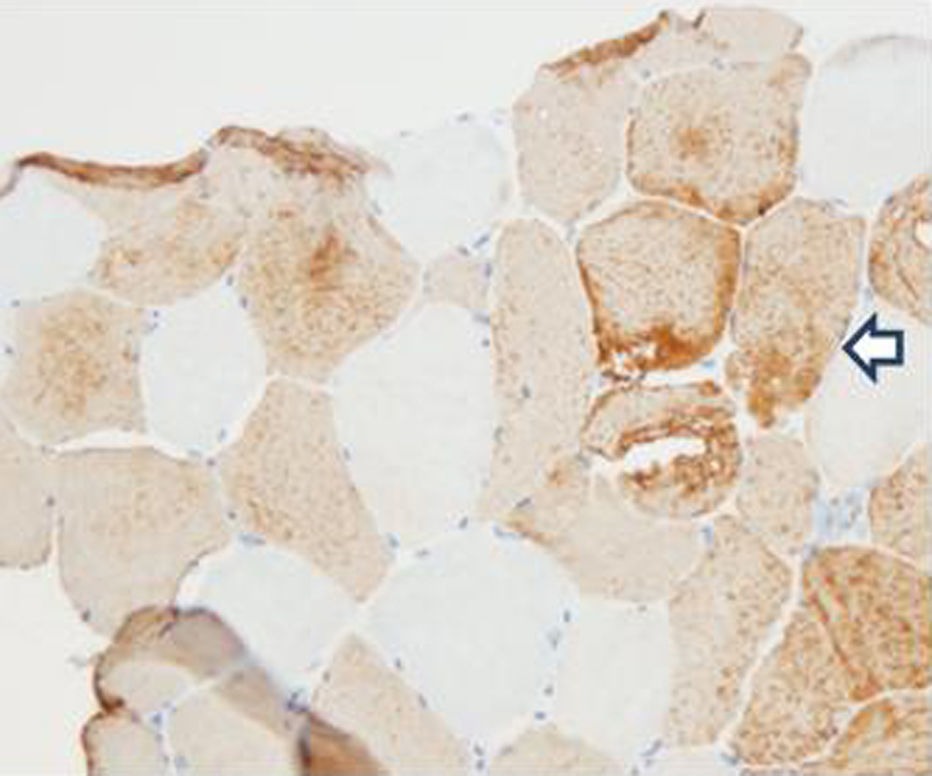
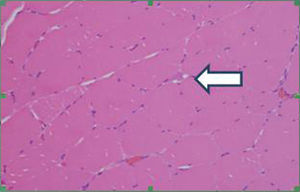
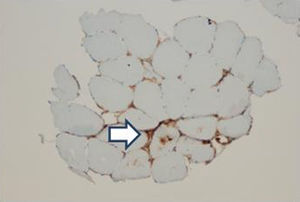
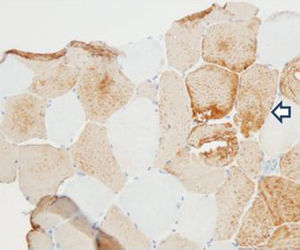
In order to define the degree of muscle atrophy, a nuclear magnetic resonance imaging of the girdle (scapular and pelvic) was performed to the patient, finding predominance of atrophy, but with areas of active myopathy (hyperintensity in the right lateralis vastus until the formation of the lateral retinaculum) (Fig. 3). With these results, it was decided to take the patient to muscle biopsy, confirming the diagnosis of inflammatory myopathy (endomysial commitment and expression of HLA-1) (Figs. 4–6).
Lead poisoning can have a broad spectrum in its clinical presentation and a variable intensity, depending mainly on the serum levels of this metal. A case of concomitance of peripheral neuropathy and polymyositis is presented in this report. As mentioned above, in several series of cases have been reported neuromuscular symptoms such as: peripheral neuropathy, weakness of the extensor muscles, myalgias and arthralgias and carpal tunnel syndrome, among others.10
With regard to the peripheral neuropathy due to lead, it has been described classically as a pure motor disease, predominantly in the arms, especially in the wrist extensors; sensory involvement is very rare despite its predominance in other neuropathies due to heavy metals such as arsenic, mercury or thallium.11 These findings coincide with the reported case; minimal electromyographic changes such as slow motor conduction with slightly reduced compound muscle action potentials are reported in the literature. There are also series reporting findings of polyneuropathy (marginally prolonged distal motor and sensory latencies) and autonomic neuropathy. It is proposed that the traditional motor syndrome seems to be a lead-induced porphyria, and in individuals with chronic intoxication a mild sensory and autonomic polyneuropathy occurs due to a direct neurotoxic effect.11
As mentioned before, after an extensive search without restriction of terms in Scielo, Lilacs, PubMed and Academic Google databases, no association or coexistence between peripheral neuropathy and polymyositis was found in patients with lead poisoning.
Only one report was found in Rhesus monkeys that were exposed to lead acetate before and after birth during 9 years; in histological muscle studies were found signs of myopathy, with increased diameters of the muscle fibers, separated by copious endomysial connective tissue, in addition to hydropic mitochondria and a massively dilated sarcotubular system, with increased deposition of extracellular collagen and nuclear destruction.12
There is one case reported in the literature of a 31 year-old-patient with severe lead poisoning secondary to retained bullet fragments after a shootout, with impact on the left hemithorax and that appeared as proximal muscle weakness 6 weeks after the event, additional to classic symptoms of saturnism and deep tendon areflexia. In this case, the muscle enzymes were normal and the studies of motor nerve conduction revealed generalized compound muscle action potentials with no changes in the nerve conduction, compatible with axonopathy without demyelination. Similar cases of acute proximal muscle weakness due to this traumatic etiology, where abrupt and massive exposure to this metal prevails, have been described. The abnormal distribution and the loss of selectivity of lead deposition in the distal motor nerves, as well as the presence of a transient thyrotoxicosis, simulating a hyperthyroid myopathy, have been proposed as hypotheses for the genesis.13
ConclusionIn a patient with lead poisoning, with moderate of high serum levels and weakness, the differential diagnosis must be broad, and neurological and muscular causes should be considered. As far as is known, this would be the first case report of concomitance of peripheral neuropathy and polymyositis in a patient with this condition.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingOwn resources.
The work was not supported by any grant or funds from the pharmaceutical industry.
Conflict of interestThe authors declare the absence of conflict of interest regarding the present case report.
Please cite this article as: Becerra L, Colorado M, Molina J, Rivera A, Mesa M, Velásquez-Franco CJ, et al. Coexistencia de neuropatía periférica secundaria a intoxicación crónica por plomo y polimiositis: Reporte de caso. Rev Colomb Reumatol. 2016;23:213–217.