The articular examination is an essential part of the physical examination of the patient with rheumatoid arthritis, since it gives information about the disease status at a given time and allows monitoring of its evolution over time. Despite the importance of the physical examination of the joints, it is noteworthy that there is no standardized technique.
MethodsThis paper aims to frame a discussion on whether standardization of the joint examination is justified, presenting arguments for and against.
Results and discussionThe paper raises several arguments about diagnostic error as a scientific and ethical challenge in establishing the activity of rheumatoid arthritis.
ConclusionIt is time to adopt a standardized physical joint examination technique that allows better assessment of the inflammatory activity status of the disease, avoids risks resultant from poor disease status classification, adheres to ethical principles and does not incur unnecessary expenses. Failure to do so would have scientific, economic, ethical, and public health implications.
El examen articular es una parte fundamental del examen físico del paciente con artritis reumatoide ya que permite obtener información sobre el estado de la enfermedad en un momento determinado, así como monitorizar su evolución en el tiempo. A pesar de la importancia del examen físico de las articulaciones, no existe una técnica estandarizada.
MétodosEste ensayo tiene como objetivo desarrollar una discusión sobre si la estandarización del examen conjunto está justificada, para lo cual se presentan argumentos a favor y en contra.
Resultados y discusiónEl ensayo plantea varios argumentos acerca del error diagnóstico como un desafío científico y ético cuando se trata de establecer la actividad de la artritis reumatoide.
ConclusiónEs el momento de adoptar una técnica de exploración física conjunta y estandarizada, que permita una mejor valoración del estado de actividad inflamatoria de la artritis reumatoide, evite los riesgos derivados de una mala clasificación del estado de la enfermedad, respete los principios éticos y no incurra en gastos innecesarios. Dejar de hacerlo tendría implicaciones científicas, económicas, éticas y de salud pública.
Health professionals who care for patients with rheumatoid arthritis (RA) must not only have a means for determining and assessing disease activity but also be able to follow the evolution of disease and its prognosis over time.1 To determine the activity of the disease, several clinical indices or clinimetry scales are used, whose main component is the physical examination of the joints.2 Additionally, joint examination by counting the number of swollen joints, is a clinical method of quantifying the amount of inflamed synovial tissue.3 The articular examination is an essential part of the physical examination of the patient with rheumatoid arthritis, since it allows obtaining information about the disease status at a given time and also allows monitoring of its evolution over time. It is therefore an important tool in therapeutic decision making. It is also an essential evaluation instrument during clinical trials for assessing the efficacy of drug in developments. Finally, it is important for being able to explain the state of their illness to the patient, and how it is evolving.
Concern about this issue arose in my clinical practice, when I attended a course in another country aimed at joint assessment for a clinical trial in patients with rheumatoid arthritis, in order to determine the activity of the disease and the effect of treatment. After examining a patient, a colleague approached me and with surprise stated: “I cannot believe that these joints are not inflamed in the patient you just examined”, to which I replied that according to the course I had just taken and based on the learnings from that course, the patient did not have swollen joints. From that moment I dedicated to research on the subject, since this topic not only has academic and scientific, but also practical clinical and ethical implications.
In spite of the importance of the physical examination of the joints, it is noteworthy that there is no standardized technique for this examination to be used in communicating and recording findings for clinical indexes or scales necessary to determine disease activity. Consequently, there are frequent controversies among rheumatologists about how to assess whether a joint is inflamed or painful.4 There is great intra- and interobserver variability when examining joints. Despite multiple standardization suggestions, there are no publications on the subject.5
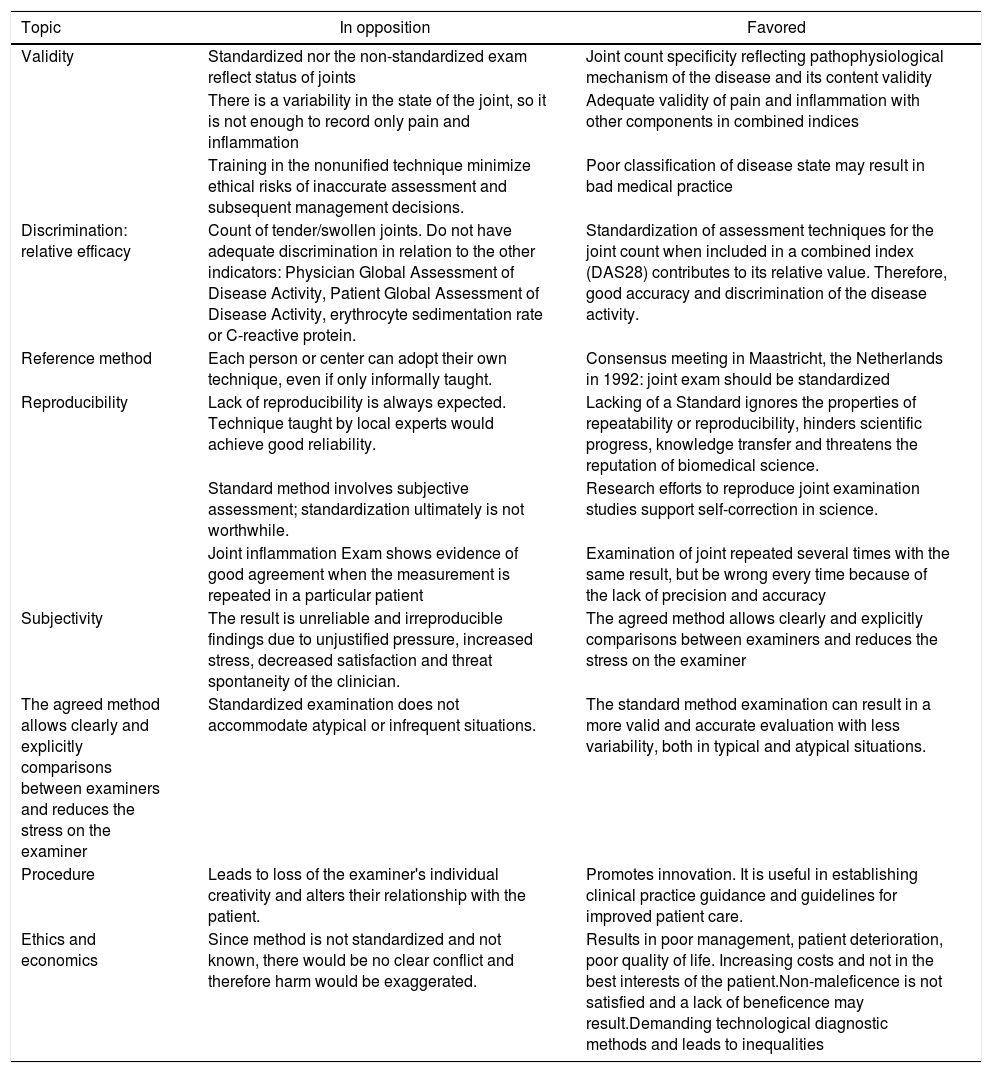
MethodsThis essay aims to frame a discussion about whether standardization of the joint examination is justified, presenting arguments in favor and opposed. It seeks to establish the points of view supporting a position in favor of the need to standardize joint examination technique in order to defining inflammatory joint activity in patients with rheumatoid arthritis (see Table 1).
Arguments for standardization of joint physical examination.
| Topic | In opposition | Favored |
|---|---|---|
| Validity | Standardized nor the non-standardized exam reflect status of joints | Joint count specificity reflecting pathophysiological mechanism of the disease and its content validity |
| There is a variability in the state of the joint, so it is not enough to record only pain and inflammation | Adequate validity of pain and inflammation with other components in combined indices | |
| Training in the nonunified technique minimize ethical risks of inaccurate assessment and subsequent management decisions. | Poor classification of disease state may result in bad medical practice | |
| Discrimination: relative efficacy | Count of tender/swollen joints. Do not have adequate discrimination in relation to the other indicators: Physician Global Assessment of Disease Activity, Patient Global Assessment of Disease Activity, erythrocyte sedimentation rate or C-reactive protein. | Standardization of assessment techniques for the joint count when included in a combined index (DAS28) contributes to its relative value. Therefore, good accuracy and discrimination of the disease activity. |
| Reference method | Each person or center can adopt their own technique, even if only informally taught. | Consensus meeting in Maastricht, the Netherlands in 1992: joint exam should be standardized |
| Reproducibility | Lack of reproducibility is always expected. Technique taught by local experts would achieve good reliability. | Lacking of a Standard ignores the properties of repeatability or reproducibility, hinders scientific progress, knowledge transfer and threatens the reputation of biomedical science. |
| Standard method involves subjective assessment; standardization ultimately is not worthwhile. | Research efforts to reproduce joint examination studies support self-correction in science. | |
| Joint inflammation Exam shows evidence of good agreement when the measurement is repeated in a particular patient | Examination of joint repeated several times with the same result, but be wrong every time because of the lack of precision and accuracy | |
| Subjectivity | The result is unreliable and irreproducible findings due to unjustified pressure, increased stress, decreased satisfaction and threat spontaneity of the clinician. | The agreed method allows clearly and explicitly comparisons between examiners and reduces the stress on the examiner |
| The agreed method allows clearly and explicitly comparisons between examiners and reduces the stress on the examiner | Standardized examination does not accommodate atypical or infrequent situations. | The standard method examination can result in a more valid and accurate evaluation with less variability, both in typical and atypical situations. |
| Procedure | Leads to loss of the examiner's individual creativity and alters their relationship with the patient. | Promotes innovation. It is useful in establishing clinical practice guidance and guidelines for improved patient care. |
| Ethics and economics | Since method is not standardized and not known, there would be no clear conflict and therefore harm would be exaggerated. | Results in poor management, patient deterioration, poor quality of life. Increasing costs and not in the best interests of the patient.Non-maleficence is not satisfied and a lack of beneficence may result.Demanding technological diagnostic methods and leads to inequalities |
As an initial point of discussion is the stance of those who disagree with the need for standardization of the exam, arguing that it is not necessary to ensure adequate validity of their findings. This position argues that neither the standardized nor the non-standardized exam reflect the reality or status of the patients’ joints and, therefore, there would be no difference in assessment. This argument is based on the fact that one patient may have many inflamed joints but little pain, while another may suffer from considerable pain but have few inflamed joints.6 However, both patients may receive identical treatments based on this information, so the detailed examination would not be a useful or necessary tool to differentiate patients from each other.
Additionally, there is a lot of variability in the state of the joint disease, so it is not enough to record only pain and inflammation. Those taking this position point out that the parameters of pain and inflammation (swelling) does not comprehensively reflect the state of the joints, failing to take into account other aspects such as range of motion, functionality, degree of deformity, damage, destruction or the total number of joints.7 Consequently, standardization becomes impracticable.
In spite of the previous arguments, the physical examination of joints has been the main component of the composite indices aimed at determining joint disease activity. The joint examination is given the greatest weight in these measures. It is almost universally accepted that the joint count has a preeminence compared to the other aspects included in the clinimetry scales due to its specificity to reflect the pathophysiological mechanism of the disease and its content validity (that is, it measures what you are trying to measure), which means that it measures the activity of the disease, based on determining what happens in the joints.8 Moreover, even if it is true that the determination of pain and inflammation is not a sufficient criterion for assessing joint status, when added to the other components in the combined indices, adequate validity is achieved in order to discriminate changes in health status.
Those who are against use of a standardized method of joint assessment on physical examination can claim that the definition of joint pain or inflammation has been in long use without any reference method, and that each person or center can adopt their own technique, even if only informally taught. Thus, a technique can be defined among those who work in a center or among people who examine the same patients. However, this contrasts with the consensus meeting held by a group of researchers from around the world (in Maastricht, the Netherlands in 1992),9,10 in order to define a core group of RA activity variables. This group proposed that techniques for measuring these variables (which included pain and inflammation on the joint examination) should be standardized, which would result in a common language and nationally and internationally unified technique.11 Despite this proposal, this standardization has not been developed.5
Some opponents of standardization might argue that in the examination of the joints, some degree of lack of reproducibility is always expected, even when all local examiners are using the same technique. They would say that the definition of a standard is not imperative, and that if continuous education is provided about the method of examination used, with transparency and without barriers or secrets, there should be no great difficulties with reliability.12 They would add that, if one works with the traditional technique, as used and taught by local experts, results would achieve better reliability. Our opinion is that this position, which ignores the properties of repeatability or reproducibility, hinders scientific progress, knowledge transfer and threatens the reputation of biomedical science.13 Here we see that numerous studies have reported variation in the reliability of the joint count between observers and between centers.
People who disagree with a standardized method of joint examination may think that their own method is as objective as the standardized method would be, and that furthermore, even use of a standard method involves subjective assessment, so that the standardization ultimately is not worthwhile.16 It is certainly possible that independent verification of the previous studies of the joint examination based on results from new studies could strengthen the results of past studies of the joint examination and therefore their reproducibility. On the other hand, when the previous results are not confirmed or reinforced, the new results of the reproducibility studies can lead to the generation of new ideas or hypotheses. This avoids the loss of time and resources, and additionally the “wild goose chase” effect can be prevented—meaning that an investigation that is useless and a waste of time because the subject being investigated is irrelevant. A research task whose execution is inordinately complex relative to the value of the outcome or is off target and irrelevant to the outcome of interest.13 An adequate reproducibility of the joint exam is based on the fact that it can verify the results from one professional to another. In summary, research efforts to reproduce joint examination studies support self-correction in science.14
The opponents of a standard method would argue that the diagnosis of the clinical state of joint inflammation shows evidence of good agreement when the measurement is repeated in a particular patient. At this point we agree. However, there are other points against this argument. First, the examination of the joint can be repeated several times with the same result, but be wrong every time because of the lack of precision in the diagnostic criteria for synovial tissue inflammation.15
Second, repeatability (several test results in a patient by the same examiner), may still be associated with poor test accuracy. Third, the evidence shows that inter-observer agreement on joint examination findings in the same patient (reproducibility) is poor.16
Opponents of a standard method express the opinion that the evaluation of joint swelling and joint tender on the physical examination is not easy or simple and that has inevitable sources of intraobserver and interobserver variability, despite using a consensus driven approach.17,18 Moreover, they would affirm that this variability can be reduced with training in the traditional technique and thus minimize ethical risks of inaccurate assessment and subsequent management decisions. From my point of view, this leads to a potential scientific and ethical conflict since not developing a standardization can lead to poor classification of disease state. This lack of skill or competence results in bad medical practice.19
As an illustration, accepted practice is a joint should be examined by palpation of the joint margin, the anatomical site where the synovial membrane inserts.20 The examiner assumes that this point of the joint is clearly defined by the anatomical position, but when it is aberrantly located, the anatomical relationship is distorted, introducing a degree of subjectivity. In contrast to this concept, we consider that the degree of objectivity increases with a standardized examination, which gives less room for improvisation or conjecture. As researchers and knowledge generators, we must resist the paradigm that clinicians should be trained to conduct the joint examination in the traditional way and that it is not important to establish a systematic and objective method.
For some clinicians, the idea of performing a standardized joint examination is counter to usual practice and takes them out of their comfort zone. They regard it as a tedious, laborious and forced exercise, which must be memorized and adopted. The result is unreliable and irreproducible findings due to unjustified pressure, increased stress, decreased satisfaction and threat to the spontaneity of the clinician.17 However, we consider that for those who favor the agreed method, it can represent an adequate evaluation that allows comparisons between examiners and applies the method clearly and explicitly, and in fact reduces the stress on the examiner.18
Another possible argument against the standardized examination is that it does not accommodate atypical or infrequent situations, such as coexistence of joint problems, joint trauma, surgery or nervous system disorders. In fact, standardization results in a more accurate and repeatable examination especially when other conditions affect the joints. The standard method examination can result in a more valid and accurate evaluation with less variability, both in typical and atypical situations.
A consideration of people who disagree with the standardization of the exam is that it leads to a boring, monotonous procedure or that leads to loss of the examiner's individual creativity and alters their relationship with the patient, as it hinders their interaction. We consider on the contrary, that such “creativity” is misplaced in diagnostic assessments such as the joint examination, and that variability should be avoided in order to have repeatable results. The evidence shows that research for methods standardization promotes innovation. Additionally, testing is more efficient and simpler to perform. This in turn can lead to future investigations that result in new processes or procedures.21 In addition, it reduces ambiguity and loss of information. At the same time, it is useful in establishing clinical practice guidance and guidelines for improved patient care. Multiplicity of techniques is avoided and the omission of information is prevented.22 Among high impact benefits, the standard method joint examination enables better and more consistent evaluation and treatment of a high-cost disease such as RA.
Diagnostic error due to poor standardization of examination which fails to account for all of the pertinent joint findings by not applying a valid and reliable technique results in poor management. Consequently, the patient may deteriorate, have a poor quality of life, develop deformities and may even require surgery. From an economic perspective, very expensive erroneous treatments may be applied that otherwise would be avoided, or necessary procedures neglected, which, although expensive, would serve to avoid even more expensive complications. Therefore, as González and Revuelta cite23: “The diagnosis, as a medical act that has profound human repercussions, must include in all its manifestations a clear ethical commitment, in obedience to the Hippocratic dictum: cure when possible, comfort always, and above do no harm”.24 Opponents of the idea of unifying the technique of joint examination can argue that the count of tender or swollen joints has less relative efficacy than other variables of ACR core data set measures (Physician Global Assessment of Disease Activity, Patient Global Assessment of Disease Activity, erythrocyte sedimentation rate or C-reactive protein), for detecting differences between active (Leflunomide) and placebo (methotrexate or placebo) in patients with active RA. In other words, patients who receive the control treatment can show improvement group when the joint count is compared with other individual measures of disease activity.25,26
An example of the concept of the relative efficacy of the components of the combined scales (joint tender and swelling) was supported by results from a clinical study where the change of several measures of disease activity was analyzed by means of DAS28 scale. This was a study of patients treated with placebo or methotrexate versus patients with leflunomide, comparing the baseline state of activity with the post-treatment state.25 There was an improvement in the placebo (control) group of 21.4% in the count of inflamed (swollen) joints, 20.3% in the count of painful joints, 11.7% in the physician global assessment, and 11.6% by patient global assessment. On the other hand, there was a worsening on the pain scale of 20.4% and of function patient self-report of 9.3% and increase in the erythrocyte sedimentation rate of 21.5% in this same group. In other words, the joint count (for pain and inflammation) did not have adequate discrimination in relation to the other indicators. According to the evidence presented, it was considered that standardization of assessment techniques for the joint count would decrease variability among examiners and therefore their ability to discriminate. Another reason that allows us to consider the importance of joint count to discriminate the patient's activity status is that, when included in a combined index such as the disease activity score 28 (DAS28), for example, it contributes to its relative value and, therefore, has shown good accuracy and ability to discrimination of the disease activity.26
An aspect of ethical debate is that, if there is no generally accepted examination method of patients, there is a risk of not correctly diagnosing the status activity of RA, so that appropriate care would not be offered and therefore disrespecting patients’ right to receive an adequate diagnosis and treatment.24 An example illustrating this point from clinical practice is this: an examiner could mistakenly classify a patient with moderate or high activity, based on the erroneous determination of a high number of painful and inflamed joints. This misclassification based on the number of inflamed and painful joints would imply a poor prognosis. Therefore, it would lead doctor to start biological therapies, with a much higher cost than non-biological medicines. In addition, the decision of the correct non-pharmacological treatment such as physiotherapy would be affected. In sum, the management is not in the best interests of the patient.27
The points addressed herein raise on the one hand, scientific, economic and public health challenges, and on the other hand, ethical dilemmas. If the decision is made to treat a patient with a disease that has a good prognosis as if he had a poor prognosis, the degree and type of immunosuppressive therapy subjects that patient to unnecessary risk, such as higher risk of infections. Additionally, more economic resources would be used than necessary. The principle of non-maleficence is not satisfied.28 On the contrary, if a patient with a poor prognosis is treated as if he had a good prognosis, a lack of beneficence results, with worsening of the RA, ultimately resulting in higher economic, human and public costs.
Those who are against standardized assessment could provide counter arguments that since the accuracy and reliability of the traditional method or the one that is intended to be standardized is not known, there would be no clear conflict and therefore putative harm would be exaggerated.
An assertion by the detractors of the standardization of joint examination method would be that with the non-standardized method, the right of patients to adequate and truthful information would not be affected. Our position, on the contrary, is that not using a standardized method can lead to the violation of patients’ right to be well informed.
An important key issue that has to be considered on the lack of a unified and standardized method of joint examination is that may even trigger demand by patients, researchers and health care providers for technological diagnostic methods such as ultrasonography or joint magnetic resonance imaging, which could be expensive and could subject some unnecessary risk to patients. Of equal importance is that magnetic resonance imaging or ultrasound does is not better than clinical examination for disease state assessment or management decisions, compared with clinical examination.29–31 Moreover, this could also lead to inequalities, since not all patients or health systems can afford these examinations, a circumstance that contravenes the principle of opportunity, that in health economics refers to failing to allocate resources to other priorities.22
ConclusionProfessionals, people who are part of the health system and decision makers who care for patients with rheumatoid arthritis, should adopt a standardized method of joint examination and take actions to apply it. It is time to adopt a standardized, unified, valid and reliable joint physical examination technique that allows a better assessment of the inflammatory activity status of the disease, avoids risks resultant from poor disease state classification, adheres to ethical principles and does not to incur unnecessary expenses. Professionals, decision makers, and even the patients should consider the advantages of standardizing the joint exam. Failure to do so would have scientific, economic, ethical and public health implications. I believe that standardization of physical examination is an especially important subject. Discussion and exploration to improve the scientific value of clinical measurement is deeply needed.
Conflicts of interestNone.
We would like to thank Dr. Eric Matteson for his support in reviewing this essay.