Good sleep has a restorative effect at the cellular level and helps maintain the body's homeostasis.
ObjectivesGiven our clinical experiences, we propose that sleep quality should be evaluated in patients with rheumatoid arthritis. Poor sleep quality should be considered as a factor that may impact clinical outcomes in patients with rheumatoid arthritis.
Materials and methodsWe researched medical literature on clinical and physiological pathways associated with sleep quality.
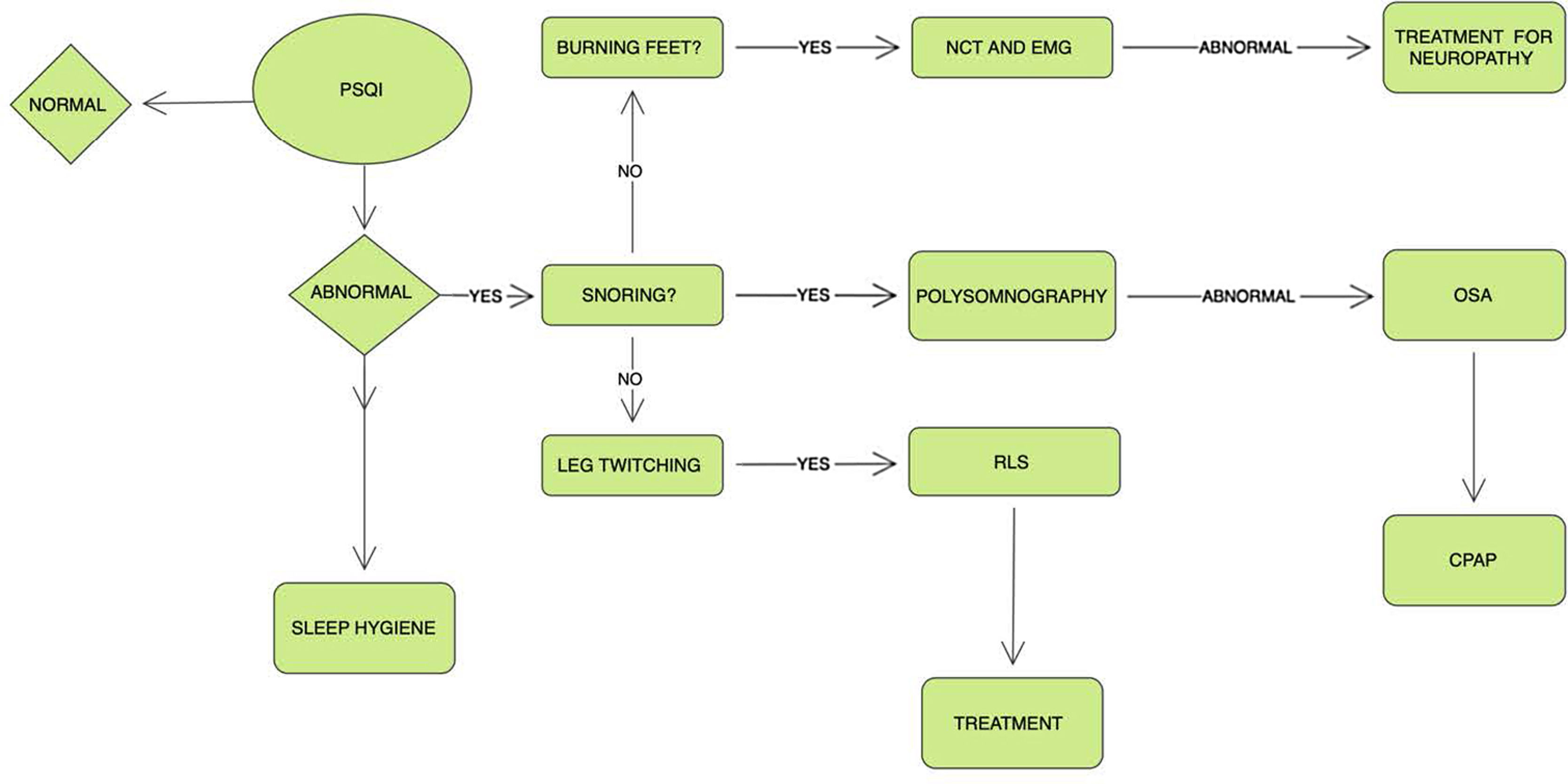
ResultsThere is evidence that interleukin-6 and tumor necrosis factor have a role in inflammatory and immune imbalance as well as in sleep disturbance in patients with rheumatoid arthritis, which leads to the chronic inflammatory process seen in these patients. Most patients with rheumatoid arthritis report sleep problems, be it insomnia or other complaints of non-refreshing sleep. Lack of sleep or poor sleep patterns in these patients further compromise their quality of life. In patients with RA, aetiologies such as restless leg syndrome (RLS), sleep apnoea syndrome, and Temporomandibular Joint Dysfunction (TMJ) syndromes might contribute to sleep disturbances. This lack of restful sleep might limit our goal, as treating physicians, to achieve remission states in these patients.
ConclusionsIt is our opinion that sleep quality evaluation must be addressed, monitored, and treated as part of the management of patients with RA. Bad sleep adds an additional burden to disease activity in patients with RA, besides, it limits patients’ possibility of achieving disease remission.
El buen sueño tiene un efecto restaurador a nivel celular y ayuda a mantener la homeostasis del cuerpo.
ObjetivosDadas nuestras experiencias clínicas, proponemos que la calidad del sueño debe evaluarse en pacientes con artritis reumatoide. La mala calidad del sueño debe considerarse un factor que puede afectar los resultados clínicos en estos pacientes.
Materiales y métodosInvestigamos la literatura médica sobre vías clínicas y fisiológicas asociadas con la calidad del sueño.
ResultadosExiste evidencia de que la interleucina-6 y el factor de necrosis tumoral tienen un papel en el desequilibrio inflamatorio e inmunológico, así como en la alteración del sueño en pacientes con artritis reumatoide, lo que conduce al proceso inflamatorio crónico observado en estos. La mayoría de estos pacientes reportan problemas para dormir. La falta de sueño o los malos patrones de sueño comprometen aún más su calidad de vida. En pacientes con artritis reumatoide, etiologías como el síndrome de piernas inquietas, el síndrome de apnea del sueño y los síndromes de disfunción de la articulación temporomandibular pueden contribuir a los trastornos del sueño.
ConclusionesEs nuestra opinión que la evaluación de la calidad del sueño debe abordarse, monitorearse y tratarse como parte del tratamiento de los pacientes con artritis reumatoide. El mal sueño agrega una carga adicional a la actividad de la enfermedad en estos, además, limita la posibilidad de los pacientes de lograr la remisión de la enfermedad.
Artículo
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora