Lipodystrophy is a pathological condition associated with an abnormal body adipose tissue redistribution. Facial lipoatrophy can be a consequence of congenital, acquired, or involutional. The lipograft is an autologous fat transplant, which constitutes a treatment option that provides volume, tissue regeneration, and advantages in relation to other fillers in autoimmune diseases. The aim is to highlight the filling action and the metabolic effect of facial lipotransfer, due to the grafted adipocytes survival, and the adipose tissue derived stem cells regenerative activity obtained by nano-fat in patients with facial lipoatrophy. Lipoinjection improves the architecture of the new dermis and increases its functional capacity. It is a treatment with autologous tissue (fatty graft) with great efficacy in relation to other alloplastic filler materials capable of exacerbating an inflammatory response mediated by antibody production.
La lipodistrofia es una condición patológica asociada a una redistribución anómala del tejido adiposo en el cuerpo. La lipoatrofia facial puede ser consecuencia de defectos congénitos, adquiridos o involutivos. El lipoinjerto es el trasplante de grasa autóloga y constituye una opción de tratamiento que aporta volumen, regeneración tisular y ventajas en relación con otros materiales de relleno en enfermedades autoinmunes. Se busca resaltar la acción de relleno y el efecto metabólico de la lipotransferencia facial, por la supervivencia de los adipocitos injertados y la actividad regenerativa de las células madre provenientes del tejido adiposo obtenidas por nanofat en pacientes con lipoatrofia facial. La lipoinyección mejora la arquitectura de la nueva dermis y aumenta su capacidad funcional, es un tratamiento con tejido autólogo (injerto graso) con gran eficacia en relación con otros materiales de rellenos aloplásticos capaces de exacerbar una respuesta inflamatoria mediada por la producción de anticuerpos.
Lipodystrophy is a pathological condition associated with an abnormal redistribution of adipose tissue in the body. It can take three main forms: lipohypertrophy, lipoatrophy, and mixed lipodystrophy in cases of pathological accumulation of adipose tissue, focal or general absence of this tissue, or a combination of both, respectively. Lipoatrophy is related to a loss of adipose tissue in the subcutaneous cellular tissue that, although it can affect the entire body, predominates in the face, upper and lower limbs, and buttocks.1
In 2003, Fontdevila et al. proposed a method for the classification of facial lipoatrophy based on physical examination by the specialist, an inexpensive and rapid method that does not require complementary technology. Three grades were established: grade 0, in which the normality of the skin of the malar region is defined and a slight protuberance from the edge of the eye area to the nasolabial fold is evident; grade 1, which describes a flattening of the malar region due to the loss of subcutaneous fat (very similar to the defect observed in skinny people); and grade 2, in which there is a great flattening of the malar region that causes a sunken cheek. The affectation is serious when, in addition to the signs presented in grades 1 and 2, the lack of almost all the subcutaneous fat is associated and the muscular and bone structures are marked due to the fact that the skin adapts more to them, so that a large depression of the cheek and subsequent skeletonization of the face is generated (grade 4).2
Facial lipoatrophy can be the consequence of congenital (malformations), acquired (deformations) or involutional (senile lipoatrophy) defects; it is a problem that is related to esthetic and functional disorders and has physical and psychological repercussions such as depression and stigmatization, by disfiguring and socially disabling the patients. It is usually accompanied by hereditary and acquired diseases, such as scleroderma and deep lupus erythematosus,3 which entails a serious personal, social and labor problem.
Scleroderma is a systemic autoimmune disease characterized by chronic inflammation of the connective tissue. The excessive deposition of collagen and the presence of structural and functional alterations of the blood vessels, internal organs and muscles produce cutaneous fibrosis in the affected areas, which presupposes a dystrophic, thick, shiny and dark skin.4 Deep lupus erythematosus, also called lupus panniculitis, is a rare variant of cutaneous lupus erythematosus that specifically affects the deep dermis and subcutaneous cellular tissue, it occurs in 3% of the patients with cutaneous lupus erythematosus and mainly affects the subcutaneous cellular tissue of the face and areas near the extremities.5
The options to correct the facial defects that occur in these diseases include microsurgical tissue transfer, whose application is limited by the presence of visible scars both in the donor area and in the facial region. In an attempt to find the ideal technique to obtain better surgical outcomes in the face of this entity using less invasive techniques, at present, the field of autogenous fat or adipose tissue grafts is beginning to be explored.4 Adipose tissue is considered the greatest accessible source of adult stem cells, implied in a large number of processes of spontaneous tissue regeneration and repair of damaged tissues. The adipose tissue contains not only adipogenic progenitor cells, but also multipotent stem cells that can differentiate into fat, bone, cartilage, and other types of tissues.6
Isolation of these pluripotent mesenchymal stem cells can be done either by enzymatic or by mechanical method.7 When the process is performed mechanically, the adipocytes are fractured by emulsification and filtration, leaving intact the viable stromal vascular fraction.8 The product obtained from this process is called nanofat, described by Tonnard et al.,9 in which the mechanical disruption of adipose tissue is performed using small diameter Luer Lock connectors, followed by filtration through a filter of 500 mm. The resulting active component and stromal vascular fraction promote endothelial proliferation, creation of collagen, and differentiation and creation of new cells. These stem cells produce a microenvironment in the tissues that in turn stimulates the release of growth factors and promotes angiogenesis and the production of collagen and elastin, which in the long term create a structure that resembles normal tissues, which leads to an improvement in the quality of the skin and even the lightening of pigmented skin.10
Autologous fat transplant can be defined as the transfer of adipose tissue.11 The vast majority of published studies using the lipograft as a treatment for facial lipoatrophy make reference to the volumizing effect after carrying out several sessions on each patient. The objective of this study is to describe two clinical cases of patients with a diagnosis of immune-mediated facial lipoatrophy treated surgically with autogenous material of nanograft type, and to highlight the metabolic effect translated into skin quality and the advantages that are visible from the first treatment session in relation to the response that other filler materials can generate in patients with autoimmune diseases.
Material and methodsThe procedure was carried out in patients who attended the service of Plastic Surgery and Caumatology of the Hermanos Ameijeiras Surgical Clinical Hospital, referred from the Rheumatology service with a diagnosis of facial lipoatrophy of immune cause and who underwent surgery with facial lipotransfer with autogenous nanograft material. An ambulatory surgery was performed, with infiltrative local anesthesia and hospital discharge after the procedure.
Autogenous fat transplantation in patients with autoimmune diseases has indications and contraindications that largely depend on the clinical evolution of the disease, both at a systemic and local level. The patients in whom this type of procedure is indicated are those with facial lipoatrophy of any grade, from 1 to 3, patients with trophic changes in the skin, scars, fibrosis, loss of elasticity, cutaneous hyperpigmentation and sequels of local inflammatory processes. Its indication stands out in systemic sclerosis and in sequels of lupus panniculitis. The procedure should not be carried out in patients who, in addition to the autoimmune disease, present some decompensated comorbidity, in those whose autoimmune disease shows data of systemic activity, who are receiving immunosuppressive treatment or under high doses of steroids (higher than 10 mg/day), psychiatric patients and pregnant women.
The present study was reviewed and approved by the ethics committee of the Service of Plastic Surgery and Burns of the Hermanos Ameijeiras Surgical Clinical Hospital, Havana - Cuba. All the consents required by the current legislation and the principles of the Declaration of Helsinki have been obtained, as well as from the patients for the publication of any personal data and images that appear in the article.
Preoperative consultationPreoperative and preanesthesic check-up was indicated and the surgical treatment, the benefits and the possible complications were explained. Informed consent was signed.
Surgical technique -intraoperativeFacial lipotransfer with autogenous material of nanograft type assisted with adipose tissue-derived stem cells. Abdominal liposuction was performed with a syringe of 20 cc and a cannula of 2 mm; the extracted fat was decanted, centrifuged for 3 min at 2.500 rpm and emulsified with transfer of 2.5, 1.5, 1 and 0.7 mm, and ended with the nanofat grid to subsequently inject the processed fat with a cannula. Measurement of CD34+ cells and CD34+/CD45+ cells was performed by means of a MACSQuant® Analyzer 10 flow cytometer.
PostoperativeSince the immediate postoperative period, antibiotic prophylaxis, analgesia and symptomatic treatment were indicated. Postoperative care included: placement of cold compresses on the lipoinjected areas; daily face wash; and avoidance of leaning on the facial region, make-up, physical exertion or exposure to the sun or steam. Compression in the donor area was indicated. The patients evolved on an outpatient basis, they were guided to reconsultation 4 days after having been operated on and were followed up at one month and at 6 months. Control photographs were taken.
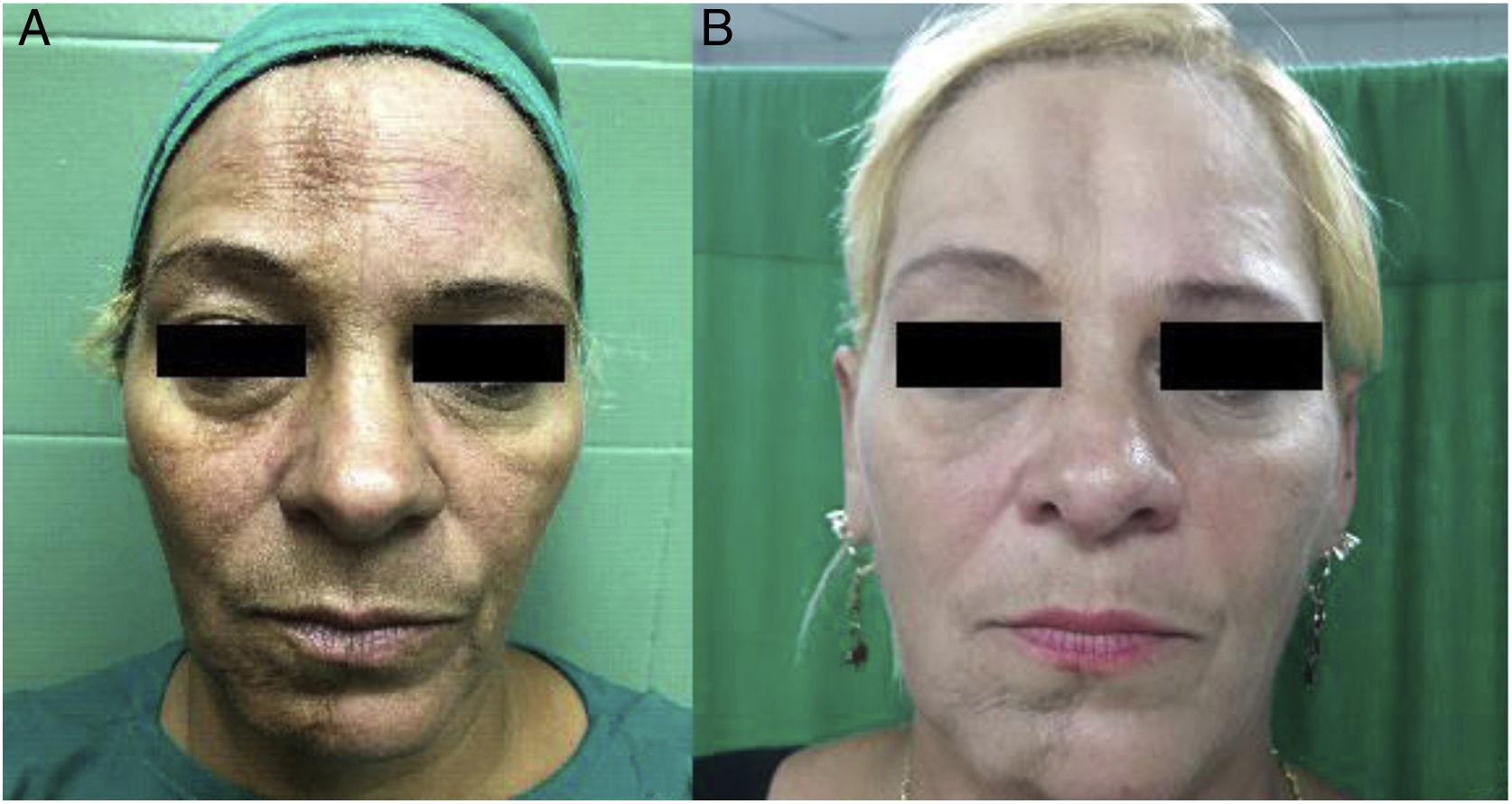
Clinical casesCase 1 A 31-year-old female patient with a pathological personal history of chronic cutaneous lupus erythematosus with scarring alopecia, diagnosed in 2016. In January 2018 she was referred from the Rheumatology service for reconstructive treatment due to physical changes in the right side of the face. She presented great deformity, depression and skeletonization in the malar region due to grade 3 lipoatrophy. In the physical examination, the deterioration of the quality of the facial skin was evident, as well as the presence of persistent erythema, inflammatory lesions and hyperpigmentation due to chronicity (Fig. 1A–C). In the temporal region of the craniofacial massif she presented scarring alopecia of 5 × 4 cm in diameter. The patient was treated with a session of facial lipotransfer; 10 ml of adipose tissue were infiltrated in the form of nanograft. There were no complications (Fig. 1D–F). A 49-year-old female patient, with a pathological personal history of type 2 diabetes mellitus and scleroderma, diagnosed 23 years ago. She attended the outpatient clinic of the service of Plastic Surgery, referred by her treating physician (Rheumatologist) for presenting a lesion in “coup de sabre” of several years of evolution that compromises from the implantation of the hair in the frontal region to the chin in a straight line, in addition to grade 2 right facial hemiatrophy. In the physical examination of the facial region, a rigid, parchment-like, atrophic and hyperpigmented skin with a dark brown color, with greater intensity in the frontal region and on the chin was evident (Fig. 2A). The patient was treated with a session of facial lipotransfer; 15 ml of adipose tissue were infiltrated in the form of nanograft. There were no complications (Fig. 2B).
In the clinical follow-up in the first postoperative year, the decrease in skin fibrosis, less tissue atrophy and a notable improvement in the quality of the skin in relation to texture, color and thickness were evident. There was no expression of the initial scleroderma lesions, the inflammatory infiltrates and indurations disappeared, as well as the initial stiff and inextensible appearance of the skin.
DiscussionLupus erythematosus is an autoimmune disease that can present clinical manifestations in different systems of the body. It can be lethal in the case of systemic lupus erythematosus, or it can occur with cutaneous manifestations without causing damage to another organ. Mucocutaneous manifestations are called specific when they appear exclusively in this disease, and non-specific when they are not exclusive to lupus and can be seen in the context of other ailments.12
Specific manifestations are called cutaneous lupus erythematosus. Histologically, they are represented by a dermal inflammatory infiltrate with a perivascular and periadnexial distribution, vacuolization and degeneration of the keratinocytes of the basal layer, hyperkeratosis and epidermal atrophy. Deep lupus erythematosus or lupus panniculitis is infrequent and manifests with subcutaneous nodules and painless infiltrated plaques that are located mainly on the head and neck, deltoid region, abdominal wall, thighs and buttocks. The esthetic sequels are evident, since these lesions leave depressed scars that produce deformity in the affected area.13
Scleroderma is a multisystem disease that presents with inflammatory, vascular, and sclerotic changes both in internal organs and in the skin. This disease produces an accumulation of collagen fibers in the reticular dermis and causes skin fibrosis that increases the thickness of the dermis and obliterates the cutaneous annexes. As the disease progresses, the skin becomes atrophic, the epidermis becomes thin, the dermal capillaries decrease -leading to hypoxia-, the synthesis of vascular endothelial growth factor increases, among other angiogenic factors, and the subcutaneous cellular tissue is also affected.14
90% of the patients present involvement of the facial region, esthetic changes, alterations in the self-image, and complications in the oral cavity. On the face, the coarse wrinkles on the forehead disappear, thinning of the lips and formation of vertical furrows appear as a consequence of the retraction of the skin. These facial manifestations are disfiguring and imply functional, esthetic and social discomfort; hence the importance of offering therapeutic options that help to correct or improve these complications.15
The transfer of adipose tissue, since its initiation, has been used for filling purposes, and the method of performing it has varied over the years. Initially, the adipose tissue obtained by an “open sky” procedure was used; then, the “unpurified” liposuction, and recently, the “atraumatic purified” technique.16 The atraumatic purified method, introduced by Coleman et al., avoids compressing, filtering, aspirating, washing or having contact with the air, among other maneuvers.15 Lipoinjection is nowadays a common procedure both in reconstructive surgery and in cosmetic surgery, although the lack of clinical evidence makes it difficult to use this type of therapy. There are clinical trials underway and a large number of institutions are conducting studies with stem cells derived from adipose tissue to demonstrate their use in the treatment of other diseases.17
Lipoinjection of subcutaneous cellular tissue is the grafting of fat cells and connective tissue. It can be of adipose tissue, adipose tissue and dermis, or adipose tissue with vascularization (omentum). The adipose tissue is a complex and dynamic tissue that involves various physiological and pathological processes. It is composed of adipocytes, vascular cells, stem cells, pericytes, macrophages, fibroblasts, lymphocytes, and connective tissue. In addition to storing energy, it has endocrine activity by releasing hormones such as adiponectin or leptin and thus regulating homeostasis.18 Adipose tissue-derived stem cells also have a whitening effect on pigmented skin, probably related to their apocrine action by secreting cytokines directly linked to the synthesis of melanin and tyrosine, related to the inhibition of melanin formation induced by exposure to ultraviolet light.10 The benefits of this procedure are diverse: absence of scars, since no incisions are used; long-lasting and natural results; effect of rejuvenation on the face; no major health risks; fast recovery; and it does not require prolonged rest.
In the year 2001, Zuk et al., a group of plastic surgeons and researchers from Pittsburgh, demonstrated that this tissue constitutes a great source of adult mesenchymal stem cells, which they named adipose tissue-derived stem cells. These cells are capable of differentiating into various tissues and are categorized within the group of multipotent mesenchymal stromal cells that correspond to stem cells obtained from adult tissues.19
Adipose tissue-derived stem cells play an important role in the regenerative effect. They can be found in any type of adipose tissue, including subcutaneous and internal (visceral and non-visceral) tissue. It has been reported that the range of extraction of these cells is higher than the range of stem cells obtained from the bone marrow.20 They express traits similar to those of the cells derived from bone marrow, such as proteins and cell markers. Surface antigens are widely used in immunology, examining the expression of surface molecular proteins on these stem cells by flow cytometry.21 These cells are capable of secreting a large number of cytokines and growth factors that are involved in angiogenesis, tissue remodeling, and antiapoptotic events, such as interleukin-6, macrophage colony-stimulating factor, transforming growth factor beta-1, and vascular endothelial growth factor.22
Autogenous fat transfer should be considered a filling, regeneration and restoration medium that provides an improvement in the quality of the tissue in which it is implanted; promotes neovascularization by creating real structural alterations and, thanks of its immunomodulatory property, stimulates the reversal of inflammatory processes caused by aging, scars, loss of substance, radiotherapy or trauma. A great advantage of the use of adipose tissue compared to alloplastic materials is biocompatibility, since alloplastic materials very often produce foreign body reactions.23 Adipose tissue remodeling is a balance between apoptosis, necrosis, and adipogenesis mediated by adipose tissue-derived stem cells. The lipograft could fertilize chronically inflamed or irradiated tissues, in which an alteration in remodeling or healing has ocurred.24
Lipoinjection, in addition to its use as a soft tissue filler, is used in various medical-surgical specialties, in burn injuries, in trauma, and for the treatment of chronic wounds and pathological scars, in addition to the treatment of Dupuytren's contracture, together with the aponeurotomy.25 The benefits of this type of therapy become noticeable after a few months, since the stem cells regenerate and optimize the quality of the tissues, thus improving the quality of life of these patients.
ConclusionsThe adipose tissue is an important source of pluripotent stem cells capable of differentiating into different types of cells, which gives it an important regenerative and restructuring capacity.
Lipotransfer is a useful, fast and economical surgical technique with excellent results both in the field of cosmetic surgery and in reconstructive surgery, which, in addition, due to its regenerative power, can be used to treat autoimmune conditions.
The transfer of adipose tissue on alloplastic materials is the option for the treatment of localized atrophies in patients with autoimmune diseases, with clinical impact on the quality of the tissues through the immunomodulation and immunocompatibility of adipose tissue stem cells, which allows the morphological restructuring of skin atrophy, tissue regeneration and reversal of the sclerodermal cutaneous process.
The use of an autogenous product in the treatment of these tissue defects in patients with hyperfunction of the immune system offers a greater advantage, since a fat autograft will be better tolerated than the filling with materials that are not of their own and are capable of exacerbating an inflammatory response mediated by the production of antibodies in patients with autoimmune diseases.
Ethical ConsiderationsThe ethics committee of the Service of Plastic Surgery and Burns of the Hermanos Ameijeiras Surgical Clinical Hospital (Havana - Cuba) approved the research. We confirm that we have obtained the consents required by current legislation for the publication of any personal data or images of the patient.
Conflict of interestThe authors declare that they have no conflict of interest.