Kawasaki disease is part of a heterogeneous group of low frequency diseases that are characterized by the presence of inflammation and necrosis of the vascular wall, generating various clinical and pathological manifestations, which compromise medium vessels, and mainly affecting the pediatric population. The case is presented of a 36-year-old man with no relevant past medical history, with a febrile episode of 4 days of onset, together with headache, nausea, and odynophagia with subsequent onset of multiple generalized maculopapular lesions. These resolved with subsequent desquamation of fingers, palms and soles of feet. Non-suppurative bilateral conjunctivitis is documented, as well as involvement of oral mucosa and lips. Skin biopsy reported lymphocytic vasculitis, associated with renal, hepatic and cardiac involvement (dilated cardiomyopathy with depressed ejection fraction). A diagnosis of complete adult Kawasaki disease with atypical manifestations was established. He was treated with methylprednisolone, acetylsalicylic acid 100mg per day, and a single dose of intravenous IgG immunoglobulin 2g/kg, and daily dialysis therapy to achieve complete recovery.
La enfermedad de Kawasaki forma parte de un grupo heterogéneo de afecciones de baja frecuencia que se caracterizan por la presencia de inflamación y necrosis de la pared vascular, que generan diversas manifestaciones clínicas y patológicas, las cuales comprometen medianos vasos, y que afectan principalmente a la población pediátrica. Presentamos el caso de un hombre de 36 años de edad, sin antecedentes patológicos previos, con cuadro febril de 4 días de evolución asociado a cefalea, náuseas y odinofagia, con posterior aparición de múltiples lesiones maculopapulares generalizadas, las cuales se resolvieron con descamación en pulpejos, palmas y plantas. Se documenta conjuntivitis no supurativa bilateral, además de compromiso de la mucosa oral y los labios. La biopsia de piel reportó vasculitis linfocítica asociada a compromiso renal, hepático y cardiaco (miocardiopatía dilatada con fracción de eyección deprimida); se configuró el diagnóstico de enfermedad de Kawasaki completa del adulto con manifestaciones atípicas. Recibió tratamiento con metilprednisolona, ácido acetilsalicílico 100mg/día, una dosis única de inmunoglobulina IgG intravenosa 2g/kg y terapia dialítica interdiaria, logrando una recuperación completa.
Kawasaki disease is a medium-sized vessel vasculitis, with an acute, self-limiting evolution and of unknown origin, mainly affecting children less than 5 years old.1 It was originally described by Doctor Tomosaku Kawasaki in Japan, where a progressive increase in its incidence – 265 cases per every 100,000 children under 5 years of age – is documented,2,3 in contrast to the numbers documented in the United States, where the incidence ranges from 19 to 27.7 cases per every 100,000 children less than 5 years old. This indicates a probable genetic predisposition and the presence of an environmental antigen.2,3
This is a rare disease among adults and there have been less than 60 cases reported worldwide, in patients between 18 and 30 years old; two cases were found in South America, and none in Colombia.4 Seasonal outbreaks have been described, indication a potential infectious source, with a higher frequency during winter than in summer.4
The clinical progression involves 3 phases: acute, sub-acute, and chronic, as evidenced by the various studies conducted in the pediatric population. The acute phase, with an approximate duration of 3 weeks, manifests with fever, inflammatory heart disease, mucocutaneous changes and rash. During this phase of the disease, coronary aneurysms and symmetrical polyarthalgias of the large joints develop.4 The sub-acute phase presents with palmar and plantar desquamation and heart disease during the second and third week of evolution, and finally convalescent or the chronic phase that may last for weeks and even months, until a clinical and paraclinical resolution.
The clinical presentation may be complete when fever lasts for ore than 5 days, in addition to 4 of the 5 criteria of the American College of Rheumatology (ACR) as follows: polymorphic exanthema (diffuse maculopapular lesions of the trunk and extremities), erythema with edema of the hands and feet, followed by fingertips and feet desquamation, bilateral non-exudative conjunctival injection, changes in the oral mucosa and lips (strawberry tongue, fissured and erythematous lips, oral and pharyngeal hyperemia) and unilateral cervical lymphadenopathy >1.5cm in diameter.5 The other clinical presentation is incomplete, when only 2 or 3 ACR criteria are met. Similarly, an atypical variety has been described with renal involvement, acute abdomen, and pleural effusion.5 Its diagnosis is clinical and of exclusion.
This is the case of a male adult patient who meets the ACR criteria for Kawasaki disease. What is relevant about this case is its atypical adult presentation that led to a review of the literature and is the first case reported in Colombia.
Clinical caseThis is a 36-year old man living in Pereira, baker by profession, who visits the doctor because he has been experiencing a 39°C fever for 4 days, associated with generalized headache with a pain score of 7/10. The patient also presents with odynophagia, nausea and occasional vomiting, with no additional GI symptoms. 4 days later, the patient presents with maculopapular lesions of the upper and lower extremities, the chest, and the abdomen and was admitted to hospital (Fig. 1). The patient has no history of past pathologies and does not use any psychotropic substances. At admission, his vital signs were as follows: BP 130/70mmHg, HR 135lpm, RR 22bpm, temperature 39°C. The physical examination showed orientation in the 3 dimensions, collaborative, absence of cervical lymphadenopathies, with rhythmic tachycardia bruit and no murmurs. Normal breath sounds with no adventitious respiratory sounds. The patient presented with a left inguinal lymphadenopathy, free of edema or neurological deficits. Multiple generalized maculopapular lesions were identified, that did not regress with digital pressure with subsequent desquamation of the fingers, palms and soles of the feet, after 10 days of hospitalization; dry and chapped lips with angular fissures and non-exudative conjunctival injection (Fig. 2).
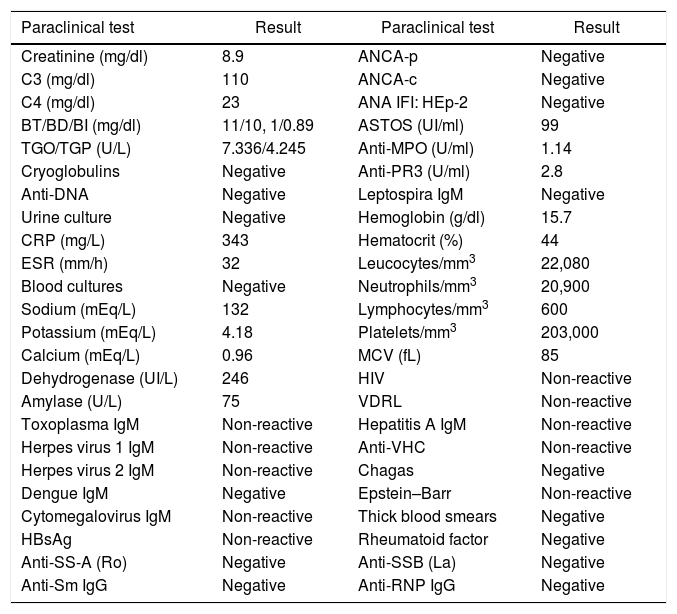
The paraclinical tests at admission showed leukocytosis and neutrophilia, elevated acute phase reactants, direct hyperbilirubinemia, and elevated transaminases. Urinalysis with proteinuria and hematuria. The blood and urine cultures were negative, as described in Table 1. The patient rapidly progressed to multiple organ failure (lung, kidney, cardiovascular and liver involvement) and hypotension leading to ICU admission to initiate empirical broad spectrum antibiotic (ceftriaxone, vancomycin and meropenem) therapy, invasive mechanical ventilation, and slow continuous hemodialysis. Initially, the suspected diagnosis was staphylococcal toxic shock syndrome, meningococcemia, ischemic hepatitis secondary to hypoperfusion, dilated cardiomyopathy with depressed ejection fraction. Based on serological tests, HIV infection, hepatitis A, B, C and E, leptospirosis, dengue, cytomegalovirus infection, Epstein–Barr virus, herpes virus, and Chagas disease were all ruled out.
Paraclinical tests at patient admission.
| Paraclinical test | Result | Paraclinical test | Result |
|---|---|---|---|
| Creatinine (mg/dl) | 8.9 | ANCA-p | Negative |
| C3 (mg/dl) | 110 | ANCA-c | Negative |
| C4 (mg/dl) | 23 | ANA IFI: HEp-2 | Negative |
| BT/BD/BI (mg/dl) | 11/10, 1/0.89 | ASTOS (UI/ml) | 99 |
| TGO/TGP (U/L) | 7.336/4.245 | Anti-MPO (U/ml) | 1.14 |
| Cryoglobulins | Negative | Anti-PR3 (U/ml) | 2.8 |
| Anti-DNA | Negative | Leptospira IgM | Negative |
| Urine culture | Negative | Hemoglobin (g/dl) | 15.7 |
| CRP (mg/L) | 343 | Hematocrit (%) | 44 |
| ESR (mm/h) | 32 | Leucocytes/mm3 | 22,080 |
| Blood cultures | Negative | Neutrophils/mm3 | 20,900 |
| Sodium (mEq/L) | 132 | Lymphocytes/mm3 | 600 |
| Potassium (mEq/L) | 4.18 | Platelets/mm3 | 203,000 |
| Calcium (mEq/L) | 0.96 | MCV (fL) | 85 |
| Dehydrogenase (UI/L) | 246 | HIV | Non-reactive |
| Amylase (U/L) | 75 | VDRL | Non-reactive |
| Toxoplasma IgM | Non-reactive | Hepatitis A IgM | Non-reactive |
| Herpes virus 1 IgM | Non-reactive | Anti-VHC | Non-reactive |
| Herpes virus 2 IgM | Non-reactive | Chagas | Negative |
| Dengue IgM | Negative | Epstein–Barr | Non-reactive |
| Cytomegalovirus IgM | Non-reactive | Thick blood smears | Negative |
| HBsAg | Non-reactive | Rheumatoid factor | Negative |
| Anti-SS-A (Ro) | Negative | Anti-SSB (La) | Negative |
| Anti-Sm IgG | Negative | Anti-RNP IgG | Negative |
The transthoracic echocardiogram documented dilated cardiomyopathy, significant reduction of the overall contractility with a severely compromised systolic function due to an ejection fraction of 25% and dilatation of the right cavities with grade III tricuspid regurgitation. A subsequent cardiac MRI ruled out infiltrative disease with an ejection fraction of 51.5%.
The skin punch biopsy of the left leg lesion and the abdomen showed a perivascular lymphocytic-like cell infiltrate that is consistent with medium-sized vessel vasculitis (Kawasaki disease), in addition to meeting 5 of the 6 ACR criteria: fever for more than 5 days, bilateral non-exudative conjunctival injection, dry and chapped lips with angular fissures, palmar and plantar erythema, indurated edema with general desquamation limited to the fingers, palms and soles of the feet (convalescent phase) (Figs. 3 and 4). Additionally, the patient had dilated cardiomyopathy with depressed ejection fraction, acute renal failure, and liver involvement. No aneurysmal dilatation or unilateral cervical lymphadenopathy was observed in this case. The patient presented only one left inguinal lymphadenopathy at admission, with a renal biopsy report of acute tubular necrosis subsequently resolved. The patient was treated with pulses of methylprednisolone at an IV dose of 1g/day and acetylsalicylic acid 100mg/day, with a satisfactory evolution and complete resolution of symptoms. During follow-up, the hemodialysis catheter was removed upon renal function improvement, and continues acetylsalicylic acid treatment.
DiscussionKawasaki disease is a medium-sized vessel vasculitis, of acute, self-limiting presentation of unknown origin, affecting mostly children under 5 years old.1 This is a rare disease in adults and less than 60 cases have been reported worldwide in patients ranging from 18 to 30 years old. 2 cases have been reported in South America, and none in Colombia.4 Our patient was 36 years old at the time of diagnosis, exceeding the age range so far described.
The incidence of cardiac involvement in adults is less than 5%, in contrast to the pediatric population, where it may exceed 30% of the cases, with evidence of aneurysms.6 No aneurysmal dilatations were identified in this case.
In Colombia, this condition has only been described in children and the aneurysmal involvement of the coronary arteries is higher as compared with adults, in whom there is a prevalence of atypical lung, liver, and kidney involvement,7,8 as manifested in our patient, with rapid onset of multiple organ failure.
A study conducted in Bogotá between 2007 and 2009, documented 4 pediatric cases among a total of 86 patients with febrile exanthema.9 100% of the cases experienced fever and oropharyngeal changes, half of them had conjunctival involvement and 75% of the children developed palmoplantar desquamation.9
Similar results were documented in another study conducted in 5 hospitals in Barranquilla between 2002 and 2008, where 20 medical records of patients with Kawasaki disease were reviewed, of which 40% were less than one-year old and the age ranged between 3 months and 8 years. Of these patients, 95% presented the complete form of the disease, in 65% of the cases the primary symptom was fever and 30% presented with cardiac involvement due to the presence of coronary aneurysms.10
Our adult patient met 5 of the 6 ACR criteria for the complete form of Kawasaki disease, with atypical manifestations due to the kidney involvement (renal failure that responded to therapy), cardiac compromise (cardiomyopathy) and liver involvement (toxic hepatitis) that was treated with methylprednisolone, acetylsalicylic acid, one dose of IV immunoglobulin IgG, and intermittent hemodialysis.
The mortality rate among children is less than 1%, with the most significant complications from ischemic cardiomyopathy presenting during the convalescent phase.11 There are no reports on mortality and complication rates in adults, because of the rare clinical presentation of this population.
Up to 2010, 81 cases the classical Kawasaki disease had been reported in adults, and 13 cases of the incomplete form.5 According to the AHA in 2017, the incomplete form is described as: unexplained fever for less than 4 days, with 2 or 3 major clinical criteria and paraclinical or imaging findings showing evidence of the disease.
The differential diagnoses include hypersensitivity reactions secondary to medications, toxic shock syndrome, scarlet fever, measles, viral infections (adenovirus, parvovirus, herpes virus, rubella, and cytomegalovirus), toxoplasmosis, leptospirosis, and rickettsial disease. Other diagnosis are rheumatic fever, reactive arthritis, and systemic juvenile idiopathic arthritis5,10; all of these diagnoses were ruled out in our patient.
The treatment consists of suppressing the inflammation primarily in the coronary arteries in order to prevent the development of aneurysmal dilatations,12 using acetylsalicylic acid (80–100mg/day) and IV immunoglobulin IgG (2g/kg) at a single dose, which in randomized controlled trials have proven to reduce the number of coronary aneurysms and were administered to the patient with a favorable resolution of symptoms.12
ConclusionsKawasaki disease is a medium-sized vessel vasculitis affecting children under 5 years old, and is quite rare in adults. This case is therefore the first one reported in Colombia. Its diagnosis of exclusion after ruling out an infectious cause and its early identification, allows for improved quality of life of the patient, preventing complications associated with multiple organ failure.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Guzmán Montealegre JC, Saldarriaga Rivera LM, Castro Rodríguez A, Henao Velásquez CM. Enfermedad de Kawasaki. Reporte de un caso infrecuente en el adulto. Rev Colomb Reumatol. 2019;26:132–136.