Hip joint involvement in rheumatoid arthritis has been related to disability and lower quality of life. Currently, not enough studies provide information for subclinical hip involvement.
ObjectivesTo determine the prevalence of subclinical hip joint involvement in rheumatoid arthritis, characterizing it by ultrasound.
Materials and methodsA descriptive cross-sectional study in rheumatoid arthritis patients with an established diagnosis of rheumatoid arthritis according to EULAR/ACR 2010 classification criteria, without hip pain or abnormalities during a clinical examination (subclinical group), this group was compared with a group of symptomatic patients with rheumatoid arthritis of the hip (pathological control group), and with healthy control individuals matched by age and body mass index. The presence of joint capsule distension, osteophytes, joint remodelling process, erosions, iliopsoas bursitis, and power Doppler signal was assessed. The images were interpreted by an experienced rheumatologist blinded to clinical and laboratory variables.
Results234 hips were studied; 37 (31.6%) symptomatic hip patients, 40 (34.1%) asymptomatic hip patients and 40 (34.1%) healthy individuals. The prevalence of joint capsule distension was 20%, while symptomatic hip patients and healthy individuals had a prevalence of 48.6% and 15%, respectively. The asymptomatic group presented higher values for osteophytes and joint remodelling.
ConclusionsUltrasound is a sensitive tool to identify subclinical hip joint synovitis in rheumatoid arthritis patients, reaffirming the value of ultrasound in preclinical diagnosis. The presence of erosions and iliopsoas bursitis was low; we observed no power Doppler signals nor significant associations between ultrasound findings with disease activity and laboratory test results.
El compromiso de la articulación coxofemoral en la artritis reumatoide se asocia a discapacidad y menor calidad de vida. En la actualidad, no existen estudios que evalúen sus alteraciones en etapas subclínicas.
ObjetivosDeterminar la prevalencia del compromiso subclínico de cadera mediante el uso del ultrasonido.
MetodologíaEstudio descriptivo de corte transversal, enfocado en pacientes con diagnóstico establecido de artritis reumatoide, según los criterios clasificatorios de la EULAR/ACR 2010, que presentaron o no dolor en la articulación coxofemoral durante el examen físico, comparados con individuos sanos. Se investigó la presencia de distensión de la cápsula articular, bursitis del iliopsoas, erosiones, osteofitos, remodelación articular y señal Doppler de poder. Las imágenes fueron interpretadas por un reumatólogo experto en US, cegado a las variables clínicas, demográficas y de laboratorio.
ResultadosSe evaluaron en total 234 caderas; 37 (31,6%) pacientes con artritis reumatoide sintomáticos de la cadera, 40 (34,1%) pacientes con artritis reumatoide subclínica y 40 (34,1%) sujetos sanos. La prevalencia de sinovitis de la cápsula articular fue de 48,6% para los pacientes con artritis reumatoide sintomática, 20% para los pacientes con artritis reumatoide subclínica y 15% para los sujetos sanos. El grupo de pacientes con artritis reumatoide subclínica presentó una mayor frecuencia de osteofitos y remodelación articular.
ConclusionesSe confirmó el valor del ultrasonido en el diagnóstico subclínico de la patología inflamatoria de la articulación coxofemoral. No se evidenciaron asociaciones significativas entre los hallazgos del US con la actividad de la enfermedad, ni con los valores de estudios de laboratorio.
Rheumatoid arthritis (RA) is an autoimmune condition characterized by systemic inflammation. Its main clinical feature is chronic symmetrical polyarthritis of the diarthrodial joints.1 In the case of the hip —or coxofemoral joint—, morphological and structural alterations can lead to the collapse of the femoral head and remodelling of the acetabulum.2 This can generate disability, increased morbidity and mortality, and a greater number of joint replacement surgeries3; these three situations can significantly impact the prognosis of the disease.4
From a clinical point of view, hip involvement, in its initial stages, can go unnoticed by the physician and the patient or be asymptomatic.5 In the case of symptoms, these range from pain in the inguinal or gluteal regions to a limited range of motion that mainly affects abduction and internal rotation4,6; these findings are not specific.5
Variable involvement of the hip joint has been documented in some reviews that analyze the frequency and distribution of joint involvement in RA. Duró Pujol4 reports a prevalence of 5%, a value that increases to 50% as the disease progresses. For their part, Nasswetter et al.5 highlight an affection of 20%. It is convenient to consider that the frequency of involvement of the coxofemoral joint is variable and depends on the imaging method used for its evaluation.
Ultrasound (US) is a non-invasive imaging technique that has proven to be a useful tool for the detection of synovitis and erosions from the early stages of the disease. In addition, it is more sensitive than physical examination in detecting joint inflammation in patients with undifferentiated RA and in those with established RA (>1 year of evolution),7,8 which makes it possible to reclassify oligoarticular to polyarticular disease.9 In recent years, the capacity of the US to detect subclinical alterations in different joints has been investigated, which opens a new horizon in clinical research: pre-symptomatic detection of joint involvement.10
In the case of the hip joint, the US has several indications, including the detection of the following elementary lesions: synovitis, bursitis, detection of muscular and tendon disease, enthesitis, detection of inguinal hernias, loose bodies, assessment of labrum disorders, bone erosions, cartilage lesions, and osteophytes. It is worth mentioning that all these elementary lesions can be observed in both rheumatologic and non-rheumatic diseases, including osteoarthritis (OA) and spondyloarthritis, as well as trauma and infectious processes, so they are not specific for RA.11 The main disadvantage of US in the assessment of the hip joint lies in its limited acoustic window, which can additionally be modified by the amount of adipose panniculus of the evaluated subject, which makes it difficult to observe the femoral head, the articular cartilage, and its joint capsule. Likewise, since it is located in a deep anatomical plane, the application of tools such as power Doppler is not very sensitive.12,13
The present study aims to determine the prevalence of subclinical involvement and ultrasonographic characteristics of the hip joint in a group of patients with RA, with and without clinical signs or symptoms of coxofemoral involvement, contrasting them with a group of healthy individuals (healthy controls). Linear regression models were used to assess possible associations between US findings and demographic, clinical, and laboratory variables.
MethodsA descriptive, cross-sectional study was conducted. The sample size was estimated from the probability formula for defined populations, with a confidence limit of 95% and an error of 5%, obtaining a sample size of 60 patients, according to the following calculation:
Confidence = 95% → Z = 1.96.Error = 0.05.N = 72 patients with RA who would attend the research unit in four months (60 subjects attend per month, of which 30% correspond to RA).p = 0.38 (mean obtained from the studies published by Di Geso et al.14 and Koski15).q = 0.62.It has been based on the hypothesis that, in healthy subjects, the prevalence of ultrasonographic changes (mainly synovitis) of the coxofemoral joint would be 10%, versus a 38% prevalence in patients with symptomatic RA and an intermediate proportion in patients with asymptomatic RA. For the comparison of the difference in proportions, these two extreme values were taken a priori. Assuming an alpha error of 5% (confidence level of 95%) and a beta of 20% (statistical power of 80%), the following formula was applied to calculate the sample size:
Where:
▪The lowest expected synovitis value is 0.10 without AR = p2.
▪The highest value of expected synovitis is 0.38 with symptomatic RA = p1.
▪The difference between the two is 0.38−0.10 = 0.28 (delta).
▪Zα = 1.96 (alpha error 5%).
▪Zβ = 0.84 (beta error 20%).
For the groups to be of equal proportion (that is, 0.50), then:
▪p = p1q1 + p2q2 = 0.50 × 0.38 + 0.50 × 0.10 = 0.19 + 0.5 = 0.24.
▪q = 1 - p = 1−0.35 = 0.76.
▪n = [1.96 √2 0.24 (0.76) + 0.84 √0.38 (0.62) + 0.10(0.90)/(0.28)]2 = 35 subjects per group.
The study focused on patients who attended the US Unit of the Musculoskeletal and Rheumatic Diseases Division of the Luis Guillermo Ibarra Ibarra National Rehabilitation Institute with an established diagnosis of RA, according to the 2010 classification criteria of the European League Against Rheumatism (EULAR) and the American College of Rheumatology (ACR).16 The study included individuals older than 18 years, with a body mass index (BMI), equal to or less than 29.9 kg/m2, with or without a history of hip joint pain (defined as pain in the groin or lower gluteal region), or pain or restriction of movement on physical examination (defined as pain on pressure on Scarpa's triangle or during the performance on arcs of motion of flexion, abduction, internal rotation, external rotation or extension).4,6 Subjects with arthropathies other than RA were excluded, such as microcrystal deposition disease, diagnosis of primary OA or fibromyalgia, history of avascular necrosis of the hip, previous hip surgery, hip prostheses, glucocorticoid infiltration or viscosupplementation in the last 3 months, data suggestive of hip malformations, pregnant women, and history of significant trauma in the coxofemoral region.
Demographic and clinical data from the electronic record were collected. In the case of laboratory variables (RF, ESR, and CRP), the latest studies recorded in the clinical file were considered.
Medical and nursing staff oversaw obtaining clinical data and physical examination. Tender and swollen joints were counted to estimate the degree of RA activity. To calculate the Disease Activity Score (DAS28-CRP), the ReumaHelper application, version 3.2, freely downloadable from the Play Store, was used. Disease activity was estimated as follows: remission: DAS28 <2.6; low activity, between 2.6 and 3.2; moderate activity, between 3.2–5.1, and high activity, >5.1. Additionally, a specific physical examination of the coxofemoral joint was carried out, asking the patient to lie on his back, and pressure was applied to the inguinal region. Finally, active and passive mobilization of all ranges of movement was performed.
ClinimetryThe free downloadable Health Assessment Questionnaire (HAQ) in Spanish (https://www.ser.es/wp-content/uploads/2016/07/HAQ-SER-SPANISH-QUESTIONNAIRE.pdf) was used to assess the functional capacity of patients in eight areas: dressing and grooming, getting up, eating, walking, hygiene, reaching, pressure, and others, with a score ranging from 0 (no disability) to 3 (maximum disability). Likewise, the Spanish version of the Copenhagen Hip and Groin Outcome Score (HAGOS) questionnaire (http://www.koos.nu/), an instrument designed to evaluate patients' perception of their hip disability, specifically to assess the hip joint in young and middle-aged, physically active people, through six subscales (symptoms, joint stiffness, pain, daily activities, sports activities, and quality of life). The score ranges from 100 (no problems) to 0 (extreme problems). The questionnaires were self-administrated after a brief instruction by the medical or nursing staff.
The participants' posture and gait (antalgic and Trendelenburg) were assessed. In dorsal decubitus, anthropometric measurements of both lower limbs were taken (from the anterior superior iliac spine to the internal malleolus, considering a difference of 1 cm or less as normal). Pressure was applied to Scarpa's triangle and the trochanteric region, and the abduction movement against resistance was performed.6
The arcs of movement were determined with a ruler-type goniometer, with the knees extended and both anterior superior iliac spines at the same level, to measure flexion (normal: 120°), abduction (normal: 45°), and adduction (normal: 30°). In a sitting position, with the knees hanging and in 90° flexion, internal and external rotation was assessed (normal: 45°). Finally, the patient was asked to assume the prone position, with the knees extended and both anterior superior iliac spines at the same level, to take the extension measurement (normal: 30°).17
Plain hip radiographs were evaluated to assess the presence or absence of alterations (joint space reduction in the axial, superior, or medial direction, subchondral sclerosis, osteophytes, osteopenia, erosions, and bone cysts). For the ultrasonographic study, US General Electric Venue 40 equipment was used, equipped with a 6−12 MHz linear transducer and a power Doppler system. The study was initially performed by two operators: the first with extensive experience in musculoskeletal and joint US (>15 years of practice) and the second in the training process. Once the second operator was properly trained, he continued with the acquisition of the remaining images.
The study subjects were in a supine position, with the knees extended and the feet in slight external rotation, and the hip joint was examined from its anterior face bilaterally. The study was conducted in orthogonal planes (longitudinal and transverse). In the anterior region, approximately at the level of the inguinal crease, the transducer was angled slightly toward the axis of the femoral neck. The following structures were assessed: the acetabulum, the labrum, the femoral head, the femoral neck, and the joint capsule and its content. The height of the joint capsule was measured, according to the recommendations of Koski et al.18. The femoral head and iliopsoas tendon were evaluated in cross-sections. The exploration methodology was carried out following the US EULAR guidelines in Rheumatology.19,20 The trochanteric region was not assessed.
All anatomical areas were assessed on gray scale to detect structural changes, and subsequently, power Doppler was used to detecting abnormal blood flow. The images were interpreted by an expert rheumatologist, blinded to the demographic, clinical, and laboratory data of all RA patients and healthy controls. Participants were divided into three study groups: group 1: symptomatic hip RA; group 2: asymptomatic hip RA (subclinical), and group 3: healthy subjects.
Clinical, anthropometric, and demographic variablesThe following variables were considered: gender, age, body mass index (BMI); disease duration, use of disease-modifying antirheumatic drug (DMARD); use of corticosteroids (prednisolone or deflazacort), use of biological DMARDs, DAS28, HAQ, HAGOS, laboratory/radiological: erythrosedimentation rate (ESR), C-reactive protein (CRP), rheumatoid factor (RF), anti-cyclic citrullinated peptide (anti-CCP) antibodies, simple pelvic radiograph (anteroposterior projection); ultrasonographic: presence of ultrasonographic alterations, synovitis (synovial hypertrophy, effusion and distension of the joint capsule >7 mm), bone erosion, joint remodelling, osteophytes, bursitis, lesion of hyaline cartilage and fibrocartilage (labrum) and power Doppler signal. Table 1 presents the definitions of the US variables.
Description of ultrasound variables.
| Distension of the joint capsule | Distance between the joint capsule and the bony edge of the femoral neck of 7 mm or more, or a difference of 1 mm or more between both hips,18 associated or not with the presence of a hypoechoic layer within the joint capsule, in addition to rectification or convexity of the joint capsule concerning the femoral cortex23 |
| Synovial hypertrophy | The presence of hypoechoic abnormal synovial tissue, located within the joint capsule, not displaceable, slightly compressible, and can show power Doppler signal24,25 |
| Joint effusion | Abnormal hypoechoic or anechoic intra-articular material (relative to subdermal fat) that is displaceable and compressible and leaves no power Doppler signal24 |
| Synovitis | Presence of hypoechoic synovial hypertrophy, regardless of the presence of effusion or any degree of Doppler signal24,25 |
| Bone erosion | Intra- and/or extra-articular discontinuity of the bone surface (visible in two perpendicular planes)24,25 |
| Joint remodelling | Flattening of the visible portion of the femoral head23 |
| Osteophyte | Bone margin prominence visible in two perpendicular planes24,25 |
| Bursitis | Distension of the bursa wall with the presence of fluid collection and/or synovial proliferation that may show a power Doppler signal12 |
| Power Doppler signal | Color image on the gray scale representing real-time synovial microvascular flow (Doppler flow). Grade 1: the presence of at least three isolated signs. Grade 2: the presence of more than three isolated or confluent signals in less than half of the synovial articular surface. Grade 3: confluent signals in more than half of the synovial surface28 |
The statistical program SPSS version 17.0 for Windows 10 was used. For the analysis of the descriptive results, means, percentages and standard deviations were used. The chi-square (χ2) and Student's t-tests were applied to compare the qualitative and quantitative variables of the different groups, depending on the case. Statistical significance was assumed with a p-value ≤0.05. Linear regression models were employed to assess possible associations between US findings and demographic, clinical, and laboratory variables. Additionally, Cohen's kappa coefficient was used to observe the agreement between two observers (expert rheumatologist and US trainee), considering the following values: K = 0.00−0.20, slight agreement; 0.21−0.40, acceptable; 0.41−0.60, moderate; 0.61−0.80, substantial; 0.81–1.00: perfect.
Ethical considerationsThis study was approved by the Ethics and Research Committee of the Luis Guillermo Ibarra Ibarra National Rehabilitation Institute. The participants gave their informed consent to take part in this study.
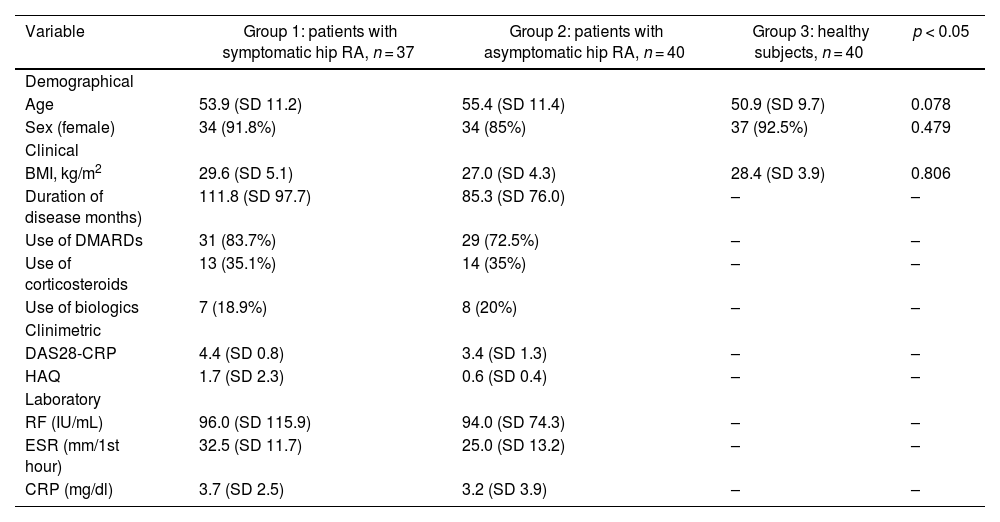
ResultsA total of 234 coxofemoral joints belonging to 77 patients with RA and 40 healthy subjects were analyzed, grouped as follows: group 1: 37 subjects with symptomatic hip RA; group 2: 40 patients with asymptomatic hip RA (subclinical), and group 3: 40 healthy subjects (control). Age, sex, and BMI did not present significant differences between the groups studied (Table 2).
Demographic, clinical, and laboratory features.
| Variable | Group 1: patients with symptomatic hip RA, n = 37 | Group 2: patients with asymptomatic hip RA, n = 40 | Group 3: healthy subjects, n = 40 | p < 0.05 |
|---|---|---|---|---|
| Demographical | ||||
| Age | 53.9 (SD 11.2) | 55.4 (SD 11.4) | 50.9 (SD 9.7) | 0.078 |
| Sex (female) | 34 (91.8%) | 34 (85%) | 37 (92.5%) | 0.479 |
| Clinical | ||||
| BMI, kg/m2 | 29.6 (SD 5.1) | 27.0 (SD 4.3) | 28.4 (SD 3.9) | 0.806 |
| Duration of disease months) | 111.8 (SD 97.7) | 85.3 (SD 76.0) | – | – |
| Use of DMARDs | 31 (83.7%) | 29 (72.5%) | – | – |
| Use of corticosteroids | 13 (35.1%) | 14 (35%) | – | – |
| Use of biologics | 7 (18.9%) | 8 (20%) | – | – |
| Clinimetric | ||||
| DAS28-CRP | 4.4 (SD 0.8) | 3.4 (SD 1.3) | – | – |
| HAQ | 1.7 (SD 2.3) | 0.6 (SD 0.4) | – | – |
| Laboratory | ||||
| RF (IU/mL) | 96.0 (SD 115.9) | 94.0 (SD 74.3) | – | – |
| ESR (mm/1st hour) | 32.5 (SD 11.7) | 25.0 (SD 13.2) | – | – |
| CRP (mg/dl) | 3.7 (SD 2.5) | 3.2 (SD 3.9) | – | – |
DAS28: Disease Activity Score; SD: Standard deviation; DMARD: disease-modifying antirheumatic drug; RF: Rheumatoid factor; HAQ: Health Assessment Questionnaire; BMI: Body mass index; CRP: C-reactive protein; ESR: Erythrosedimentation rate; RA: Rheumatoid arthritis.
The HAGOS questionnaire showed differences between the asymptomatic and symptomatic RA groups (p ≤ 0.0001). The prevalence of synovitis was 48.6% for symptomatic RA patients, 20% for asymptomatic RA, and 15% for healthy subjects; the first two groups presented significant differences (p = 0.008). Patients with asymptomatic hip RA presented a higher frequency of hip osteoarthritis (joint remodelling and osteophytes), but significant differences were only observed in femoral head remodelling between the asymptomatic RA group and healthy subjects (p = 0.002). The presence of elementary lesions such as erosions and iliopsoas bursitis was very low, occurring in only four patients. No power Doppler signal was observed in any of the cases (Table 3). Fig. 1 depicts representative images of the documented ultrasound findings.
Clinimetry for the hip joint and ultrasonographic findings.
| Variable | Symptomatic RA, n = 37 | Asymptomatic RA (subclinical), n = 40 | Healthy subjects, n = 40 | p-valueSymptomatic vs. Asymptomatic RA | p-valueAsymptomatic RA vs. Healthy subjects | p-valueSymptomatic RA vs. healthy subjects | Observed statistical ´power (%)Comparison of the three groups |
|---|---|---|---|---|---|---|---|
| Clinimetric | |||||||
| HAGOS | 46.4 (17.9) | 87.4 (11.48) | 91.0 (12.2) | <0.0001 | 0.173 | 0.0001 | 84.3 |
| Ultrasonographic | |||||||
| Hip joint synovitis | 18 (48.6%) | 8 (20%) | 6 (15%) | 0.008 | 0.556 | 0.01 | 81.9 |
| Joint remodelling | 5 (13.5%) | 11 (27.5%) | 1 (2.5%) | 0.131 | 0.002 | 0.08 | 79.6 |
| Osteophytes | 1 (2.7%) | 8 (20%) | 4 (10%) | 0.018 | 0.210 | 0.20 | 71.5 |
| Erosions | 1 (2.7%) | 0 | 0 | 0.295 | – | 0.48 | 59.1 |
| Iliopsoas bursitis | 0 | 1 (2.5%) | 2 (5%) | 0.333 | 0.556 | 0.26 | 58.3 |
HAGOS: The Copenhagen Hip and Groin Outcome Score; RA: Rheumatoid arthritis.
Ultrasonographic findings of subclinical involvement of the hip in RA.
A) Normal hip (joint capsule parallel to the femoral cortex). B) Distension of the joint capsule. Patient with RA with no symptoms attributable to hip joint activity (group 2); ultrasonographic data of effusion and synovial hypertrophy were evident.
Table 4 shows the associations of asymptomatic and symptomatic RA groups with the demographic, clinical, and laboratory variables. Only the use of glucocorticoids was associated with the presence of lesions suggestive of OA (osteophytes + joint remodelling) in the subclinical group (p = 0.03).
Associations between US and demographic, clinical, and laboratory findings.
| Asymptomatic RA (n = 40) | Symptomatic RA (n = 37) | |||
|---|---|---|---|---|
| Distension of joint capsule | Lesions suggestive of coxarthrosis | Distension of joint capsule | Lesions suggestive of OAa | |
| Age | 0.10 | 0.87 | 0.35 | 0.54 |
| BMI | 0.76 | 0.22 | 0.78 | 0.99 |
| Disease duration (months) | 0.12 | 0.21 | 0.37 | 0.73 |
| Use of DMARDs | 0.28 | 0.17 | 0.80 | 0.23 |
| Use of glucocorticoids | 0.86 | 0.03 | 0.51 | 0.77 |
| Use of biologics | 0.55 | 0.86 | 0.15 | 0.87 |
| DAS28-CRP | 0.88 | 0.55 | 0.93 | 0.54 |
| HAQ | 0.09 | 0.77 | 0.24 | 0.76 |
| RF (IU/mL) | 0.77 | 0.28 | 0.22 | 0.28 |
| ESR | 0.27 | 0.50 | 0.96 | 0.07 |
| CRP (mg/dl) | 0.93 | 0.50 | 0.44 | 0.90 |
BMI: Body mass index; RA: Rheumatoid arthritis; DMARDS: Disease-modifying antirheumatic drugs; DAS: Disease Activity Score; CRP: C-reactive protein; HAQ: Health Assessment Questionnaire; RF: Rheumatoid factor; ESR: Erythrosedimentation rate.
Cohen's kappa coefficient showed acceptable agreement between ultrasonographers for the presence of osteophytes (0.34), moderate for joint remodelling (0.59), substantial for iliopsoas bursitis (0.66), and perfect for erosions (1.00), all with a significant level (p ≤ 0.0001).
DiscussionThe present study documented a subclinical prevalence of elementary lesions (joint capsule distension) of 20%, while the RA symptomatic group and healthy subjects presented a prevalence of 48.6% and 15%, respectively (p = 0.008). Previous publications have reported prevalences between 17% and 42%12,21; however, they included all patients with RA—whether they had symptoms or not. This study is the first to describe the prevalences independently. The reported prevalence is within the reference range mentioned in the background and is lower than the average calculated from the publications by Di Geso et al.14 and Koski15 (38%). The results demonstrate, once again, the value of US in early diagnosis in subclinical stages of the disease, particularly in the assessment of large joints, as demonstrated by Gutierrez et al.10 when determining the prevalence of subclinical involvement in the ankle joint in RA.
In agreement with the studies by Di Geso et al.14 and Chávez-López et al.,12 no significant associations were found between the US findings and the general activity of the disease, nor with the laboratory values. This study confirms that, despite its size, the participation of the hip joint in the inflammatory process can go unnoticed by the clinician until advanced stages, or in which morphostructural damage to the joint is already present.
The HAGOS questionnaire, which evaluated the different symptoms related to the hip joint (stiffness, pain, daily activities, sports, recreational, physical, and quality of life), showed significant differences between symptomatic patients (group 1) and asymptomatic patients (group 2). This reinforces the physical examination as a useful instrument to stratify patients.
The Koski measurement technique (described in 1989) has been used in different ultrasound studies12,14,15,21 and daily clinical practice by rheumatologists as a method of assessing suspected synovitis in the hip joint. However, in the present study, several limitations and technical difficulties were found in its application, such as patient biotype (the higher the BMI, the greater the difficulty in differentiating the structures of interest), the degree of pressure exerted with the probe (it was observed that with different degrees of pressure, the value of the measurement tends to vary), the low reproducibility, and the variability of the exact anatomical site of measurement. Soini et al.,22 who determined the value of the measurement technique by comparing it with magnetic resonance imaging (MRI), maintain that the US does not clearly distinguish the anatomical borders (tissue interfaces) of the joint capsule, the iliofemoral ligament, and synovial proliferation. On other occasions, the echogenicity of synovial proliferation and the iliofemoral ligament cannot always be differentiated, so the definition of synovitis from the Outcome Measures in Rheumatoid Arthritis Clinical Trials (OMERACT) group also poses difficulties in its application.
In the present publication, not only the measurement technique of Koski et al.18 was considered, but also other ultrasonographic features that point to the presence of distention of the joint capsule, which were already described by Qvistgaard et al.23 in 2006, through a semiquantitative scoring system in patients with OA, in which the presence of a hypoechoic layer within the joint capsule adjacent to the femoral neck is mentioned, as well as the rectification or convexity of the joint capsule concerning the femoral cortex (which should normally lie parallel). It is noteworthy that during data collection, four symptomatic patients with RA did not present joint capsule distension using the measurement technique of Koski et al.,18 but they did present ultrasonographic data that point to distension of the joint capsule. Fig. 2 describes a representative image of the distension of the joint capsule with a measure of less than 7 mm.
On the other hand, Soini et al.,22 in their comparative study (US vs. MRI) described a sensitivity of 87% and a specificity of 37%, with high values of false positives and false negatives (28 and 4, respectively) for the US, in 40 subjects with RA and ankylosing spondylitis. The same author mentions that it is possible to detect a minimal amount of normal synovial fluid in healthy subjects by MRI (from 1 to 2 mm thick), with a difference equal to or greater than 1 mm in 38% of healthy subjects with the US.
In our publication, four of the six healthy subjects who presented distension of the joint capsule presented differences equal to or greater than 1 mm between both hips; in this way, the finding described by Soini could explain our findings. In any case, the validity of this difference should be assessed through additional studies. On the other hand, the two healthy subjects who presented a measurement greater than 7 mm also showed ultrasonographic evidence of lesions suggestive of OA.
The OMERACT group defines an osteophyte as a bony prominence visible in two perpendicular planes.24,25 This definition is used in the present study, and a frequency of 20% is reported for the asymptomatic RA group, a higher value when compared to the other two groups. Epidemiological studies have established that a significant percentage of patients with OA are asymptomatic26; therefore, a high frequency of this elementary lesion in people between 40 and 70 years is expected. Similarly, the study by Di Geso et al.14 mentioned that there are no significant associations between the presence of osteophytes and hip joint pain. The study by Chávez-López et al.12 describes a frequency of 50.9% for the presence of osteophytes; however, the author used the definition described by Grassi et al.27 in 2004, who define osteophytes as bone irregularities in the articular margins. On this point, Qvistgaard et al.23 maintain that this manifestation occurs in the initial stages of the disease. The differences in frequencies between our work and that of Chávez-López are possibly due to the use of different definitions and the fact that the OMERACT definition is presented in more advanced stages of the disease.
Likewise, the OMERACT ultrasound group defines the presence of hyaline cartilage damage as loss of echogenicity or thinning with irregularities and less sharpness at its margins24,25; however, the adequate identification of this elementary lesion is difficult in deep joints, especially in obese individuals. In the present publication, it was decided to use the term joint remodelling, defined as a flattening or loss of sphericity of the visible portion of the femoral head, which was already described in the OA scoring system by Qvistgaard et al.23 to define the presence of a reparative phenomenon of endochondral ossification, typical of ball and socket joints. Said abnormality was documented with a frequency of 27.5% in the asymptomatic RA group, 13.5% in the symptomatic RA group, and 2.5% in the group of healthy individuals. On the other hand, Di Geso et al.14 indicated a frequency of 32% for hyaline cartilage damage, while Chávez-López et al.12 —as in our series— did not include this elemental lesion.
The number of patients who presented erosions was very low (only two hips in the symptomatic RA group), unlike the studies by Di Geso et al.14 and Chávez-López et al.,12 which reported 10 and 6 hips, respectively. We believe that the identification of this elementary lesion in the hip joint also presents difficulties, such as the presence of an acoustic shadow caused by osteophytes, and the fact of observing only a part of the femoral head and neck. Unlike the small joints of the hands and feet, the US is not an ideal tool for their identification in large joints located in deep anatomical planes and with a limited acoustic window.
Di Geso et al.14 did not describe the presence of iliopsoas bursitis14 in their cohort, while Chávez-López et al.12 reported a very low frequency (only two affected hips). In our study, in the same way, a frequency of only three affected hips was observed. Both frequencies are very low, and it is striking that they only occur in asymptomatic people.
This study should be interpreted under the following limitations:
- 1)
The use of a linear probe, with frequencies of 6–12 MHz in all patients, undoubtedly influenced the measurement of the joint capsule, considering that Backhaus et al.19 recommend the use of low-frequency probes, from 3.5 to 5 MHz, in deep joints, depending on the physical constitution of the patient.
- 2)
The age of patients with RA and healthy subjects places them within the epidemiological group susceptible to OA.
- 3)
The lack of a gold standard to compare our findings.
- 4)
The study design allowed the inclusion of patients with different types of treatments—including DMARDs, biologics, and glucocorticoids—that could influence the subclinical status of the hip joint.
Finally, the present work provides new data that, to date, had not been studied and published:
- 1)
The ultrasonographic prevalence of distention of the joint capsule in patients with subclinical RA.
- 2)
The value of ultrasonographic findings other than the Koski measurement technique in the assessment of synovitis in the hip joint.
- 3)
Limitations and difficulties in the applicability of the OMERACT group definitions of synovitis, hyaline cartilage damage, and hip joint erosions.
- 4)
The presence of distension of the iliopsoas bursa in an asymptomatic population suggests new points that can be clarified in subsequent studies.
The present study determined a prevalence of subclinical involvement of the hip in RA through the US, which is lower compared to symptomatic patients and higher when compared to healthy individuals, which reaffirms the value of the US in the subclinical diagnosis of inflammatory disease (joint capsule synovitis) of the hip joint. However, the Koski measurement technique presented several limitations and difficulties (lack of reproducibility in the exact measurement with a higher degree of obesity and greater difficulty in differentiating the anatomical structures of interest at various degrees of probe pressure, since the measurement values tend to change). Therefore, it is necessary to consider other ultrasonographic abnormalities for an adequate assessment. As in previous publications, no significant associations were found between the US findings and the clinical activity of the disease, nor with laboratory results.
FinancingNo funding source was received.
Conflict of interestsNo conflicts of interest are declared.
The authors thank the Research Support Unit of the Luis Guillermo Ibarra National Rehabilitation Institute for the methodological advice received.