Determinar las complicaciones durante el postoperatorio en Reanimación y analizar qué variables del receptor, donante y quirúrgicas se asocian a complicaciones mayores.
Material y métodoAnalizamos una serie de trasplantes cardiacos ortotópicos consecutivos realizados en nuestro centro entre 2001-2007. Se compararon pacientes que no presentaron complicaciones mayores (CM) durante la estancia en Reanimación (Grupo 1) con los que sí las desarrollaron (Grupo 2). Se consideró CM el exitus, fallo primario del injerto (FPI), infección grave y necesidad de hemodiálisis.
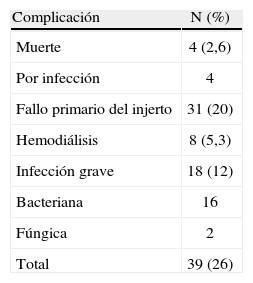
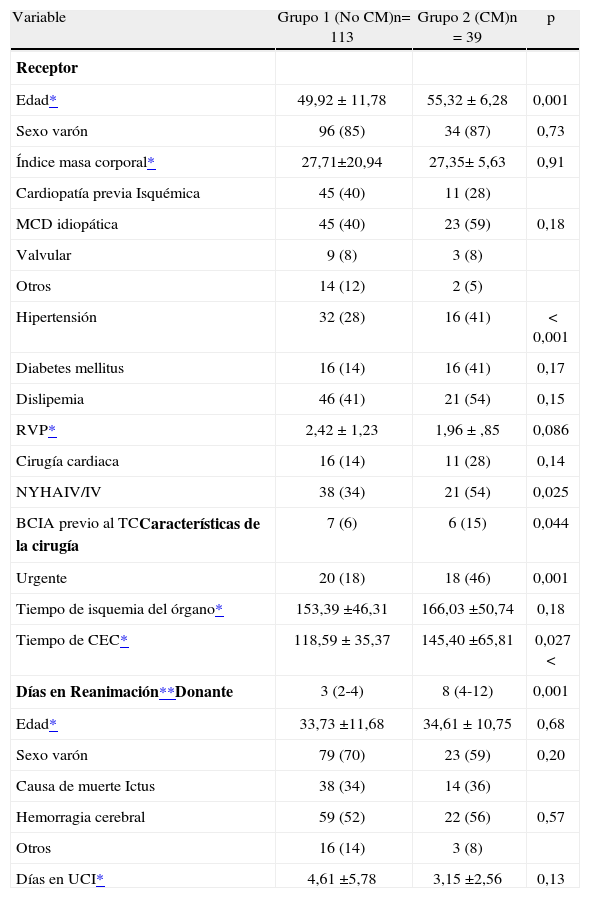
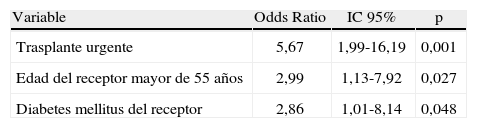
ResultadosIncluimos 152 pacientes cuyo tiempo de permanencia en Reanimación fue de 3 (2,25-5) días. Ciento trece pacientes no presentaron CM en Reanimación (Grupo 1), mientras que 39 pacientes (26%) sí desarrollaron complicaciones (Grupo 2): FPI (20%), infección (12%) y disfunción renal grave (5,3%). Observamos diferencias significativas entre los grupos respecto a edad (50±12 vs 55±6; p=0,001), diabetes (14 vs. 41%; p=0,0001), clase funcional New York Heart Association IV/IV (34 vs. 54%; p=0,04), trasplante urgente (18 vs 46%; p=0,001), tiempo de circulación extracorpórea (119±35 vs. 145±66 minutos; p=0,03), balón de contrapulsación pretrasplan-te (6 vs 15%; p=0,04). El análisis multivariado demostró asociación entre las CM y el trasplante urgente (OR: 5,67; p=0,001), receptor mayor de 55 años (OR: 2,99; p=0,027) y diabético (OR: 2,86; p=0,048).
ConclusionesUn 26% de los pacientes cardiacos desarrollaron CM en Reanimación. Las más frecuentes fueron el FPI, la infección y la disfunción renal grave. Son variables predictivas independientes de su aparición el trasplante urgente, edad y diabetes mellitus del receptor.
To assess the incidence of major complications in the postoperative recovery unit and to analyze the associated recipient, donor, and surgical risk factors.
Material and methodsWe studied a series of consecutive orthotopic heart transplants carried out in our hospital from 2001 through 2007. Patients who experienced major complications during their stay in the recovery ward were compared with those who did not. Exitus, primary graft failure, severe infection, and need for hemodialysis were considered major complications.
ResultsOne hundred fifty-two patients were enrolled. The mean stay in the recovery unit was 3 days (range, 2.25-5 days). Thirty-nine patients (26%) developed major complications in the recovery unit and 113 did not. The complications were primary graft failure (20%), infection (12%), and acute renal failure (5.3%). Patients with and without major complications were significantly different with respect to mean (SD) age (55 [6] vs 50 [12] years, respectively; P=.001), presence of diabetes mellitus (41% vs 14%, P=.0001), classification in New York Heart Association functional class IV/IV status (54% vs 34%, P=.05), emergency transplantation (46% vs 18%, P=.001), mean cardiopulmonary bypass time (145 [66] vs 119 [35], P=.03), pretransplant use of an intra-aortic balloon pump (15% vs 6%, P=.04). Multivariate analysis demonstrated an association between major complications and emergency transplantation (OR, 5.67; P=.001), recipient age over 55 years (OR, 2.99; P=.027), and diabetes mellitus (OR, 2.86; P=.048).
ConclusionsThe incidence of major complications in our postoperative recovery unit was 26%. The most common complications were primary graft failure, infection, and acute renal failure. Emergency transplantation, older age, and a diagnosis of diabetes mellitus in the recipient were predictors of complication.