The current SARS-CoV-2 pandemic has been the world's largest socio-health crisis experienced in the last century. Each healthcare center has been compelled to adapt the treatment guidelines established by the different scientific societies.
ObjectiveAnalyze the impact of the methodology based on simulation as a tool to improve our clinical practice: work dynamics, effectiveness and safety of all the physicians involved in the management of labor in COVID pregnant women and its usefulness to facilitate the adaptation of protocols to a specific clinical context.
MethodDescriptive observational study that includes the C-sections and deliveries of COVID pregnant women performed in our hospital. The actions carried out in each procedure were analyzed using the simulation multidisciplinary briefing and debriefing tools, before and after each case.
ResultsA total of 5 clinical cases were analyzed. Difficulties were found in the execution of the protocols established for the care of the COVID pregnant. Organizational, structural, material resources and human factors obstacles were the most common.
ConclusionsOur results showed that the analysis example using simulation methodology was a tool of great value in three aspects: teamwork improvement, actions consent and improvement proposals for the adaptation and implementation of protocols.
La pandemia actual de SARS-CoV-2 ha supuesto la mayor crisis socio-sanitaria mundial experimentada en el último siglo. Cada centro asistencial se ha visto impelido a adecuar las guías de tratamiento establecida por las distintas sociedades científicas.
ObjetivosAnalizar el impacto de la metodología basada en la simulación como herramienta de mejora de nuestra práctica clínica: dinámica de trabajo, efectividad y seguridad de todos los facultativos implicados en el manejo del parto en gestantes COVID y su utilidad para facilitar la adecuación de los protocolos, a un contexto clínico específico.
MétodoEstudio observacional descriptivo que incluye las cesáreas y partos de gestante COVID realizados en nuestro hospital. Se analizaron de manera multidisciplinar las actuaciones ejecutadas utilizando las herramientas de la simulación briefing y debriefing, antes y después de cada caso.
ResultadosSe analizaron un total de 5 casos clínicos. Se encontraron dificultades en la ejecución de los protocolos establecidos para la atención de la gestante COVID a nivel organizativo, estructural, de recursos materiales y de factores humanos.
ConclusionesEste modelo de análisis ha resultado una herramienta de gran valor en tres aspectos: la mejora del trabajo en equipo, la realización de protocolos de actuación consensuados y el establecimiento de propuestas efectivas para la adecuación de los protocolos.
The current SARS-CoV-2 pandemic has been the largest global public health crisis this century. It has compelled us to redefine health models, prevention protocols, diagnosis, strategies and treatment.1 All healthcare centres have had to tailor the treatment guidelines established by the health authorities2 and/or scientific societies3 to the ongoing changes in their local capacity and resources, while our scientific knowledge of the disease4 and our experience in treating it increases.
One of the most complex scenarios to protocolize in this context is the management of the obstetric patient, as different units are involved: maternal-foetal units, ultrasound units, the delivery area, the surgical suite, and puerperium units. To this is added the limitations of RT-PCR screening, where waiting times can sometimes be longer than the delivery itself, and a weak viral load or incorrect sampling can yield false negatives.5
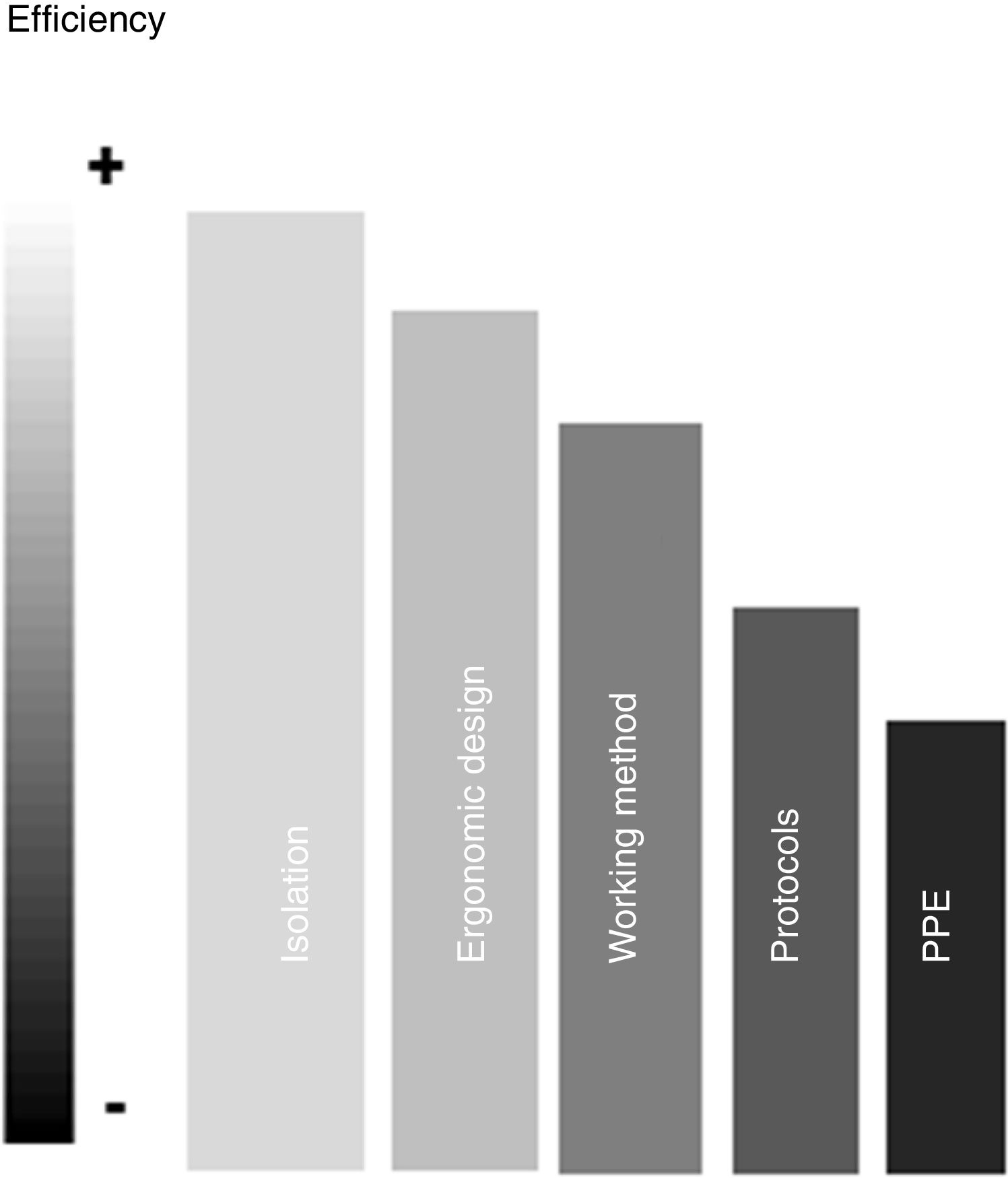
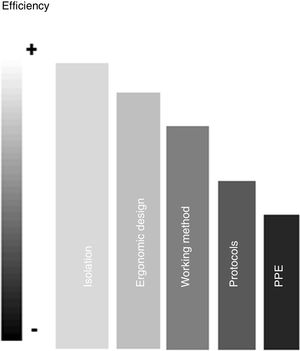
Most of the considerations set out in protocols for the management of pregnant woman with suspected or known SARS-CoV-2 infection include strategies to ensure maternal care and prevent infection in health personnel. The latter involves several different levels (Fig. 1), not only the use of personal protective equipment (PPE).
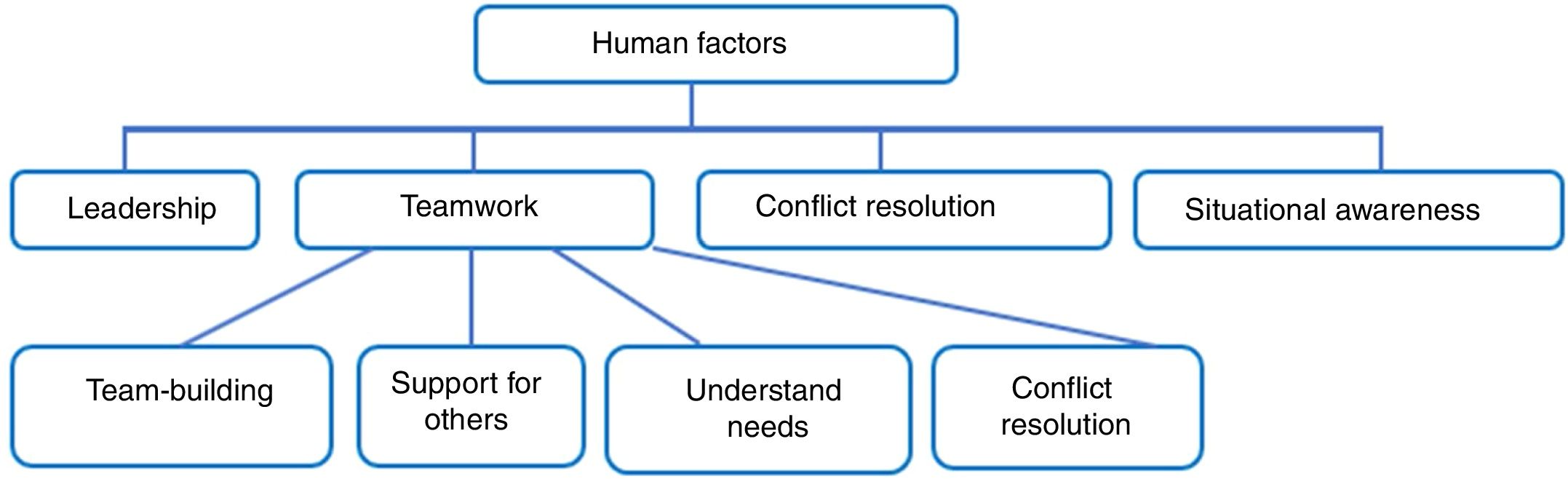
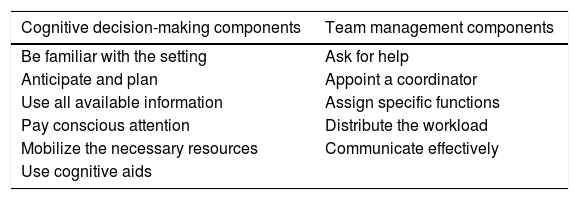
In fact, the heterogeneous, unforeseeable and complex situations that can occur in this context are often not addressed in clinical guidelines and protocols, making it necessary to adapt these recommendations to the circumstances arising at any given time. This calls for rapid, accurate, decision-making by the entire multidisciplinary team involved. In this regard, simulation provides functional models of the cognitive processes that are suitable for dynamic decision making6 (Table 1) and the management of human factors7 (Fig. 2).
Functional elements that facilitate dynamic decision-making.
| Cognitive decision-making components | Team management components |
|---|---|
| Be familiar with the setting | Ask for help |
| Anticipate and plan | Appoint a coordinator |
| Use all available information | Assign specific functions |
| Pay conscious attention | Distribute the workload |
| Mobilize the necessary resources | Communicate effectively |
| Use cognitive aids |
Human factors involved in teamwork dynamics.7.
The methodology used in simulation-based clinical training, such as briefing and debriefing,8 can facilitate group coordination and detect the weak points in a particular activity. Difficulties detected and successfully resolved can be studied using the type of root cause analysis9 used in clinical simulation, and can be used to establish proposals for improvement in established protocols.
ObjectivesTo determine whether clinical simulation methodology (briefing and debriefing) can be used to adapt protocols to a specific clinical context, and to examine their use as a tool to improve clinical practice, including work flows, effectiveness, and safety of all clinicians involved in the management of COVID-19 patients during childbirth.
Material and methodsWe describe 5 cases of pregnant COVID patients treated in our hospital consecutively between 24 March and 11April 2020, including emergency and scheduled caesarean sections and deliveries. The team in charge of the patient that day collected data related to the difficulties encountered implementing the protocol. Clinical simulation methodology was used, starting with a multidisciplinary briefing before the procedure, followed by a post-procedure debriefing in which the teams actions were analysed using gather-analyse-summarize (GAS) methodology. The conclusions reached were drafted into improvement proposals that have been submitted to the hospital’s COVID working group for evaluation and possible inclusion in the latest version of the hospital’s protocol.
ResultsCase 1: «Although many believe there is one team, this does not always seem to be the case»A 23-year-old patient at 36+ 2 weeks of gestation (WOG) who came to the emergency room with fever, headache, odynophagia and dry cough. Given the current context, she was screened for SARS-CoV-2, which was positive, and was admitted to the COVID ward of our hospital (Tower D, floor 7) to monitor her evolution. Three days later, due to the persistence of fever and worsening labs, she was scheduled for priority caesarean section according to our institutional protocol. She had to be transferred from the COVID ward to the maternity unit (Tower B, floor 1) using specific routes for COVID patients. The caesarean section was performed by the on-call team using subarachnoid anaesthesia, with no notable maternal or neonatal incidents. Post-anaesthesia monitoring was performed in the operating room, and the patient was then returned to the COVID ward.
GatherEven though this was our first case, we had enough time to plan the scenario as it was a priority caesarean section. One of the anaesthesiologists involved led a multidisciplinary briefing session to prepare and coordinate the team. The transfer routes and action protocol established for this type of patient were reviewed, allowing the team to detect discrepancies and unify criteria. Following this, a checklist of the material, drugs and PPE needed was drawn up, for which the previously prepared checklists were very useful.
AnalyseDespite the use of specific lists of drugs and material for COVID patients, some items were missing, and the doors to the surgical suite had to be opened repeatedly. Although the material and drugs were laid out on specific tables, they were insufficiently isolated, so all unused material had to be discarded due to possible exposure to contamination.
Our initial protocol called for 14 people to perform the COVID caesarean section, 7 in the operating room for direct care of the patient and infant, and another 7 on stand-by in the surgery anteroom. This was wasteful in terms of both time and resources, and also hampered PPE donning and doffing. On-duty mobile phones are not allowed in the operating room, and the absence of an alternative communications systems, meant that the surgical team was unable to communicate directly with the anteroom team. More than 5 h were needed for surgery, post-anaesthesia monitoring, ventilation, cleaning and disinfection, during which time the operating room was unavailable for any other obstetric emergency. Wearing PPE for such a long time was exhausting, so the final transfer of the patient to the COVID ward was carried out by the anteroom support staff and not the anaesthesiologist involved, as required in the protocol. During the procedure, the need for an emergency NON COVID caesarean section arose, which had to be performed in a suitably sterile room in the delivery area with a midwife acting as a surgical nurse until a surgical nurse from the central surgical suite was able to join the team. Even though this eventuality is included in the institutional protocol, it was not taken into account until the emergency arose.
Case 2: «There are many barriers against effective interdisciplinary collaboration. Leadership and hierarchies must be recognized and accepted»A woman at 38+ 3 WOG had been scheduled for caesarean section in a private hospital. On admission, she presented symptoms of anosmia and SARS-CoV-2 testing was positive. She was referred to our hospital and admitted to the COVID ward. After consulting the Obstetrics and Gynaecology Service, it was decided to schedule an priority caesarean section.
GatherOnce again, we had to perform a priority caesarean section in a pregnant COVID patient. However, this situation differed slightly from the preceding case insofar as we were able to draw on previous experience, and luckily one of the anaesthesiologists who had participated in the first case conducted the initial multidisciplinary briefing in which the team went over transfer and procedure protocol, including the changes introduced after our experience with the first case.
AnalyseOur standard surgical practice is conceived as an aggregate of individual teams (gynaecologists, anaesthesiologists, nurses, midwives, etc.) participating in the same procedure. This is not synonymous with teamwork, so we decided to appoint a coordinator - a clinician capable of pulling the individual team members together to achieve the previously agreed common objectives. Once the coordinator had been appointed, our first priority was to ensure the safety of team members by minimizing exposure. Thus, the protocol was modified and the group directly involved was reduced to 9 professionals, with the rest remaining in standby This allowed us to reduce the number of PPEs needed, the preparation time, and the number of people exposed. Communication difficulties were resolved by using mobile phones encased in plastic. To avoid re-entering the operating room and donning a PPE, the anaesthesiologist and one of the gynaecologists remained in the operating room during preliminary post-anaesthesia monitoring in case immediate complications arose. To free up the operating room earlier, the patient received “express” post-anaesthesia care, and the entire process, including ventilation and cleaning, took only 3 h. Particular importance was given to the correct removal of PPE, which was supervised by the coordinator in all cases, particularly less trained staff members such as assistants and cleaning staff, who continue working when everyone else has left the surgical suite.
Case 3: «Doctors are willing to delegate a task but not to delegate decision-making»A woman at 37+ 5 WOG, with a history of fever, malaise, myalgia, and dry cough. A nasal smear taken in the Emergency Room was positive for SARS-CoV-2. She was admitted for evolutionary control and treated with lopinavir/ritonavir. Foetal progress was satisfactory, and on the fourth day, afebrile and asymptomatic, she was discharged. The test was repeated after 14 days, and continued positive. She was told to continue isolation at home, but the next day she presented to the emergency room in labour, fully dilated.
GatherThere was some initial confusion due to the urgency of the situation and uncertainty about whether strict adherence to our pregnant COVID patient protocol was required in this scenario. According to our protocol, vaginal delivery should be performed in the COVID ward when dilation is greater than 5 cm. When this is not the case, a caesarean section was indicated. In this patient, who was fully dilated and ready to push, we believed that transferring the mother, the material and the medical team (midwives, assistants, gynaecologists, anaesthesiologist and neonatologist) from the maternity unit to the COVID ward would endanger maternal-foetal safety due to the real risk of precipitated delivery in the middle of the transfer process. At this point, as it was not possible to perform vaginal delivery in the obstetrics room because it was not equipped with a COVID area, the gynaecological emergency team decided to perform urgent caesarean section in the obstetric operating room and avoid transfer.
AnalyseThe urgency of the situation made it impossible to appoint a coordinator, although the team agreed on the basic strategy. The anaesthesia team lacked the recognized and accepted authority to coordinate the team, so it acted once again as an aggregate of individual working groups. The immediate outcome was confusion about how many people should be available for the emergency, and all were considered equally essential. The lack of coordination made it difficult to redistribute PPE, especially FFP3 masks. Shortage of some protective equipment (face screens), and the resulting fear of infection among the team led to an individual dynamic instead of members pairing up to help/supervise donning of PPE. This prolonged the donning procedure and delayed the start of surgery. Although previous experience facilitated and speeded up the preparation of trays of standard and emergency drugs, there was insufficient time to isolate much of the anaesthetic material, and it had to be discarded due to the risk of contamination. The urgency of the situation, the mother’s unwillingness to undergo caesarean section, and her concerns about being separated from the infant left her in a state of anxiety that made it difficult to perform the neuraxial technique. After post-anaesthesia care in the operating room, the mother was transferred to the COVID ward where she was followed up by Internal Medicine, supported by Gynaecology.
Case 4: «Communication is the most important tool in solving professional questions in a team construct»A woman at 38+ 5 WOG was admitted to our delivery room in labour with 2 cm cervical dilation. Following our protocol, the epidemiological questionnaire was administered, which was negative, and RT-PCR for SARS-CoV-2 was requested. Before the test results were received the patient required epidural analgesia, which was performed using all the protective measures indicated in the COVID protocol for indeterminate cases. Later, the patient's smear was reported to be positive.
GatherInitial bewilderment, disbelief and concern: Had the appropriate protective measures been taken at each stage of the procedure? How should we proceed when our pregnant patient was already fully dilated? Was caesarean section justified, given the favourable conditions for vaginal delivery?
The first step was to bring the team together for a briefing session to jointly decide how the situation should be managed. Luckily, both anaesthesiologists previously involved in COVID cases were present, we were able to draw on the experience gained in the preceding case, and new evidence had emerged on the indications for childbirth in COVID patients. We then contacted the head of the Gynaecology Service to inquire about the possibility of performing a vaginal delivery, and in consensus with the duty supervisor and the duty head nurse a strategy was developed and an appropriate team was put on stand-by to respond to another situation, if needed.
AnalyseAfter confirming that the patient was fully dilated, we decided not to transfer her to the COVID ward and instead to directly change the protocol and perform the delivery in the delivery room. Initially, her room was isolated from the surrounding rooms in an attempt to minimise horizontal contamination. An anaesthesiologist was appointed coordinator, and his first priority was to change the approach to the procedure in order to ensure the safety of all concerned and minimise staff exposure. Accordingly, the intervention team was reduced to 3 members (gynaecologist, midwife and nursing assistant). This team, equipped with PPE, performed a vaginal delivery in the delivery room, while the other anaesthesiologist, gynaecologist, neonatologist, midwife and nursing assistant remained on standby outside the isolated room. A commercial video/audio baby monitor was used to allow both teams to communicate during the procedure.
Finally, the coordinator supervised the correct placement and removal of PPE for all the personnel involved and the collection of waste from the obstetric area.
Case 5: «Interdisciplinary decision-making requires special skills»Primipara at 40+1 WOG who went to the emergency room in the early stages of labour. She was transferred to the maternity unit, evaluated, and finally sent home after completing an epidemiological questionnaire and providing a SARS-CoV-2 RT-PCR smear. She returned 5 h later when the PCR tests results were available, which turned out to be positive for SARS-CoV-2, so she was admitted to the COVID ward for isolation and monitoring of dilation, expulsion and puerperium. After 2 h of labour, epidural analgesia to control labour pain was requested.
AnalyseThe protocol for treating pregnant patients with COVID specifies that material and drugs required for labour analgesia should be provided in the isolation room, so in this case analgesia administration outside the obstetric area was indicated. After 8 h of labour, when the patient had entered the expulsion stage, the gynaecological team decided that it would be safer to transfer her to the operating room in the obstetric area for delivery.
AnalyseWhen the anaesthesiologist was preparing to administer the analgesia, it became clear that the minimum material and drugs needed for this purpose were not available in the room. Even though they were clearly defined in the care protocol, they were not transferred from the obstetric area. During expulsion, the gynaecologist, in the interests of clinical safety, unilaterally decided to modify the established procedure. The absence of a pre-procedural briefing to coordinate management of the situation, the lack of experience needed to take on a leadership role and coordinate, assign tasks, limit the number of staff involved, and facilitate decision-making, created confusion in the COVID ward and during transfer to the obstetric area, causing unnecessary overexposure of both staff and material to contamination.
Incorrect separation of the areas put the entire obstetric operating suite at risk of contamination, and it had to be cleaned and disinfected. This again meant that the operating room had to be sealed for more than 6 h. This case compelled hospital management to rethink the care model for pregnant patients with COVID in our hospital. The result was the creation of an isolated obstetric COVID area within the delivery room, equipped with all the necessary obstetric material resources. Here, COVID patients undergoing vaginal delivery can be treated or monitored during dilation, expulsion and post-delivery without the need to transfer staff and materials.
DiscussionThe use of simulation-based training in the healthcare sector has increased exponentially in the last 20 years. In the present context, we use simulation to teach health personnel to don and doff PPE, to train clinicians in safe airway management techniques, to train non-anaesthesiologists to perform alveolar recruitment and lung protective ventilation techniques, and to rehearse position changing techniques, among other activities.
A fundamental part of simulation-based learning is the debriefing held after the training session. Conceptually, debriefing, originally a military term, refers to the process in which participants systematically go through the events that occurred after a mission has been completed in order to draw conclusions and review the lessons learned. However, its effectiveness in improving learning after real-world situations has yet to be explored in different organizations.10
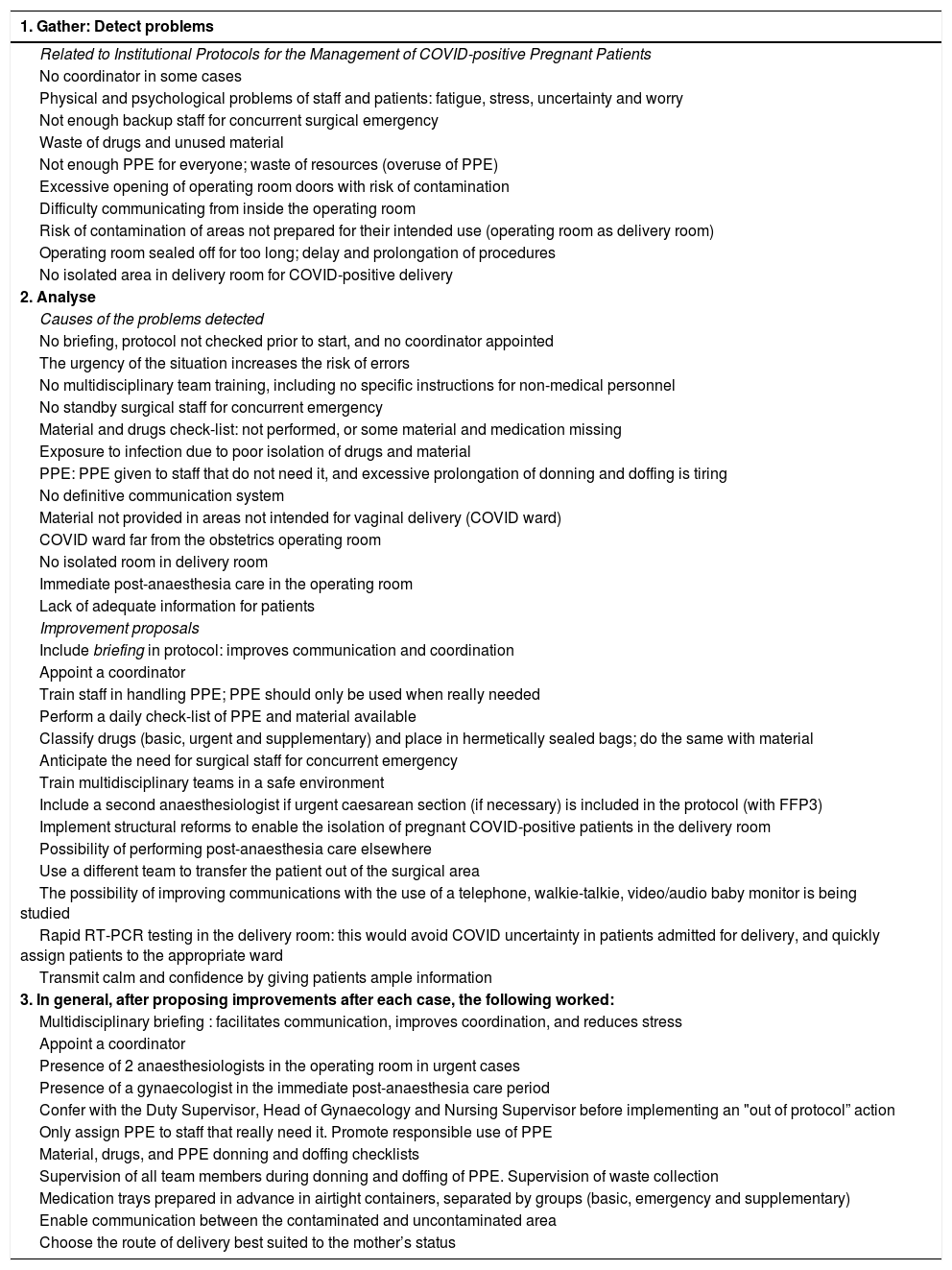
Based on our extensive experience in simulated environments and teaching methodology,11 we used a simulation-based technique to evaluate our own approach (Table 2) to handling the different situations arising in a context as variable and dynamic as childbirth during the COVID-19 pandemic.
Gather and Analyse. Detect problems and their causes, and propose improvements.
| 1. Gather: Detect problems |
|---|
| Related to Institutional Protocols for the Management of COVID-positive Pregnant Patients |
| No coordinator in some cases |
| Physical and psychological problems of staff and patients: fatigue, stress, uncertainty and worry |
| Not enough backup staff for concurrent surgical emergency |
| Waste of drugs and unused material |
| Not enough PPE for everyone; waste of resources (overuse of PPE) |
| Excessive opening of operating room doors with risk of contamination |
| Difficulty communicating from inside the operating room |
| Risk of contamination of areas not prepared for their intended use (operating room as delivery room) |
| Operating room sealed off for too long; delay and prolongation of procedures |
| No isolated area in delivery room for COVID-positive delivery |
| 2. Analyse |
| Causes of the problems detected |
| No briefing, protocol not checked prior to start, and no coordinator appointed |
| The urgency of the situation increases the risk of errors |
| No multidisciplinary team training, including no specific instructions for non-medical personnel |
| No standby surgical staff for concurrent emergency |
| Material and drugs check-list: not performed, or some material and medication missing |
| Exposure to infection due to poor isolation of drugs and material |
| PPE: PPE given to staff that do not need it, and excessive prolongation of donning and doffing is tiring |
| No definitive communication system |
| Material not provided in areas not intended for vaginal delivery (COVID ward) |
| COVID ward far from the obstetrics operating room |
| No isolated room in delivery room |
| Immediate post-anaesthesia care in the operating room |
| Lack of adequate information for patients |
| Improvement proposals |
| Include briefing in protocol: improves communication and coordination |
| Appoint a coordinator |
| Train staff in handling PPE; PPE should only be used when really needed |
| Perform a daily check-list of PPE and material available |
| Classify drugs (basic, urgent and supplementary) and place in hermetically sealed bags; do the same with material |
| Anticipate the need for surgical staff for concurrent emergency |
| Train multidisciplinary teams in a safe environment |
| Include a second anaesthesiologist if urgent caesarean section (if necessary) is included in the protocol (with FFP3) |
| Implement structural reforms to enable the isolation of pregnant COVID-positive patients in the delivery room |
| Possibility of performing post-anaesthesia care elsewhere |
| Use a different team to transfer the patient out of the surgical area |
| The possibility of improving communications with the use of a telephone, walkie-talkie, video/audio baby monitor is being studied |
| Rapid RT-PCR testing in the delivery room: this would avoid COVID uncertainty in patients admitted for delivery, and quickly assign patients to the appropriate ward |
| Transmit calm and confidence by giving patients ample information |
| 3. In general, after proposing improvements after each case, the following worked: |
| Multidisciplinary briefing : facilitates communication, improves coordination, and reduces stress |
| Appoint a coordinator |
| Presence of 2 anaesthesiologists in the operating room in urgent cases |
| Presence of a gynaecologist in the immediate post-anaesthesia care period |
| Confer with the Duty Supervisor, Head of Gynaecology and Nursing Supervisor before implementing an "out of protocol” action |
| Only assign PPE to staff that really need it. Promote responsible use of PPE |
| Material, drugs, and PPE donning and doffing checklists |
| Supervision of all team members during donning and doffing of PPE. Supervision of waste collection |
| Medication trays prepared in advance in airtight containers, separated by groups (basic, emergency and supplementary) |
| Enable communication between the contaminated and uncontaminated area |
| Choose the route of delivery best suited to the mother’s status |
Although we are unsure of the exact role played by debriefing in improving clinical practice12 or patient outcomes, in our hands it has turned out to be an extremely valuable tool for improving communication, a fundamental element in the management of team dynamics12 and consensus protocols.
For example, as can be seen in the cases presented, one of the most controversial issues among clinicians was where to place women in labour. In taking this decision, specific clinical criteria for infectious patients took precedence over other factors, such as pregnancy. The problem lies in the fact that a pregnant women is not the same as a parturient, and when the pregnant patient is about to give birth, the route of delivery must be arranged. When the room set aside for this purpose is located in a ward as far from the maternity unit as the COVID ward is in our hospital, a significant amount of material and human resources needs to be transferred to control the process and deliver the infant. The combination of fear of infection and unfamiliarity with the setting clearly undermined patient safety and the quality of care13 provided.
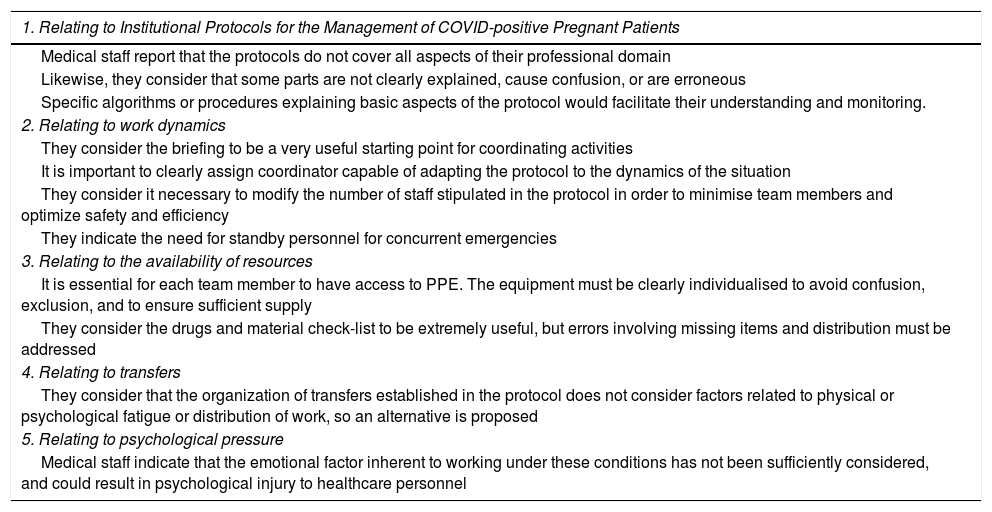
Gathering team members together in a small pre-procedure briefing session proved to be the key to detecting discrepancies, unifying criteria and improving team coordination.14 After the procedure, analysing and discussing the events, our performance, the lessons learned individually, as a team, and as a system with the team involved was extremely beneficial15 and helped establish proposals for improving existing protocols. Some of these were obvious enough to compel management to rethink the model of care for the pregnant COVID patient and create an isolated COVID area within the delivery room, where dilation and delivery can be monitored and post-vaginal delivery care given to pregnant women with COVID (Table 3).
Main conclusions drawn during the debriefing of clinical cases.
| 1. Relating to Institutional Protocols for the Management of COVID-positive Pregnant Patients |
|---|
| Medical staff report that the protocols do not cover all aspects of their professional domain |
| Likewise, they consider that some parts are not clearly explained, cause confusion, or are erroneous |
| Specific algorithms or procedures explaining basic aspects of the protocol would facilitate their understanding and monitoring. |
| 2. Relating to work dynamics |
| They consider the briefing to be a very useful starting point for coordinating activities |
| It is important to clearly assign coordinator capable of adapting the protocol to the dynamics of the situation |
| They consider it necessary to modify the number of staff stipulated in the protocol in order to minimise team members and optimize safety and efficiency |
| They indicate the need for standby personnel for concurrent emergencies |
| 3. Relating to the availability of resources |
| It is essential for each team member to have access to PPE. The equipment must be clearly individualised to avoid confusion, exclusion, and to ensure sufficient supply |
| They consider the drugs and material check-list to be extremely useful, but errors involving missing items and distribution must be addressed |
| 4. Relating to transfers |
| They consider that the organization of transfers established in the protocol does not consider factors related to physical or psychological fatigue or distribution of work, so an alternative is proposed |
| 5. Relating to psychological pressure |
| Medical staff indicate that the emotional factor inherent to working under these conditions has not been sufficiently considered, and could result in psychological injury to healthcare personnel |
In real life, as in the simulated environment, one of the most difficult elements to define was the figure of the procedure coordinator. The coordinator must be the person capable of providing the members of an organization with the resources, motivation and values they need to achieve previously agreed objectives. He or she must possess a series of qualities: ability to trouble-shoot problems as they arise, ability to clearly convey how to achieve the goals defined, and ability to convince other people to accept their guidance in this regard.
Teams generally find it very difficult to appoint a coordinator. The reasons for this are diverse, and include: the interaction of various highly specialised teams working together but independently16; difficulties in communication and information transfer; reluctance to share responsibilities; and unwillingness to delegate decisions that clinicians consider to be part of their specialty. As a result, it was not always possible to choose a coordinator capable of facilitating interdisciplinary communication and coordination, and this was one of the factors that had the greatest impact on the outcome of the procedure.
Finally, insufficient consideration was given to human emotions, such as fear of infection. This could have influenced people’s actions, and could even have left sequelae that could lead to psychological trauma17 among staff members. Forums, such as Schwartz Center Rounds,18 allow healthcare workers to share their experiences and receive emotional support.
ConclusionsOur experience with COVID-positive pregnant patients has shown that the methodology used in simulation-based training can be extrapolated to the management of real-life situations,19 and is subject to the same difficulties found in simulated environments.
Briefing sessions held before each case were very useful for improving important aspects of teamwork, such as communication and coordination of a multidisciplinary team.20 It also helped to appoint a coordinator, who plays a fundamental role in adapting existing protocols to the reality of the dynamic, ever-changing clinical context.21
Holding a post-procedure debriefing session to analyse the team’s actions and the difficulties encountered allowed us to draw up proposals for improving existing protocols.22 This ultimately led to the creation of an isolated COVID area within the delivery room and improved the quality and safety of maternal-foetal care. The cases described also highlight the need for fast-track PCR testing with results in less than 1 h in pregnant women in labour. This enabled us to rapidly assign pregnant women to COVID or non-COVID rooms within the delivery room, and allowed staff members to take the appropriate protective measures.
Conflict of interestsThe authors declare that they have not received any funding for the research or the preparation of the manuscript.
Special thanks go to Dr. Sergio Maldonado, a great professional and an even greater person - with our best wishes.
We also thank Dr. José María Maestre, head of teaching at the Valdecilla Virtual Hospital, for his critical reading of the manuscript and his help in editing the text.
Please cite this article as: González AM, Hernández Pinto P, Maldonado S, Villalobos I, Sierra N, Melgosa I. Análisis del protocolo de atención a las gestantes COVID y detección de puntos de mejora aplicando metodología de simulación clínica. Rev Esp Anestesiol Reanim. 2020. https://doi.org/10.1016/j.redar.2020.07.010