Developmental dysplasia of the hip (DDH) is a condition which comprises a number of joint abnormalities, including modifications in femoral version and neck-shaft angle (CCD), as well as a probable progression to osteoarthritis in certain cases. The main objective of this research was to find a correlation between femoral version and severity of DDH in patients with advanced osteoarthritis prior to joint replacement, which has not been previously reported. A secondary aim was to describe the modification of CCD as the severity of DDH increases.
Materials and methodPatients over the age of 15 with dysplastic hips and severe osteoarthritis prior to total hip arthroplasty were assessed between March 2018 and February 2019. Cases with any previous hip surgery were excluded. Anteroposterior pelvis X-rays and femoral computed tomography (CT) were performed; femoral version was measured in CT and CCD was evaluated both in X-rays (2 observers: A and B) and CT (one observer: musculoskeletal radiologist). Severity of DDH was defined by observers A and B according to Crowe classification in X-rays. Statistical analysis was performed on SPSS v.21. Shapiro–Wilk test was used to confirm a normal data distribution. Intraclass correlation coefficient (ICC) determined the level of agreement between observers A and B. Pearson test assessed the correlation between femoral version and Crowe classification (positive if >0.5). Student's t test evaluated the statistical significance, which was defined as P<0.05.
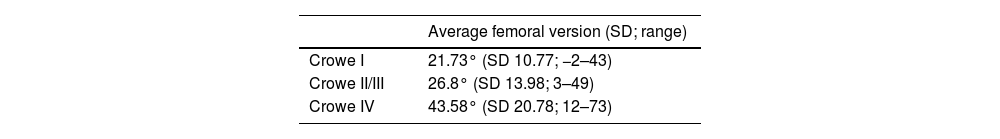
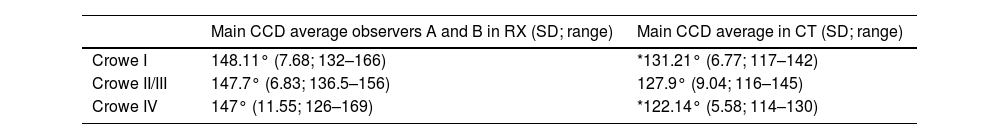
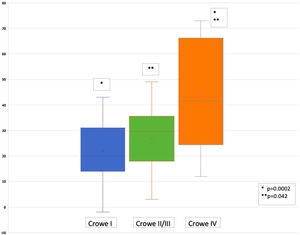
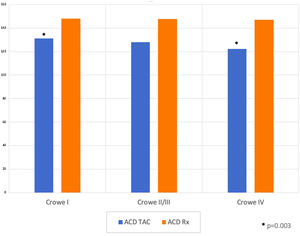
ResultsOne-year assessment; 42 patients (54 hips), 76% women. Mean age 52.7 years. 45 hips completed the imaging set, 9 hips were assessed only with X-rays. 48%, 16%, 7% and 28% were classified as Crowe I, II, III and IV (100% interobserver agreement). Crowe classes were grouped as I, II/III and IV due to a low number of cases classified as II and III. Mean femoral version was 21.73°, 26.8° and 43.58°, respectively. ICC between observers A and B for CCD measured in X-rays was 0.96. Mean CCD measured in X-rays for each group (I, II/III and IV) was 148.11°, 147.7° and 147°, and in CT was 131.21°, 127.9° and 122.14°, respectively. A significant difference was found in femoral version between groups I and IV (P=0.0002) and II/III and IV (P=0.042). Pearson correlation between femoral version and severity of DDH was positive (r=0.52; P=0.0002). A significant difference between CCD measured in CT was found between groups I and IV (P=0.003).
ConclusionsA significant increase in femoral version related to severity of DDH and a positive correlation between these 2 features were found. Furthermore, a significant decrease in CCD between groups I and IV measured in CT was revealed. These findings would be helpful for preoperative planning of total hip replacement in osteoarthritis secondary to DDH, because once the surgeon has assessed the severity of DDH on X-rays or CT, an increased femoral version could be expected. Therefore, availability of specific implants such as conic, modular or cemented stems is critical, in order to modify the femoral anteversion to normal values in the most severe cases.
La displasia del desarrollo de cadera (DDC) es una dolencia que incluye un gran espectro de manifestaciones articulares, tales como alteraciones en la versión femoral y en el ángulo cérvico-diafisiario (ACD), así como una probable progresión a artrosis. El objetivo de este estudio fue buscar una correlación entre la versión femoral y la gravedad de la DDC en pacientes con artrosis. Otro objetivo planteado fue evaluar si se presentan cambios significativos en el valor del ACD a medida que la gravedad de la DDC aumenta.
Materiales y métodoEntre marzo de 2018 y febrero de 2019 fueron evaluados pacientes mayores de 15años con DDC, sin cirugías de cadera previas y artrosis grave de cadera en espera de artroplastia total. Se solicitaron radiografías (Rx) de pelvis (anteroposterior) y de cadera (anteroposterior y lateral), así como tomografías axiales computarizadas (TC) de cadera y rodilla de las extremidades afectadas, en las cuales se realizó la medición de la versión femoral y del ACD.
La clasificación de Crowe fue utilizada para categorizar la gravedad de la DDC y, al igual que el ACD, fue evaluada en forma independiente por dos observadores. La versión femoral y el ACD en la TAC fueron medidos por un radiólogo especialista en enfermedad musculoesquelética. El análisis estadístico fue realizado con SPSS v. 21. Se consideró un valor significativo de p<0,05.
ResultadosLos 42 pacientes que cumplieron los criterios de inclusión asistieron a la evaluación; el 76% era de género femenino, con una edad promedio de 52,7años. De un total de 54 caderas afectadas, 45 fueron evaluadas con ambos exámenes (Rx y TAC) y 9caderas solo con Rx (uno de ellos falleció por otras causas antes de la TAC). El 48%, el 16%, el 7% y el 28% de las caderas fueron clasificadas en la Rx como Crowe I, II, III y IV, respectivamente, con una concordancia interobservador del 100%. Los tipos de DDC según Crowe fueron agrupados como I, II/III y IV para su análisis, debido al bajo número de casos clasificados como II y III. Respecto a la versión femoral, el promedio de cada grupo fue 21,73°, 26,8° y 43,58°, respectivamente. El ACD en Rx fue medido por dos observadores independientes con una correlación interobservador del 0,96. El ACD promedio en Rx para cada grupo (I, II/III y IV) fue de 148,11°, 147,7° y 147° y en TAC de 131,21°, 127,9° y 122,14°, respectivamente. Dentro de los resultados más relevantes, destacan los siguientes: a)una diferencia significativa en cuanto a versión femoral entre los grupos I y IV (p=0,0002) y entre los grupos II/III y IV (p=0,042); b)la correlación de Pearson entre versión femoral y los 3grupos fue positiva (r=0,52; p=0,0002), y c)una diferencia significativa del ACD medido en TAC entre los gruposI y IV (p=0,003).
ConclusionesEste estudio demostró importantes hallazgos, como el aumento significativo de la versión femoral en relación con la gravedad de la DDC y la correlación positiva entre ambos factores. Por otra parte, se encontró una disminución significativa del ACD entre los gruposI y IV al comparar las mediciones de la TAC. Estos resultados son relevantes y pueden ser considerados durante la planificación quirúrgica con el fin de contar con los implantes necesarios para corregir las alteraciones de la cadera displásica artrósica.
Developmental dysplasia of the hip (DDH) is a spectrum of joint manifestations ranging from isolated acetabular dysplasia to subluxation or complete dislocation of the hip. If left untreated, dysplastic hips are prone to lead to muscle impairment, gait claudication and osteoarthritis.1 DDH prevalence ranges between 1.56 and 2.8 cases per 1000 live births, depending on its definition and the population studied.2,3 The reported rate of DDH among different countries varies between .04% and 16%, as published by Loder and Skopelja.4 This incidence apparently varies according to child-rearing practices of each geographical area. In colder regions, such as the north of Canada, the reported incidence is 19.8%; in Hungary it is 2.8%; In Australia, .78%; in Spain .2%; in Israel, .3%; in Taiwan, .29% and in South Africa .003%.4 In Chile, DDH affects a range between .1% and 3% of the population and its incidence is estimated as one in every 500–600 live births,5 i.e. between 400 and 460 cases per year.6
It has been reported that up to 94% of adults with untreated DDH will present with moderate or severe hip osteoarthritis in the second decade of life.7 According to the Norwegian arthroplasty register, DDH was associated with 7% of all primary hip replacements, and at least with a third of the hip arthroplasties in those under 65 years of age.8
Although most studies have focused on acetabular morphology, 9–15 several publications have described the femoral characteristics in this pathology.12,14,16 Which the following stand out: short neck, narrow medullary canal, increased anteversion and anespherical head.9–15 Femoral version is another aspect that has been mentioned in previous publications and is defined as the angle between the line tangent to the posterior border of the femoral condyles and the line passing through the centre of the femoral head and femoral neck.17 However, these studies do not mention whether a correlation exists between the severity of the DDH and the femoral version, which is a major aspect to consider when planning a total hip arthroplasty (THA). Besides, understanding this association is essential for hip surgeons in order to consider specific implants should a major femoral anteversion require correcting as the degree of DDH severity increases.
The main aim of this study was to search for correlation between the femoral version and the DDH severity. The secondary aim was to assess whether significant changes presented in the caput-collum-diaphyseal angle (CCD) as DDH severity increased.
MethodFrom March 2018 to February 2019 patients with coxofemoral osteoarthritis on the waiting list for THA were assessed, on prior approval for this research by the hospital Ethics Committee. To meet the inclusion criteria patients had to be over 15 years of age, with no previous surgery, with osteoarthritis secondary to DDH, which was defined as coxofemoral joints with a centre-edge angle<20°.18 The age criterion is explained because our institution is a hospital for adults, according to the national health definition, and therefore all people attending it are over 15 years of age.
The selected patients were contacted by phone, the absence of prior hip surgery was confirmed, and they were given appointments for medical assessment. They all agreed to participate in the study and received written instructions to take radiographs (XR) and computed axial tomographies (CT) of the affected hip. In addition, the absence of previous scars was confirmed during the physical examination.
The radiographs (XR) requested from each patient were the following views19: (a) anteroposterior (AP) of the pelvis, supine, with the hips in 15° internal rotation, with a distance of 120cm between the beam-emitting tube and the receiving plate, with the beam perpendicular to the table, centred in the space between the upper edge of the symphysis pubis and the line between the 2 anterosuperior iliac spines; (b) AP hip view with similar technique to the AP pelvis projection, with the beam directed perpendicular to the femoral neck (approximately 6.4cm below the anterosuperior iliac spine) and c) lateral hip view, with the patient in the supine position, the extremity to be assessed extended with 15° internal rotation and the contralateral extremity with the hip and knee in flexion above 80°, so that the beam is positioned parallel to the table and aimed at a 45° angle with the affected extremity extended, focused on the femoral head. These images were assessed separately by 2 orthopaedic surgeons and trauma surgeons (C.C and N.R.: observers A and B, respectively). The intraclass correlation coefficient (ICC) was applied to assess the level of concordance between both observers, in keeping with Landis and Koch criteria.20
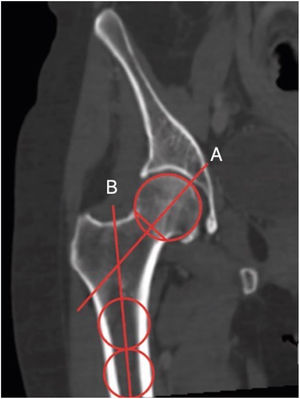
The affected hip was classified according to with the Crowe11 classification in the AP pelvis view. In the AP hip view the CCD21 was measured, which is defined as the angle between the axes of the femoral neck and the diaphysis.21 The CCD measurement technique used in the AP radiographs (XR) of the hip was similar to that described for the CT: first the circumference of the femoral head and its centre were traced; then the femoral neck axis was determined as a line passing through the centre of the cephalic and caudal neck edges and which passes through the centre of the femoral head. The femoral axis was then determined as the line passing through the centre of 2 contiguous circles contacting the medial and lateral outer cortices of the femoral diaphysis. The angle formed between those two axes corresponds to the CCD.
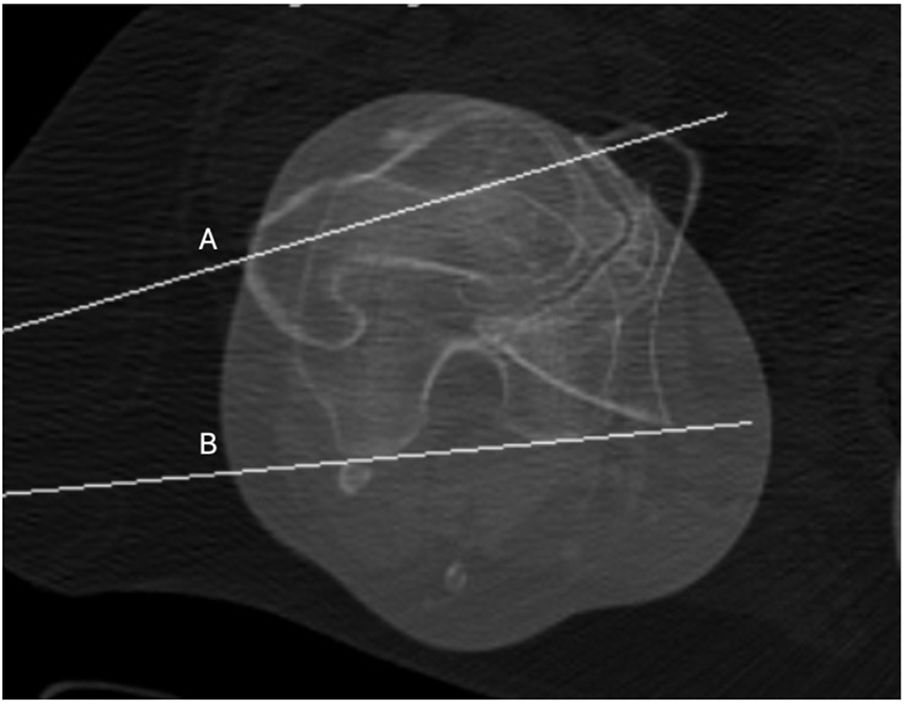
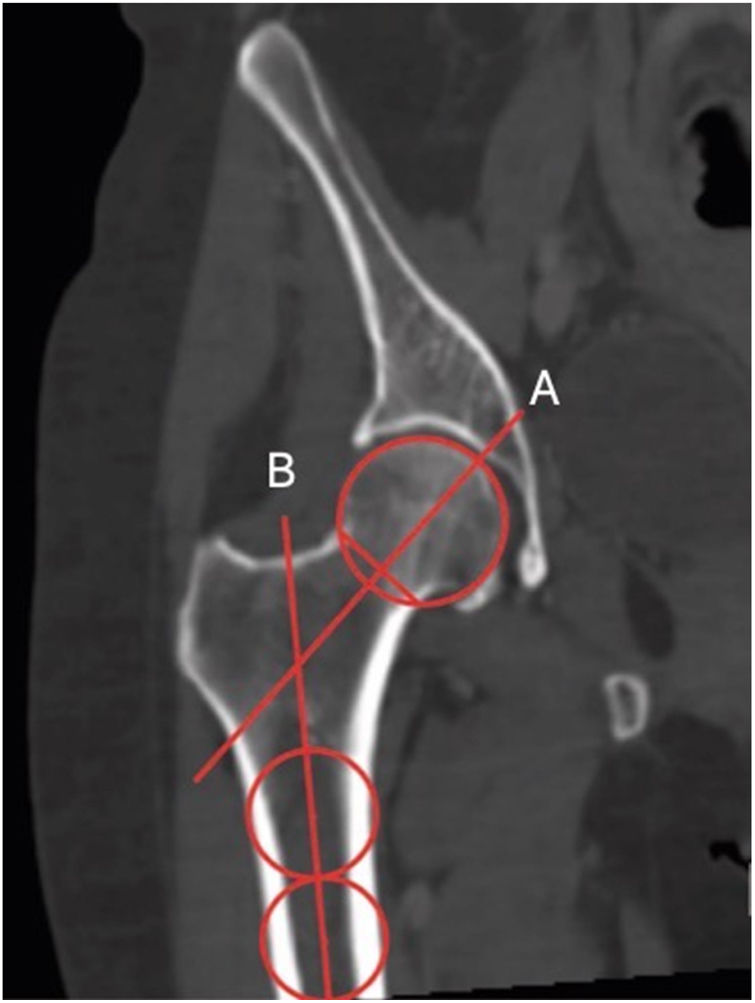
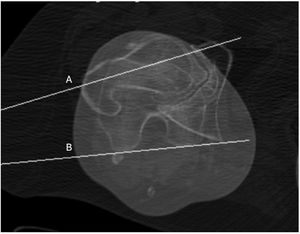
CT was also performed of the proximal and distal femur of the affected side to measure the femoral version22,23 (Fig. 1) and the CCD24 (Fig. 2), which was performed by a radiologist, trained in musculoskeletal diseases, applying the previously described technique relating to the measurement of the CCD in XR.
Measurement of the femoral version in CT according to the method described by Murphy et al.22,23 The angle formed between A (axis of the femoral neck) and B (posterior axis of the femoral condyles) represents the femoral version.
Measurement of the CCD, as described by Boese et al.24 The angle formed between A (head-neck axis) and B (femoral shaft axis) represents CCD.
Statistical analysis was performed with the SPSS v. 21. software. The Shapiro–Wilk normality test was used to confirm normal distribution of the data and the Student's t-test for non-paired samples to analyse the statistical significance, defined as p<.05. The Pearson (r) test was assessed if correlation existed between the femoral version of each group (I, II/III and IV) (positive if >.5).
ResultsA total of 42 patients (54 hips) met the inclusion criteria and they all attended assessment. Of these patients, 32 (76%) were female and their mean age was 52.7 years (standard deviation [SD] 9.5; range 24–66). The imaging study request was complete (RX and CT) in 45 hips; CT was not performed in 9 hips due to non-attendance of the patients (in one of them only the RX was taken, due to death). This provided a total of 54 hips assessed in at least one of the 2 tests.
According to the classification by Crowe, 26 (48%), 9 (16%), 4 (7%) and 15 hips (28%) were classified as Crowe I, II, III and IV, respectively, with RX. The concordance between both observers in this parameter was 100%. Due to the low number of Crowe II and III hips in this series, the authors decided to join these cases together into a new group called ii/iii for statistical analysis, following the example of other publications.12,14
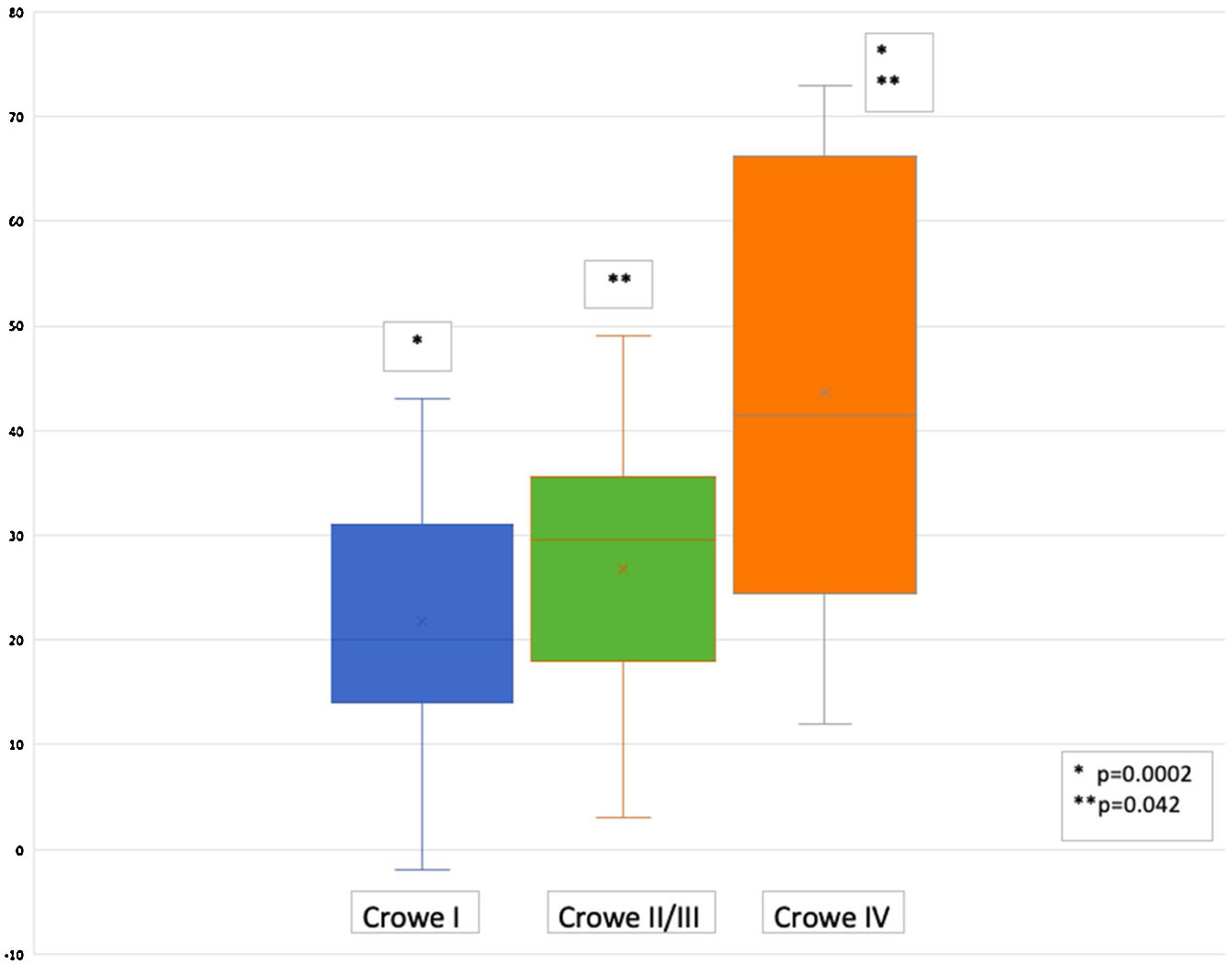
Femoral versionThe mean femoral version for each Crowe class is contained in Table 1 and in Fig. 3. It is of note that in 8 hips the femoral version was not possible to be measured due to a major osteoarthritic deformity and neither could a patient be assessed who, although the RX was performed, died of other causes prior to the CT.
The main femoral version for groups I, II/III and IV was 21.74 (95% confidence interval [CI] −2 to 43); 26.8 (95% CI 3–49) and 43.58 (95% CI 12–73), respectively, with a statistically significant difference between groups I and IV (p=.0002) and between groups II/III and IV (p=.042).
The correlation of the femoral version with severity of DDH according to Crowe (comparison between groups I vs. II/III, II/III vs. IV and I vs. IV) was positive (r=.52; 95%CI .27–.7; p=.0002).
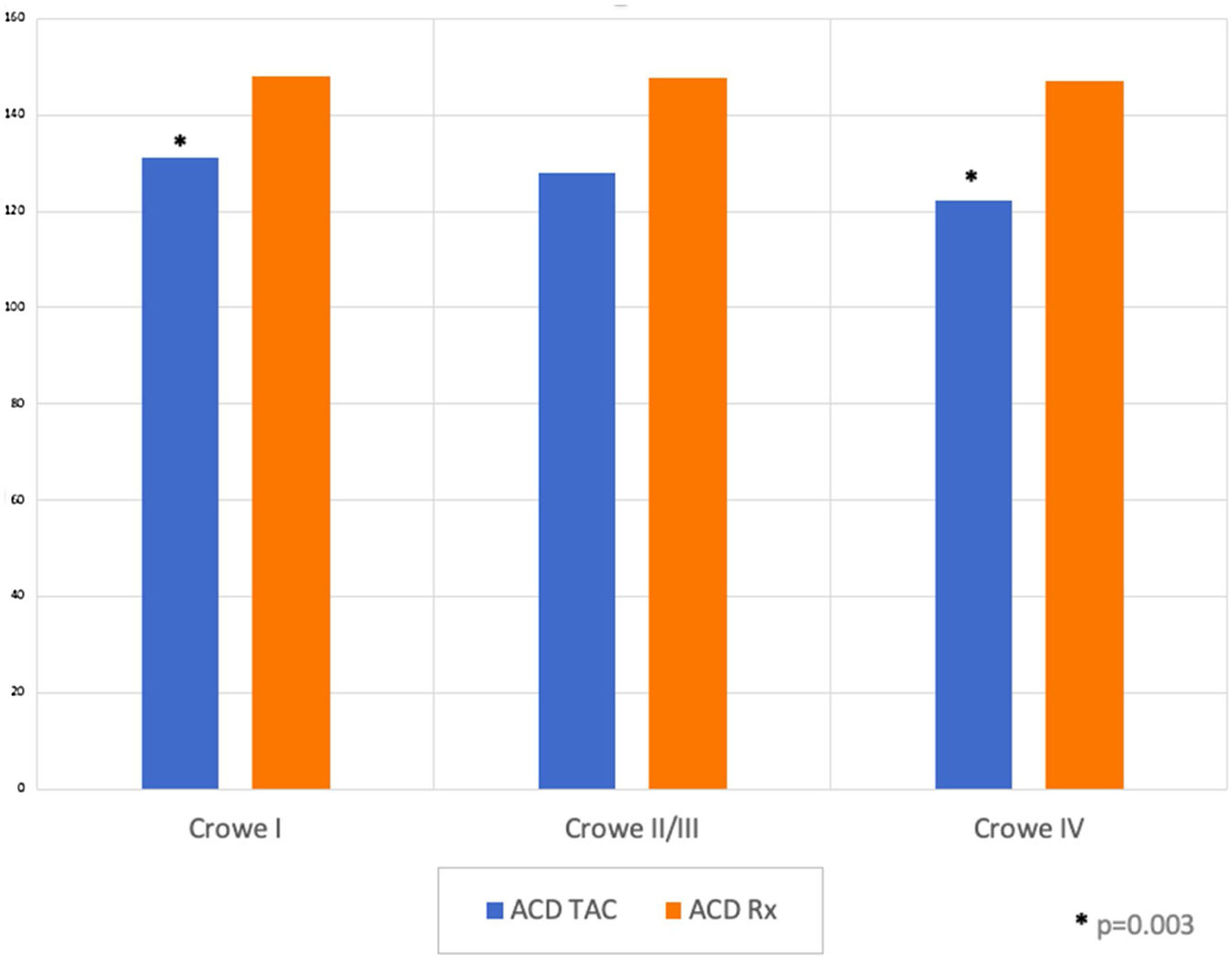
Caput-collum-diaphyseal angleThe main CCD measured on RX by observer A was 147.54 (SD 9.03; range 123–167). The average CCD measured by observer B was 147.9 (SD 8.63; range 129–174). The ICC between both observers for CCD measured on RX was 0.96. The main CCD of both observers was used for subsequent analyses (Table 2).
Main CCD average in RX according to observers A and B, and CCD average in CT.
| Main CCD average observers A and B in RX (SD; range) | Main CCD average in CT (SD; range) | |
|---|---|---|
| Crowe I | 148.11° (7.68; 132–166) | *131.21° (6.77; 117–142) |
| Crowe II/III | 147.7° (6.83; 136.5–156) | 127.9° (9.04; 116–145) |
| Crowe IV | 147° (11.55; 126–169) | *122.14° (5.58; 114–130) |
CT: computerised axial tomography; CCD: caput-collum-diaphyseal angle; RX: radiography; SD: standard deviation.
On the other hand, the mean CCD measured on CT by a single observer (radiologist) was 128.84 (SD 7.74; range 114–145). The Student's t-test between RX-measured CCD (when comparing all groups to each other), as well as when comparing RX vs. CT measurements, did not show a significant p-value. However, when comparing CCD measured on CCD between groups I and IV, the p-value was .003, which showed that there was a significant difference between the two measurements (Fig. 4). It should be noted that in 3 RX cases and in 7 CT cases, measurement of CCD was not possible due to the severe deformity of the proximal femur caused by osteoarthritis.
DiscussionThis study demonstrated a positive correlation between femoral anteversion and severity of DDH according to Crowe, and also found a significant difference between the CT-measured CCD between Crowe classes I and IV, implying that, as the severity of the dysplasia increases, the CCD would tend to decrease. Furthermore, the difficulty in CCD measurement in dysplastic osteoarthritic hips is considerable and differences were observed in the evaluation of that angle between RX and CT.
There are several interesting publications on this subject. Sugano et al.14 studied 35 dysplastic femora of 31 adult women with CT and compared them with a control group paired in age and sex. They observed a significant difference in the femoral version between the Crowe IV dysplastic hips (37.0°±5.4°) and the control group (22.6°±10.6°; p=.0005), but they did not find any differences between the other Crowe classes and controls, despite the fact the femoral version showed a trend to increase the higher the DDH severity. Furthermore, they noted that the femoral anteversion of the Crowe I hips was 12° higher than in the control group and that in the Crowe II/III and IV hips this anteversion was 10–14° greater than normal. With regard to the CCD, the most severe cases of DDH presented angles lower than the milder ones, similarly to findings of our study. However, no statistically significant differences were found.
Noble et al.12 developed a CT study of 154 dysplastic hips and compared them with a control group adjusted by age and gender. In their results, they reported that the Crowe I hips had a greater increase in femoral anteversion (45.4°±13.6°) compared with normal controls (35.6°±13.7°; p=.0005). Nevertheless, this finding was not significant when compared with the other Crowe classes and the control group. Besides, these authors showed that the most severe cases of dysplasia presented with a greater femoral version than the mildest ones (Crowe IV: 47.0°±8.3°), but with no statistical significance, similarly to the results found by Sugano et al.14 The femoral anteversion found by these authors in the most advanced cases of dysplasia is comparable with the data obtained in our study.
Wells et al.16 evaluated with CT 50 non-arthritic dysplastic hips that were undergoing preoperative planning for periacetabular osteotomy. They calculated a mean femoral version of 19±12 and a mean CCD of 136±5, comparable with our results in Crowe I hips.
Furthermore, Argenson et al.9 evaluated with RX and CT 247 osteoarthritic dysplastic hips which were on the waiting list for arthroplasty in 218 adults and they were classified according to Crowe. One interesting point in this study is that dysplastic hips which were not subluxated were considered as a separate group and that there was a control group of primary osteoarthritic hips. In their results they found great variability in the femoral version of the dysplastic groups, which was higher in the Crowe IIs when compared to all groups. In terms of CCD, they reported an incidence of coxa valga of 46.5% and 27.4% in the subluxation and non-subluxed dysplasia groups, respectively. Reviewing the data table presented by them, a trend towards coxa vara with increasing severity of dysplasia stands out, which is comparable with our results.
This study started with the hypothesis that as the severity of DDH increased, femoral anteversion incremented as well. For the purposes of analysis, the Crowe II and III classes were considered as a single group, due to the low number of hips classified as such in our series. The results show a statistically significant difference between groups I and IV, and also between groups II/II and IV, regarding the Crowe classification and femoral version, which supports the initial hypothesis. A positive correlation was also found between these 2 variables.
The authors’ theory on this research regarding these findings is explained as follows: it has been demonstrated that femoral anteversion decreases as age in childhood increases,25,26 thus it is probable that the femur in severe DDH cases supports loads in different directions compared to the normal femora during walking, due to subluxation or frank dislocation and are therefore prone to maintain the increased anteversion.
Regarding CCD, a statistically significant difference between groups I and IV was shown only for measurements performed in CT, which indicates a trend towards reduction for the CCD in the most severe groups of dysplasia according to the Crowe classification, in a similar manner to previously published data.12,14
The reduction of the CCD could be explained, according to a hypothesis of the authors of this study, by the traction that the ligamentum teres and joint capsule would exert on the unstable femoral head, which tends to ascend in the developing dysplastic hip. Along these lines, it could be suggested that these static hip stabilisers have a role in remodelling the CCD towards varus as the femoral head dislocates or subluxates during intrauterine development and childhood. However, it is clear that further research is required to determine whether this hypothesis is valid.
The major strength of this study is that the selected patients did not have any previous surgeries on the assessed hips and therefore these hips did not possess surgical modifications in the acetabular and femoral versions which could alter the position of the femur. Another positive aspect is that the patient assessment and data collection was performed prospectively.
Notwithstanding, this research exhibits some obvious limitations. Firstly, it is neither a randomised nor blind study and there is no control group. In addition, all the patients presented with advanced osteoarthritis, which hindered a precise measurement of the angles in the images. Another major factor to consider is the presence of osteoarthritis attributable to patient age and activity which was not specifically analysed. The CT angles were assessed by a single observer (radiologist), whereas measurements performed by at least 2 observers would be preferable. Another element to analyse is that the severe deformity produced by osteoarthritis hindered some measurements, mainly in the RX, given that the CT permitted to select the best slice to perform the necessary evaluations. Another relevant aspect is that the groups according to the Crowe classification did not have the same number of patients in this study, because the majority of the cases in our series were classified as Crowe I. Lastly, a highly interesting variable which could have been assessed if the degenerative arthropathy cases reported in our series had not been such advanced is the acetabular morphology and in what manner its version or inclination was related to the femoral morphology.
The authors of this study consider that the findings are valuable for preoperative planning of THA secondary to DDH, since with this information the surgeon can expect to find an increased femoral anteversion in the most severe cases and have specific implants available to modify this excessive anteversion, such as conical, modular or cemented stems and to avoid the inadequate positioning of the components due to the modification in the usual anatomical references caused both by the dysplasia and the joint deformity of the advanced osteoarthritis.
ConclusionAmong the findings of this study are included the significant increase of the femoral version the higher the DDH class according to Crowe's classification, and a positive correlation between both variables. In addition, the results revealed a significant reduction of the CCD measured in CT between the Crowe I and IV dysplasia groups. These results are relevant and should be considered during the surgical planning, in order to have the necessary implants to correct the modifications of the osteoarthritic dysplastic hip, and prevent an inadequate position of the components due to modification of the normal anatomy.
FinancingThis research did not receive any specific funding from the public sector, commercial sector or not-for-profit entities.
Level of evidenceLevel of evidence iv.
Conflict of interestsNone.