Compare the morbidity and mortality, the length of hospital stay and the economic cost of the fragility fracture of the hip, in two nonconsecutive years thanks to the integrated orthogeriatric care.
Material and methodRetrospective observational cohort study with 633 patients with hip fragility fracture with a mean age of 85.5 years, treated in the same Trauma and Orthopaedic Surgery service in two different years (2012 and 2017). Mean stay, surgical delay, perioperative mortality, one month and one year, and perioperative complications such as acute urine retention, pressure ulcers, and need for transfusion were measured.
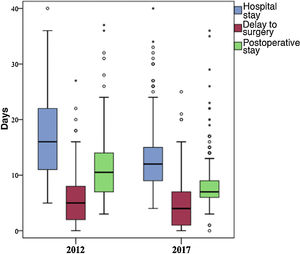
ResultsMortality during admission decreased from 10% in 2012 to 3.6% in 2017 (p = .004*), while mortality at thirty days (10.5% vs 7%) (p = .123) and one year (28.9% versus 24.9%) (p = .277). Hospital stay times, surgical delay, and postoperative admission time also decreased. The estimated total annual economic savings thanks to integrated orthogeriatric care amounted to € 1,017,084.94.
ConclusionsIntegrated orthogeriatric care of the patient with fragility fracture of the hip, results in a more effective and efficient care model. Both the care and the clinical situation of patients are improved in the perioperative period, both hospital stay and mortality during admission are significantly reduced, and all this with significant associated economic savings.
Comparar la morbimortalidad, el tiempo de estancia hospitalaria y el gasto económico de la fractura por fragilidad de cadera en 2 años no consecutivos gracias a la atención ortogeriátrica integrada.
Material y métodoEstudio observacional retrospectivo de cohorte con 633 pacientes con fractura por fragilidad de cadera con una media de edad de 85,5 años, tratados en un mismo servicio de Cirugía Ortopédica y Traumatología en dos años diferentes (2012 y 2017). Se midieron la estancia media, la demora quirúrgica, la mortalidad perioperatoria, al mes y al año, y complicaciones perioperatorias como la retención aguda de orina, las úlceras por presión y la necesidad de transfusión.
ResultadosLa mortalidad durante el ingreso disminuyó del 10% en 2012 al 3,6% en 2017 (p = 0,004), a la vez que la mortalidad a los 30 días (10,5% frente a 7%) (p = 0,123) y al año (28,9% frente a 24,9%) (p = 0,277). También disminuyeron los tiempos de estancia hospitalaria, la demora quirúrgica y el tiempo de ingreso postoperatorio. El ahorro económico total anual estimado gracias a la atención ortogeriátrica integrada supuso 1.017.084,94€.
ConclusionesLa atención ortogeriátrica integrada del paciente con fractura por fragilidad de la cadera, resulta en un modelo de atención más efectivo y eficiente. Se mejoran tanto la calidad asistencial como la situación clínica de los pacientes en el periodo perioperatorio, se disminuyen significativamente tanto la estancia hospitalaria como la mortalidad durante el ingreso, y todo ello con un importante ahorro económico asociado.
Fragility fractures of the hip (FFH) occur due to accidental falls from standing height in patients over 60 years of age. They are a major and common health problem, especially in aged societies like that of our autonomous community of Galicia. Here, according to the Galician Institute of Statistics there is an ageing index of 158.15 in 2019 (for each 100 people under the age of 20 years over 158 people are over the age of 64).1 The consequences in the short and long term are particularly relevant, since quality of life falls, morbimortality increases, and subsequently physical dependence in the great majority of cases.
This type of fracture accounts for under 20% of all osteoporotic fractures2 but due to the progressive rise in the ageing population, it has been estimated that the total number of hip fractures in the world will surpass 3 million in 2040.3
In most cases the main treatment is surgery, but even after it the rate of postoperative complications is high and the recovery period complicated. It has been described in the literature that after early surgery, during the first 24–48 h, the number of complications falls considerably but even so, the rate of mortality in patients with FFH is up to 10% after one month and up to 30% one year after suffering from the fracture.3–6
Integrated orthogeriatric care was developed in England at the end of the 1950’s. In the literature it is described as having major advantages, such as the reduction of mortality rates, hospital stay and hospital costs.7–10 As a result improvements in clinical and functional outcomes occur, since there is early movement and faster functional recovery in these patients. Spain has a broad experience of this, reflected in several publications from recent decades.3,9,10
The main aim of this study was to assess morbimortality and length of hospital stay in patients with FFH in our area, on 2 non-consecutive years, and to carry out a comparative study of the evolution of hip fractures with involvement of a geriatric specialist. A secondary aim was to analyse the financial impact of orthogeriatric care in the total hospital costs afforded by the FFH.
Material and methodA retrospective observational study was made where all patients over 75 years of age who had suffered from a FFH and had been cared for in our centre on 2 non-consecutive years were reviewed. The years 2012 and 2017were chosen as comparison groups. In the year 2012 our health area comprised 2 different hospitals which were benchmarks for different populations. Patient follow-up for FFH by a different specialist was only made through inter-consultation to medical services when the Orthopaedic Surgery and Traumatology Service (OSTS) considered it necessary. In 2017 the two hospitals were amalgamated to form a large tertiary level hospital covering the whole health area population (approximately 480,000 inhabitants), of both urban and rural areas. The orthopaedic surgeons, anaesthetists and nursing staff of both hospitals were incorporated together into the new centre. We began to work with integrated orthogeriatric care for the follow-up and treatment of patients with FFH. Our hospital also started to participate in the Spanish National Hip Fracture Registry (SNHFR). This project promotes the unification of FFH patient data in Spain and compares quality in order to optimize care, reduce morbimortality and lower costs.10 Based on this, we wished to compare the data collection of our area with the known national levels and to review several different variables which were of interest to us, such as the need for transfusion or acute urine retention.
Fractures from high energy accidents, or pathological or atypical fractures were excluded, as were patents transferred to other healthcare centres, and those lost to follow-up.
The main variables of measurement were mortality and length of hospital stay. Mortality was collected in 3 periods: death in hospital; death after one month and death after one year. Regarding hospital stay this variable was divided into: mean hospital stay calculated as the difference between the discharge date and the admission date; surgical delay, calculated as the difference between the date of surgery and the admission date and postoperative stay, calculated as the difference between discharge date and surgery.
Furthermore, for analysis of the comparability between groups age; sex; type of fracture; side; type of surgery carried out; pre and post fracture mobility; prior comorbidities of the patient according to the American Society of Anaesthesiologists (ASA)11 scale; place of residence before the fracture and on hospital discharge and the degree of cognitive impairment according to the Pfeiffer12 scale were assessed.
Hospital morbidity variables were measured as the incidence during hospital admission of acute urine retention (AUR) and pressure ulcers (PU) equal to or above 213,14 and the need for blood product transfusion.15
Management and cost/benefit analysis involved the cost of hospital resources and the gross salary of the professionals according to the scale published in the Official Bulletin of the autonomous community where the study was conducted.16 Surgical, implant, medicine and diagnostic test costs were assumed to be similar in both periods and the difference in the total cost was estimated indirectly through the hospital stays saved. This method had already been used previously in other studies.9
All data were obtained from the patients’ electronic medical records. Given that the whole population is covered by the National Healthcare System, the care traceability received at all healthcare levels is ensured, both in primary and in specialist hospital care. Similarly, deaths are recorded in the system the same date they are certified. The data register comes from the SNHFR17 database, to which our hospital centre subscribes and the protocol was approved by our hospital’s research ethics committee. The researchers carried out the study in keeping with the principles of the Declaration of Helsinki. The study was developed in accordance with the protocol and met with good clinical practice, as described in the regulations of the International Conference on Harmonization for good clinical practice.
Statistical analysisDescriptive statistical analysis was performed of the categorical variables using frequencies and percentages. For the continuous variables central tendency measurements were used, such as mean and standard deviation, mean standard error and confidence interval. To compare the variables between both groups the Chi-square test and Mann–Whitney U test were used. A p < .05 value was considered to be statistically significant. Analyses were performed with SPSS v24.0 (IBM®).
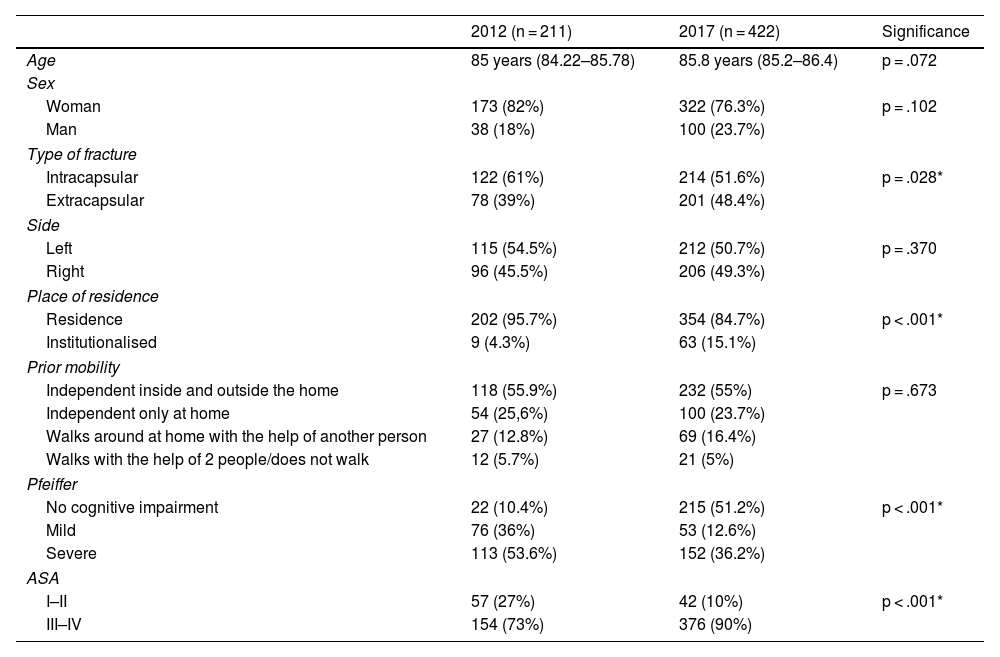
ResultsA total of 633 patients who suffered from an FFH were studied, aged between 75 and 101 years (mean 85.5 ± 6 years). The sociodemographic characteristics of the 2 groups of patients are detailed in Table 1. The typical patient was a women aged 85 with an intracapsular fracture of the left hip due to non-pathological fragility, who lived at home, was independently mobile both inside and outside the hose, who presented with severe cognitive impairment and suffered from at least one systemic disease which limited her activity and could have left her disabled (ASA III–IV).
Sociodemographic characteristics and differences between groups.
| 2012 (n = 211) | 2017 (n = 422) | Significance | |
|---|---|---|---|
| Age | 85 years (84.22–85.78) | 85.8 years (85.2–86.4) | p = .072 |
| Sex | |||
| Woman | 173 (82%) | 322 (76.3%) | p = .102 |
| Man | 38 (18%) | 100 (23.7%) | |
| Type of fracture | |||
| Intracapsular | 122 (61%) | 214 (51.6%) | p = .028* |
| Extracapsular | 78 (39%) | 201 (48.4%) | |
| Side | |||
| Left | 115 (54.5%) | 212 (50.7%) | p = .370 |
| Right | 96 (45.5%) | 206 (49.3%) | |
| Place of residence | |||
| Residence | 202 (95.7%) | 354 (84.7%) | p < .001* |
| Institutionalised | 9 (4.3%) | 63 (15.1%) | |
| Prior mobility | |||
| Independent inside and outside the home | 118 (55.9%) | 232 (55%) | p = .673 |
| Independent only at home | 54 (25,6%) | 100 (23.7%) | |
| Walks around at home with the help of another person | 27 (12.8%) | 69 (16.4%) | |
| Walks with the help of 2 people/does not walk | 12 (5.7%) | 21 (5%) | |
| Pfeiffer | |||
| No cognitive impairment | 22 (10.4%) | 215 (51.2%) | p < .001* |
| Mild | 76 (36%) | 53 (12.6%) | |
| Severe | 113 (53.6%) | 152 (36.2%) | |
| ASA | |||
| I–II | 57 (27%) | 42 (10%) | p < .001* |
| III–IV | 154 (73%) | 376 (90%) | |
Mean ± standard deviation, frequency (percentage).
p Value corresponding to Mann–Whitney U test and Chi-squared test.
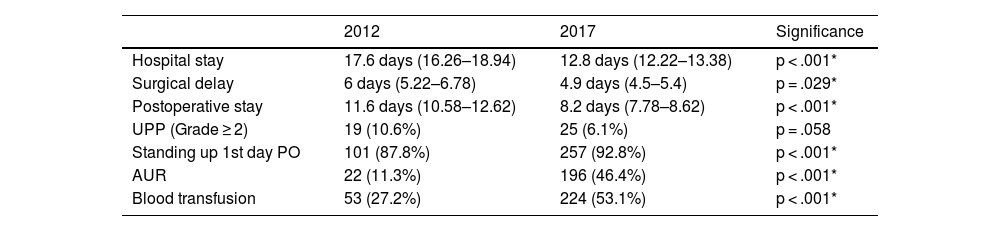
In 2012 hospital management of patients with FFH was associated with intervention from a clinical specialist in 29% of cases (internal medical professional in 17% and geriatric in 12% of cases.). In 2017, in addition to follow-up by an orthopaedic surgeon, these patients received orthogeriatric co-management in 98% of cases (p < .001). The differences in hospital stays and complications during the admission between both years are detailed in Table 2.
Difference in hospital stay and complications during hospitalisation between groups.
| 2012 | 2017 | Significance | |
|---|---|---|---|
| Hospital stay | 17.6 days (16.26–18.94) | 12.8 days (12.22–13.38) | p < .001* |
| Surgical delay | 6 days (5.22–6.78) | 4.9 days (4.5–5.4) | p = .029* |
| Postoperative stay | 11.6 days (10.58–12.62) | 8.2 days (7.78–8.62) | p < .001* |
| UPP (Grade ≥ 2) | 19 (10.6%) | 25 (6.1%) | p = .058 |
| Standing up 1st day PO | 101 (87.8%) | 257 (92.8%) | p < .001* |
| AUR | 22 (11.3%) | 196 (46.4%) | p < .001* |
| Blood transfusion | 53 (27.2%) | 224 (53.1%) | p < .001* |
AUR: acute urine retention; PO: postoperative; PU: pressure ulcers.
Values expressed as mean + standard deviation and frequency (percentage).
p Value corresponds to Mann–Whitney U tests and Chi-squared test.
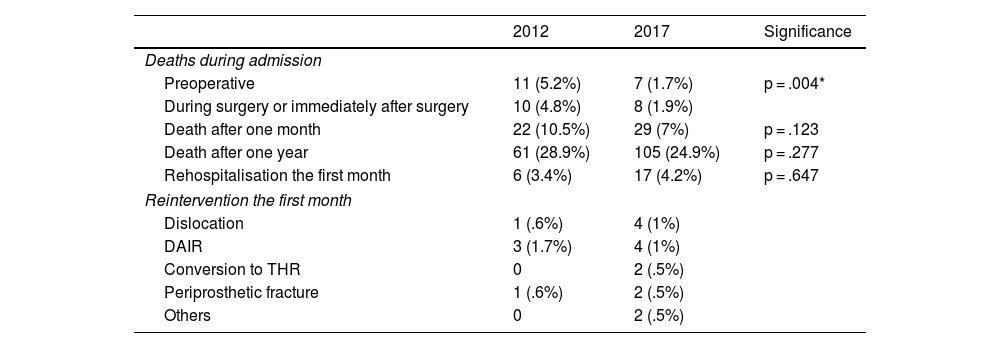
The number of deaths during stay, one month and one year after the fracture are included in Table 3. Statistically significant differences were found in mortality during stay, which was 10% in 2012and dropped to 3.6% in 2017 (p = .004). A reduction in mortality was also observed after 30 days (10.5% compared with 7%) (p = .123) and after one year (28.9% compared with 24.9%) (p = .277) between both groups, although these differences were not statistically significant.
Mortality and morbidity rates in both groups.
| 2012 | 2017 | Significance | |
|---|---|---|---|
| Deaths during admission | |||
| Preoperative | 11 (5.2%) | 7 (1.7%) | p = .004* |
| During surgery or immediately after surgery | 10 (4.8%) | 8 (1.9%) | |
| Death after one month | 22 (10.5%) | 29 (7%) | p = .123 |
| Death after one year | 61 (28.9%) | 105 (24.9%) | p = .277 |
| Rehospitalisation the first month | 6 (3.4%) | 17 (4.2%) | p = .647 |
| Reintervention the first month | |||
| Dislocation | 1 (.6%) | 4 (1%) | |
| DAIR | 3 (1.7%) | 4 (1%) | |
| Conversion to THR | 0 | 2 (.5%) | |
| Periprosthetic fracture | 1 (.6%) | 2 (.5%) | |
| Others | 0 | 2 (.5%) | |
DAIR: surgical drainage, antibiotic therapy and implant retention; THR: total hip replacement.
p Value corresponding to Chi-squared test.
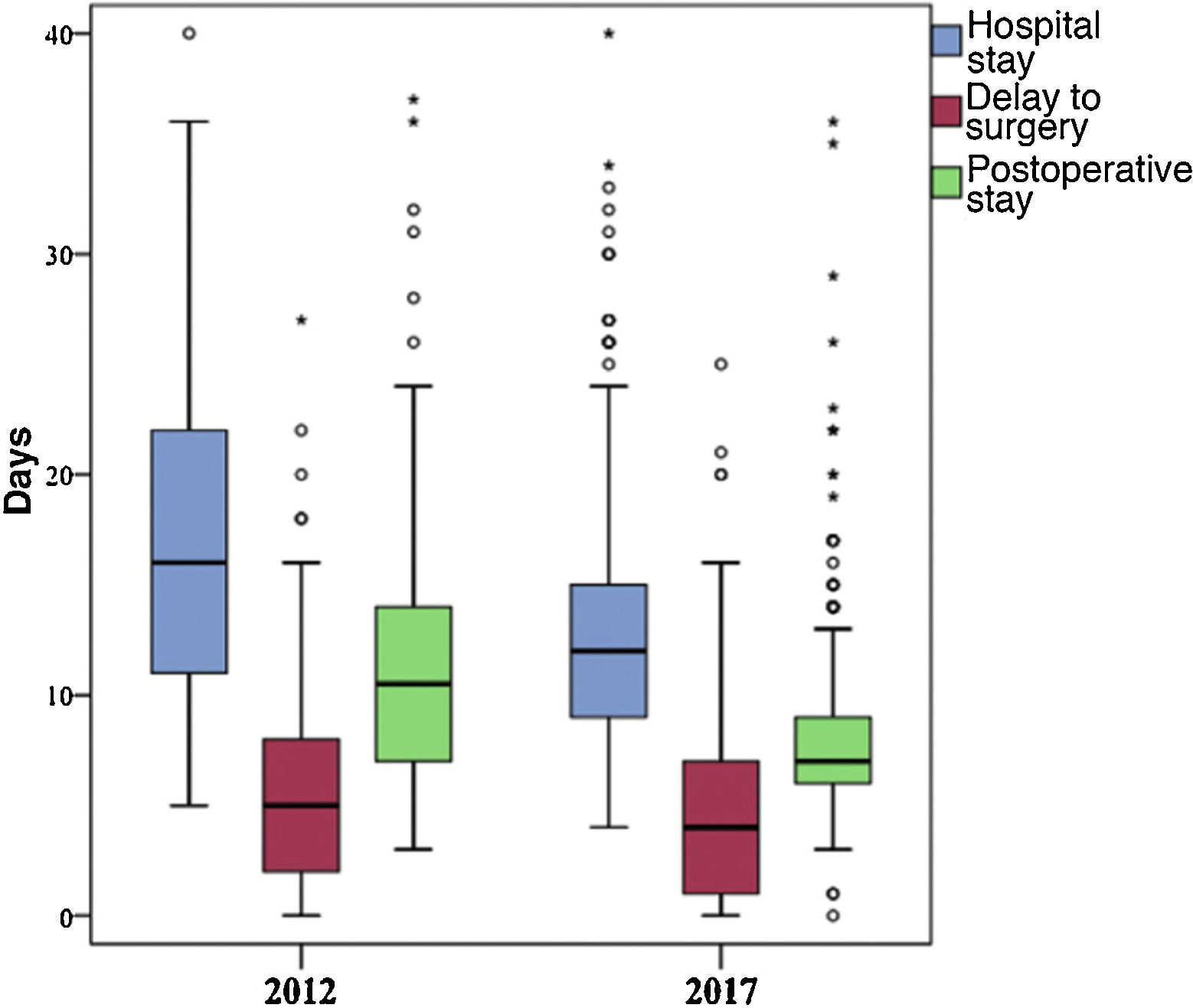
All hospital stay times dropped significantly in 2017 compared with 2012. Mean stay specifically dropped by 4.8 days (p < .001), surgical delay dropped by 1.1 days (p = .029) and the postoperative hospital stay duration, from surgery until discharge, dropped by 3.4 days (p < .001). These variations are shown in Fig. 1. The proportion of patients who received a blood product transfusion during their stay and who were diagnosed with acute urine retention also statistically significantly increased (p < .001). The percentage of patients who developed grade 2 pressure ulcers during their stay also dropped, although this difference was not statistically significant. (p = .058).
Regarding cost-benefit analysis, the essential difference in intrahospital follow-up of patients with FFH in the year 2017 compared with 2012,was that follow-up of practically all of them was carried out by a geriatric specialist. Assuming a similar sum of hospitalization, medication and surgical costs and bearing in mind that every hospitalization day amounted to a cost of €528.95 a reduction in mean hospital stay of 4.8 days between the two years amounted to a saving of €2538.96 per patient in each admission. The saving in hospitalization days in 2017 therefore, bearing in mind that the geriatric specialist attended 98% of all FFH (422 fractures), was of €1,050,012.3. Deducting this amount from the cost of an annual gross salary of a specialist in the geriatric area, which is €32,927.36/year not including specific bonuses, the total final estimated saving for involving geriatrics in patient follow-up of hip fracture in 2017 was €1,017,084.94.
DiscussionIntegrated orthogeriatric care from 2017 in our hospital has generated considerable differences for treating our patients with FFH. Since the introduction of this multidisciplinary approach in many Spanish hospitals,10,17 closer follow-up of the patient is made, optimising their general status from admission, and considerably reducing morbimortality and hospital stay.7
Mortality after FFH has a multifactorial aetiology. Firstly, several clinical studies have found there to be an association between previous medical involvement and survival during the first few months.6,7 Secondly, the actual hip fracture has a negative impact on the patient’s health, both directly with the trauma, time between injury and surgery, presence of PU, presence of postoperative delirium, start of rehabilitation or surgical technique, and also indirectly due to the secondary postoperative risk involved. Although the rate of FFH has substantially increased in recent years due to the ageing of the population and multiple comorbidities, recent data show that mortality has dropped in the last 40 years, testifying to how effective orthogeriatric focus is.6–8
In our study we analysed the number of deaths that occurred during hospital stay, one month and one year after the fracture. We observed a trend in mortality reduction in all groups in the 2017 sample after the incorporation of orthogeriatrics. Statistically significant differences were shown in mortality during hospital stay, which was 10% in 2012 and fell to 3.6% in 2017, values which are similar to those described in the literature where intrahospital mortality of 4%–8% had been described.9,10,19 The Spanish National Health system considers this as an indicator of hospital care quality, and reducing this marker to a maximum has to be a primary aim in the OSTS. The considerable improvement in mortality during hospital stay, either prior to intervention (5.2% compared with 1.7%), during surgery or immediately after it (4.8% compared with 1.9%) may also be related to the reduction in surgical delay. A reduction in mortality after 30 days was also observed in 2017 (10.5% compared with 7%), which was similar to that recorded in the SNHFR17 in Spain that year (7.6%), and a reduction in mortality after a year (28.9% compared with 24.9%) between both groups, although these differences were not statistically significant.
Since the introduction of this multidisciplinary approach in many hospitals in our country, according to the SNHFR,17 mean hospital stay is 11 days (range between 6–20 days). In our sample we obtained a significant reduction of 4.8 days compared with 2012, achieving in 2017 a mean stay of 12.8 days, which was very close to the national mean. The relationship between surgical delay and increase in morbimortality, risk of infection and other complications is well described in the literature.18 It has been demonstrated that operating on the patient with a hip fracture within the first 24–48 h significantly lowers hospital stay, pressure ulcer rates,4,10,19 perioperative pain and medical complications, promoting return to an independent life and reducing mortality rates, especially after 30 days.4,5,8
Several international bodies have published guidelines for elderly patient management for hip fracture patients (AAOS 2014, NICE 2017, ACS TQIP Best Practice Guidelines, BC Canada, etc.) and delay to surgery is used throughout the world as a care quality and hospital performance marker. In Spain, according to SNHFR,17 in 2017, the mean delay to surgery was 3 days, with variations of between one day and 6 days, depending on the hospital. In our study the mean delay was 4.9 days. What becomes clear is the improvement in waiting times from hospital admission to surgery in 2017 compared with 2012, with a difference of 1.1 days that is statistically significant. Comparatively, our waiting times surpass the limit considered recommendable and we believe this is due to multiple factors: the need for optimization of patients prior to surgery; medical decompensations secondary to the fracture; more serious trauma-associated diseases (severe TBI, intracranial haemorrhages, etc.); time required to revert the effect of new direct-acting oral anticoagulants or platelet agents; the lack of availability of emergency operating theatres and the need to schedule patients from the waiting list.
Different studies have assessed the risk of death based on the ASA classification, reporting that those with a grade III or IV ASA had a higher risk of death compared with grade I or II ASA.20 According to SNHFR17 in 2017 over 70% of patients in Spain presented with a high anaesthetic risk (ASA III–IV). In our population sample we observe d a statistically significant increase in patient comorbidities compared with 2012, from 73% of patients ASA III–IV to 90% in 2017.
In our study we found an association between hip fracture and impairment of age-associated cognitive function. These patients are a major public health problem due to the large quantity of medical complications (respiratory or urinary infections) and delirium which increase hospital stay, causing considerable deterioration in general status and an increase in secondary risk of death.11,21 This implies the need for closer, multidisciplinary care to substantially improve patient procedures. In our sample we found there was a rise in the percentage of patients without cognitive impairment from 10.4% in 2012 to 51.2% in 2017. We believe these differences observed are due to integrated orthogeriatric management leading to an improvement in cognitive evaluation of patients. Also, our results in 2017 are similar to the mean published that year in the SNHFR16 (44.1% of patients with Pfeiffer > 3).
FFH in patients of advanced age is a known high risk factor for the development of PU,19,22 and the appropriate management and minimization of their appearance during hospital admission is a care quality marker and major predictor of mortality.23 In these patients it is very important to carry out strict control and prevention of PU, especially during the first week in hospital, since they have a negative impact on recovery,23 increasing hospital stay, healthcare costs, readmission rates and the risk of an early death.22,23 The mean rate of pressure ulcers in these patients in the literature is highly variable (between 8% and 55%),14 and in Spain it is between 7% and 14%.22 In our series we observed a tendency for PU (above grade 2) to drop by up to 4.5% in 2017 (from 10.6% in 2012 to 6.1% in 2017), although this difference was not statistically significant.
Another essential factor in the management of this type of patients is the AUR, which requires early detection and on occasion may be asymptomatic. AUE leads to many complications which may be acute (pain, discomfort and reduced state of consciousness) or delayed (urinary tract infection, sepsis and urinary incontinence).13,24 Main risk factors include the first 24 h after surgery, male sex, and increased prostate size. Also of negative impact in cognitive impairment are hypothyroidism, vascular failure, the administration of drugs such as opioids and bed rest from the hip fracture.25 AUR prevalence described in the literature is highly variable (5%–70%),13,24 and in our series was 11.3% in 2012 and 46.3% in 2017. The high difference between the two years is due to the fact that currently the orthogeriatric co-management does not use urinary catheterisation in all patients with FFH on admission, to avoid possible presentation of urinary and bacterial infections13 which would diminish the general status of our patients. We consequently observed an increase in the rate of AUR, associated with greater prevention and early diagnosis.
It is known that anaemisation is one of the common complications during the perioperative period of hip fracture patients. Its diagnosis, management and treatment is vital for recovery. Several studies found that up to 70% of these patients require perioperative allogenic blood transfusions.15,26 It has been described that the main factors influencing the reception of transfusion are age, prior comorbidities, type of fracture and surgery performed (extracapsular fractures treated with endomedullary screws are the cause of increased anaemisation)26 and haemoglobin concentration on admission.8,15 In the 2 population samples, when required, 2 red blood cell concentrates were transfused in keeping with haematology department protocol. Tranexamic acid was not used in any pre, intra or post operative cases. Close patient follow-up and presurgical optimization allowed our sample to obtain blood transfusion levels of 27.2% in 2012 and 53.1% in 2017, similar data to those found in the prospective and multicentre article by Molina Hernández et al.10 This difference may be accounted for because in 2012 the person in charge of transfusion referral was the specialist profession in OSTS. Transfusion criterion was essentially analytical, with transfusion being made when the Hb figure was equal to or lower than 8 g/dl. Criteria are now different, aimed at achieving both preoperative and postoperative optimisation to facilitate good patient progress during the whole process from fracture to functional recovery.
In our hospital if our patients are stable during the postoperative period early standing up during the first 24 h occurs. It has been described in the literature that early mobility of the operated patient is associated with better posterior mobility and early recovery of autonomy.27,28 In our series we found that in 2017 there was a 5% increase in patients who sat down on the first postoperative day, obtaining somewhat more than 90%. This point depends on the protocols of each hospital, and in fact there is a great variability between hospitals in the data obtained in the SNHFR17 in Spain from 2017.
FFH has major socioeconomic implications due to multiple factors, since it leads to greater functional impairment, reduced quality of life and loss of independence. This often gives rise to the fact that these patients need to be institutionalized, as they require greater medical and social care that involves financial costs.1 It has been described that, after 6 months, only 50%–60% of patients with FFH recover the ability to walk as they did previously and around 40% recover their previous functional status. Tight follow-up of patients and their recovery significantly impacts the need to institutionalise a patient with a hip fracture or not, but even so, despite having improved care at hospital level, in our study we observed greater institutionalisation during a 5-year period, from 4.3% in 2012 to 15.1% in 2017.
In Spain, depending on the autonomous community, direct hip fracture costs during the first year amount to between 6500 and 12,300 euros.28 Regarding hospital stay, our autonomous community is one of the ones with the highest costs derived from the same, with an approximate cost of 6500 euros per patient. Certain countries in Spain have very variable direct costs related to hip fracture, with major differences found, for example, between Poland at 1256 euros and France at 9996 euros, United Kingdom at 15,300 pounds or Switzerland at 29,910 euros28.
Healthcare systems are facing the challenge of providing these patients with appropriate medical care in the acute phase, which minimises complications, hospital stay, and the degree of social dependence and mortality through good management of financial resources. To achieve these aims it has been corroborated in the literature that the establishment of orthogeriatric units and a multidisciplinary approach to the patient with a hip fracture does not involve high hospital costs, since the efficacy of prevention and treatment options are highly relevant and associated with major cost savings.9 In our hospital, with regards to cost/benefit analysis, there was an essential difference between 2012 and 2017, leading to a total annual saving of approximately 1,000,000 euros. These finding are in line with that described by González Montalvo et al., where they report an approximate saving of 3741 euros per patient, based on hospital stays with integrated orthogeriatric care in the Community of Madrid.9 Taking into consideration the casuistry of our centre, where there are between 400 and 450 FFH per year, the total saving would be well over the million euros estimated in our study, although it should be remembered that estimated costs differ between autonomous communities.
This study has several major limitations which are inherent in its observational and retrospective nature and should be considered. In the year 2012 we had a loss of patient follow-up for those with hip fractures because they had been referred to contracted hospitals in order to avoid delay in both their final treatment and in the scheduled service programme. In 2017, following the creation of a tertiary level centre of reference for the whole healthcare area, all patients were cared for by our service and no more patients were referred elsewhere. This explains the difference in the sample size of both groups and that despite the fact all patients were included who received care from our centre and who met with inclusion and exclusion criteria, this situation constitutes a major limitation, since it could affect the comparability between the two groups, as reflected in the variables described in Table 1.
In the same way, the differences in the ASA reported in both patient groups could be due to the fact this is a tool with moderate variability, both inter and intraobserver.11 Also, this was not an evaluation tool of the number of patient comorbidities, but of their severity. For this same reason, future research studies should be made into the use of more appropriate tools, such as the Charlson Comorbidity Index, which is one of the most used predictive indexes of mortality.29,30 Furthermore, the inclusion of other more general variables of mobility could be of interest, which are inherent to hospital admission of the population of this age range and which we do not usually take into account in this study. For example, that of delirium, nosocomial infection, or other cardiovascular complications.
Furthermore, although cost/benefit analysis was not the main aim of this study, establishing an estimation of the cost difference between both periods as only the saving in hospital stays could be insufficient. For this reason, comparisons of our outcomes with the costs of other regions or countries should be cautiously viewed, since the different studies did not use uniform criteria when defining hospital care costs. For future research studies that establish cost analysis as the main study objective we would recommend the use of resources such as the Health Resource Utilization.31
ConclusionIntegrated orthogeriatric care of the patient with a fragility fracture of the hip is a more effective and more efficient care model in our area. The quality of patient care improves; satisfactory medical optimisation in the perioperative period is achieved; hospital stay length drops significantly, as does mortality during hospital stay whilst simultaneously, major financial savings in the treatment of this disease are achieved.
AuthorshipAll the authors contributed to the study concept and design. All the authors prepared the material, collected data and analysed data. The initial draft manuscript was redacted by Patricia Balvis Balvis and all the authors commented on the previous version of the document. All the authors read and approved the final draft.
Level of evidenceLevel of evidence III.
Conflict of interestsEach author certifies that they have no commercial associations (e.g. consultancy, share ownership, share participation, patent/licence agreements, etc.) that could lead to a conflict of interest relating to the presented article.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.
Please cite this article as: Balvis-Balvis PM, Dominguez-Prado DM, Ferradás-García L, Pérez-García M, Garcia-Reza A, Castro-Menendez M. Influencia de la atención ortogeriátrica integrada en la morbimortalidad y el tiempo de estancia hospitalaria de la fractura de cadera. Rev Esp Cir Ortop Traumatol. 2022;66:28–36.