Ipsilateral proximal and shaft femoral fractures typically occur in young adults after high-energy trauma. No consensus exists regarding the optimal internal fixation device or surgical strategy for these complex fractures. Our main objective is to identify differences on outcomes and complications between patients treated with one or combined implants.
Material and methodThis is a single-center retrospective cohort study in patients with associated fractures of the proximal (31 AO) and shaft femur (32 AO). We divided the patients into two groups according to the use of single (Group I) or combined implants (Group II). Demographic, clinical, radiological, surgical data and development of complications were collected.
ResultsWe identified 28 patients (19 men and 9 women) with an average age of 43 years. We used an anterograde femoral nail in group I (17 patients) and a retrograde femoral nail or a plate associated with hip lag screws or sliding hip screw in Group II (11 patients). Patients were followed up for 26.28 (9.12–62.88) months. Osteonecrosis of the femoral head, osteoarthritis, infection or nonunion was found in 9 patients (32%). No significant differences (p 0.70) were found in complications between two groups or between definitive surgical fixation before or after the first 24h.
ConclusionsNo differences in the development of complications or timing of definitive fixation were found between the use of one or combined implants in ipsilateral proximal femur and shaft fractures. Regardless of the implant chosen, an appropriate osteosynthesis technique is crucial, even so high complication rates are expected.
Level of evidence: IV. Grade of Recommendation: C.
Las fracturas ipsilaterales proximales y diafisarias del fémur suelen ocurrir en adultos jóvenes después de un traumatismo de alta energía. No existe consenso sobre el dispositivo de fijación interna óptimo o la estrategia quirúrgica para estas fracturas complejas. Nuestro principal objetivo es identificar las diferencias en los resultados y complicaciones entre los pacientes tratados con un implante o combinados.
Material y métodoEste es un estudio de cohorte retrospectivo unicéntrico en pacientes con fracturas asociadas del fémur proximal (31 AO) y diafisarias (32 AO). Dividimos a los pacientes en 2 grupos según el uso de implantes únicos (grupo i) o combinados (grupo ii). Se recogieron datos demográficos, clínicos, radiológicos, quirúrgicos y complicaciones.
ResultadosSe identificaron 28 pacientes (19 hombres y 9 mujeres) con una edad promedio de 43 años. Utilizamos un clavo femoral anterógrado en el grupo i (17 pacientes) y un clavo femoral retrógrado o una placa con tornillos a compresión o tornillo deslizante de cadera en el grupo ii (11 pacientes). Los pacientes fueron seguidos durante 26,28 (9,12-62,88) meses. Se encontró osteonecrosis de la cabeza femoral, osteoartritis, infección o seudoartrosis en 9 pacientes (32%). No se encontraron diferencias significativas (p=0,70) en las complicaciones entre los 2 grupos o entre la fijación quirúrgica definitiva antes o después de las primeras 24h.
ConclusionesNo se encontraron diferencias en el desarrollo de complicaciones o el momento de la fijación definitiva entre el uso de un implante o combinado en fracturas ipsilaterales de fémur proximal y diafisario. Independientemente del implante elegido, una técnica de osteosíntesis adecuada es crucial; aun así son esperables altas tasas de complicaciones.
Ipsilateral proximal and shaft femoral fractures typically occur in young adults after high-energy trauma, frequently involving multiple associated orthopedic and visceral injuries.1 This fracture pattern was first described in 1953 and since then, studies have shown that between 2 and 9% of femoral shaft fractures (FSF) associate an ipsilateral proximal femur fracture (PFF).2 The classic pattern presents a nondisplaced or minimally displaced PFF, even leading to misdiagnosis on initial assessment and a displaced and obvious FSF. Surgical options for PFF include cannulated screws (CS), sliding hip screw (SHS), hook plates and cephalomedullary nail fixation, while intramedullary nailing (IMN) has long been the gold standard for FSF.3 However, when both fractures come together, no consensus exists regarding the best surgical treatment,4 being much more challenging than the surgical management of FSF or PFF when appear separately, because each fracture conditions the other.
The anatomical reduction and stable internal fixation should be the goal of treatment in PFF.5 One of the main debates is about the use of one or combined implants in this complex pattern of fractures,6 and no consensus exists regarding which implants provide the best results.7–9 We need implants that permit us to make compression in PFF (CS, SHS or new cephalomedullary nails). Not only should we analyze the implant selection for these fractures, but also the optimal timing and sequence of fixation. Although some studies determined that early fixation decreases morbidity and mortality and allows for early patient mobilization and rehabilitation,4 it is necessary to know that management of these patients must be frequently adapted to the polytrauma context.10 It is imperative to treat some urgent life-threatening associated injuries that might delay definitive surgical treatment of these fractures.11
Our main objective is to describe our results and to identify if there are differences on outcomes and complications between patients treated with single or combined implants in ipsilateral proximal and shaft femoral fractures. We aim to determine what type of patients can benefit from one or another type of internal osteosynthesis according to the characteristics of the fracture, and whether there are differences in complications (hypothesis). Our secondary objectives are to describe the fracture patterns and to determine if the severity of patient's injuries might delay definitive surgical treatment of this complex femur fractures, and if it consequently entails a higher rate of complications during follow-up.
Material and methodThis is a single-center retrospective cohort study of the patients with ipsilateral PFF and FSF; subtypes 31 and 32 respectively, according to AO Foundation/Orthopaedic Trauma Association (AO/OTA) classification.12 A systematic search was carried out in the Orthopedic-Trauma Unit database of our hospital, including trauma patients of the last 15 years. Patient information were analyzed from our hospital software HCIS (Health Care Information System) and from charts in paper format. All patients were virtually reviewed during February 2021, with a minimum follow-up time of 6 months. The study was approved by the Clinical Research Ethics Committee (CREC). The retrospective nature of the study and the anonymization of patients’ data made unnecessary to have a signed consent form.
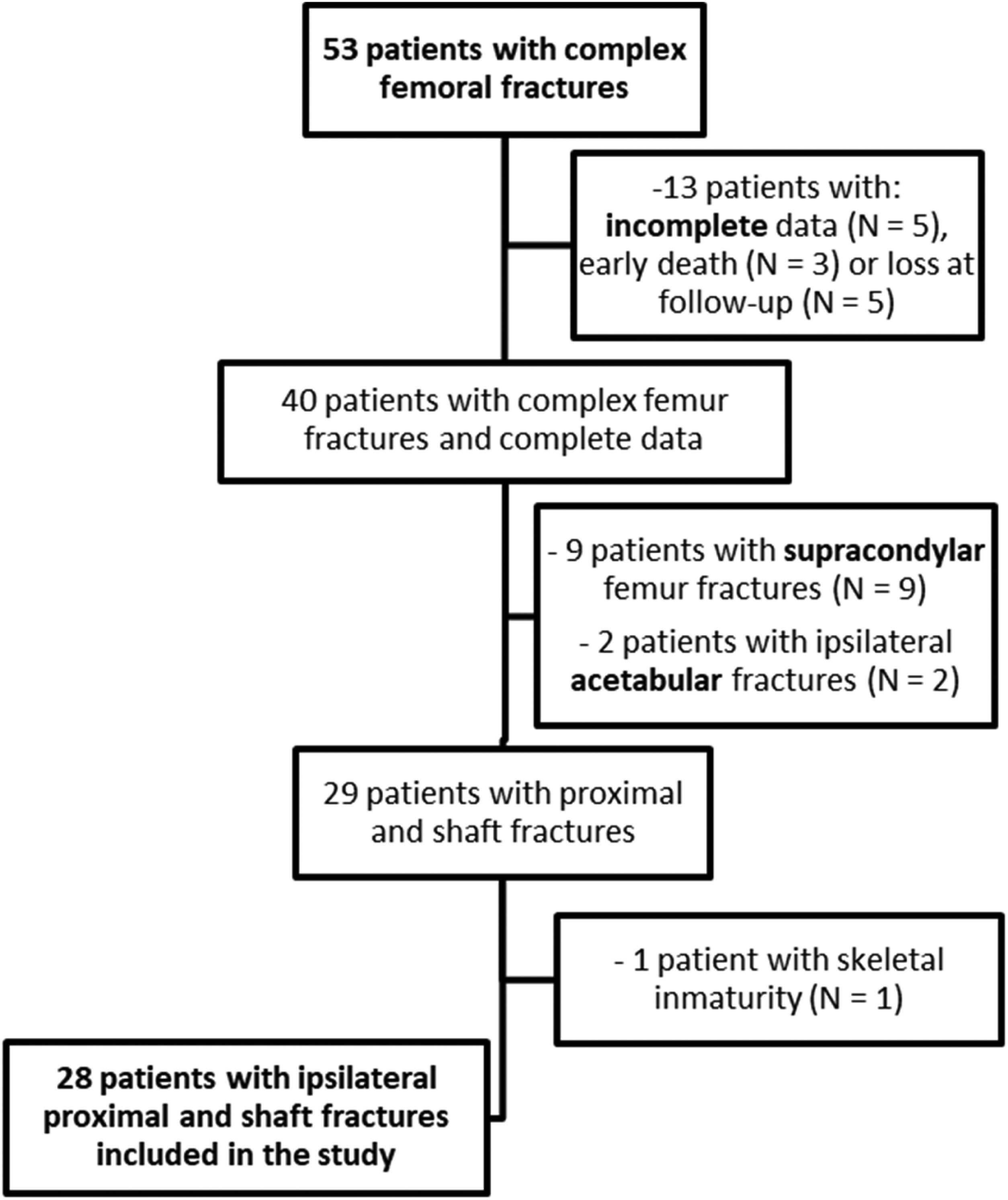
Three groups of patients were excluded: 1. Patients with incomplete data, death during initial assessment or inadequate follow-up. 2. Patients with an ipsilateral acetabular fracture associated or with a supracondylar femur fracture (33 AO/OTA) rather than a FSF (32 AO/OTA). 3. Patients with skeletal immaturity (open physis), as it was not the aim of the study and because of the need of specific internal osteosynthesis devices. It was not possible to exclude patients with associated injuries, virtually all of the patients presented associated injuries (Fig. 1).
Patients were divided in two groups. Group I included patients treated with a single implant and Group II included patients managed with combined implants. Demographic and clinical variables of the patients were collected in a database for subsequent analysis; we included sex, age, laterality, injury mechanism, fractures in other anatomical regions and ipsilateral knee injuries, associated systemic injuries, New Injury Severity Score (NISS) and Injury Severity Score (ISS).13,14
All patients included were admitted in the Intensive Care Unit (ICU) for initial management and were evaluated according to Advanced Trauma Life Support (ATLS) protocol. Preoperatively, anteroposterior (AP) view of the pelvis and AP and lateral view of the complete femur were obtained. The decision of making a CT scan of the hip was determine by the patient's condition in the ICU: whole body CT on the initial assessment or hip CT preoperatively ordered by the surgeon. To provide radiologic information on the PFF (31 AO/OTA), we described displacement according to the Garden classification and type of fracture according to the Pauwels classification.15 In FSF (32 AO/OTA), the degree of comminution was collected according to the Winquist classification.
We also collected data about the initial assessment; we recorded the presence of open fractures, provisional external fixation, acute compartment syndrome, deep vein thrombosis (DVT) or pulmonary embolism (PE), fat embolism syndrome and emergent definitive surgical fixation. Moreover, we recorded the time to definitive surgery and we collected variables regarding surgical treatment: the need of open reduction techniques, patient position on the operating room, type of implant, anterograde or retrograde IMN, CS, SHS or plates. We also searched for the ICU and length of hospitalization time.
Finally, we studied fracture union time, postoperative weight bearing and complications in the follow-up. We considered infection, avascular necrosis (AVN), nonunion and hip osteoarthritis as major complications; and osteosynthesis implant removal and malreduction or malunion as minor complications. Owing to the high incidence of visceral and orthopedic injuries, it was not possible to make a thorough evaluation of functional outcomes; consequently, the only comparable variable between patients that we collected was the ability to walk at the end of the follow-up.
Femoral fractures were considered healed when anteroposterior and lateral radiographs showed that three of four cortices had trabeculae bridging the fracture site. Nonunion was defined by persistence of the fracture line at 6 months after the index procedure, without progressive callus formation and/or failure of fixation with broken implant. We considered a malunion when femoral neck-shaft angle is greater than 5° compared with the contralateral side and when there is more than 10° deviation in sagittal or coronal plane in FSF.
Definitive surgery was performed by three experienced trauma surgeons from the Orthopedic-Trauma Unit and the timing was determined by the stabilization of the medical condition of the polytraumatized patient. We used to implant a simple device for nondisplaced or minimally displaced PFF and a combined device for displaced PFF. However, the final implant choice and order of fixation were decided by the preference and experience of each surgeon. All patients received antibiotic prophylaxis and subcutaneous prophylactic low-molecular-weight heparin. Most patients have been followed-up with medical examination at 1, 3, 6 and 12 months, as well as annually since then to rule out any complication. Postoperative care was custom decided by the main surgeon, taking into consideration variables such as bone quality, mechanical stability of the implant and the presence of concomitant fractures in lower extremities.
A descriptive study of all variables (demographic, temporal, clinical and surgical assessment and outcomes) was carried out. Qualitative variables were described by absolute frequency and percentage. Quantitative variables were described by measures of central tendency (mean) and dispersion (SD). Subsequently, a univariate analysis using Chi-square or Fisher's exact test for the qualitative variables and Student t test or Mann–Whitney U test for quantitative variables was performed (depending on whether or not a normal distribution, evaluated by Kolmogorov–Smirnov test, can be assumed). Two-sided P-value<0.05 was considered significant. The relationship between NISS scale, length of ICU hospitalization and time to definitive surgical intervention was analyzed using Pearson's correlation. Data were analyzed using statistical package IBM SPSS Statistics 21.0. Regarding the sample size, based on previous studies and on the annual incidence in our hospital, the estimated incidence of subjects meeting inclusion and exclusion criteria to participate in the study was 2–3 patients per year, so patients had to be recruited for a long period of time (at least 15 years).
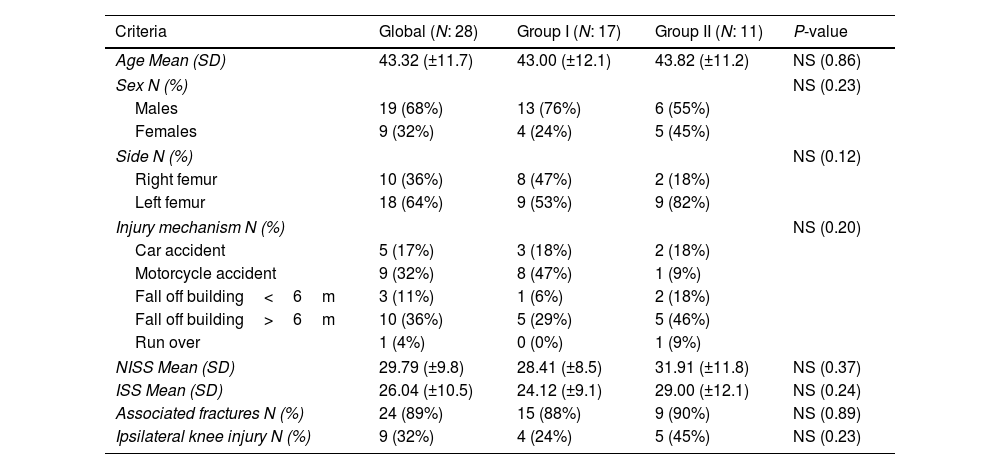
ResultsWe identified 28 patients who suffered ipsilateral PFF and FSF with an average age of 43 years (SD 11.7), there were 19 males and 9 females. All patients suffered high-energy accidents. The average ISS and NISS were respectively 26 (SD 9.8) and 29.7 (SD 10.5). There were 24 patients (89%) who had associated fractures in extremities and 9 patients (32%) who had ipsilateral knee injuries (2 ligamentous injuries, 1 tibial plateau fracture and 6 patellar fractures). 17 patients were included in Group I (single implant) and 11 patients in Group II (combined implants). There were no significant differences between the two groups in those parameters (Table 1).
Patient demographics. Comparison Group I (single implant) and Group II (combined implant).
| Criteria | Global (N: 28) | Group I (N: 17) | Group II (N: 11) | P-value |
|---|---|---|---|---|
| Age Mean (SD) | 43.32 (±11.7) | 43.00 (±12.1) | 43.82 (±11.2) | NS (0.86) |
| Sex N (%) | NS (0.23) | |||
| Males | 19 (68%) | 13 (76%) | 6 (55%) | |
| Females | 9 (32%) | 4 (24%) | 5 (45%) | |
| Side N (%) | NS (0.12) | |||
| Right femur | 10 (36%) | 8 (47%) | 2 (18%) | |
| Left femur | 18 (64%) | 9 (53%) | 9 (82%) | |
| Injury mechanism N (%) | NS (0.20) | |||
| Car accident | 5 (17%) | 3 (18%) | 2 (18%) | |
| Motorcycle accident | 9 (32%) | 8 (47%) | 1 (9%) | |
| Fall off building<6m | 3 (11%) | 1 (6%) | 2 (18%) | |
| Fall off building>6m | 10 (36%) | 5 (29%) | 5 (46%) | |
| Run over | 1 (4%) | 0 (0%) | 1 (9%) | |
| NISS Mean (SD) | 29.79 (±9.8) | 28.41 (±8.5) | 31.91 (±11.8) | NS (0.37) |
| ISS Mean (SD) | 26.04 (±10.5) | 24.12 (±9.1) | 29.00 (±12.1) | NS (0.24) |
| Associated fractures N (%) | 24 (89%) | 15 (88%) | 9 (90%) | NS (0.89) |
| Ipsilateral knee injury N (%) | 9 (32%) | 4 (24%) | 5 (45%) | NS (0.23) |
New Injury Severity Score (NISS), Injury Severity Score (ISS), Intensive Care Unit (ICU). N=number of patients with available data.
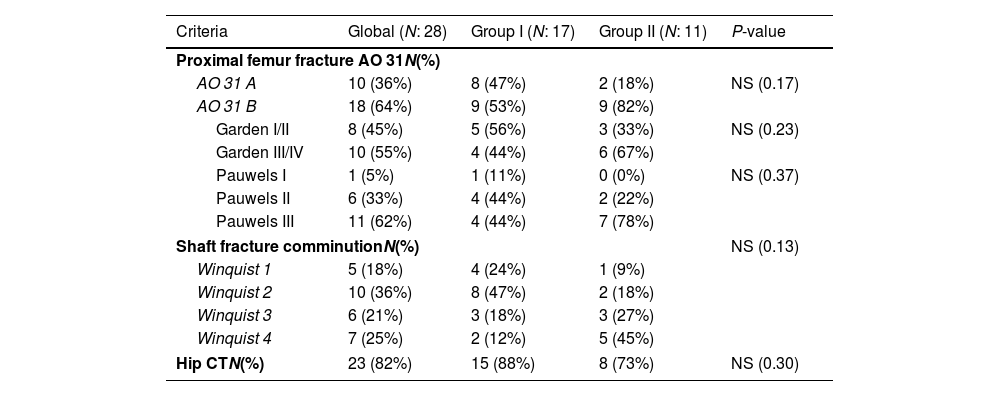
About the PFF, there were 10 (36%) OTA 31-A and 18 (64%) OTA 31-B PFF types. The predominant pattern of fracture was OTA 31-B, of which 3 patients had subcapital (31-B1), 8 transcervical (31-B2) and 7 basicervical fractures (31-B3). The neck fracture is usually vertically oriented, 11 were Pauwels type III. About fracture displacement, 45% were Garden type I/II and 55% Garden type III/IV, without differences between two groups. In relation with FSF, 10 were OTA 32-A (36%), 13 OTA 32-B (46%), and 5 (18%) OTA 32-C. According to the Hansen–Winquist classification, 5 (18%) were type I, 10 (36%) type II, 6 (21%) type III and 7 (25%) type IV (Table 2). We can see in Table 2 that 9 of 11 (82%) patients in Group II had 31-B intracapsular fractures while only 9 of 17 (53%) in Group I (p 0.17). It should be pointed out that, between the displaced intracapsular fractures, 6 of them were treated with combined implants (Group II) and 4 with a single implant (Group I), in comparison with the non-displaced ones: 3 treated with double implant (Group II) and 5 with single implant (Group I). In relation with FSF, greater comminution of the shaft was observed in Group II, without statistical significance (p 0.13).
Characteristics of ipsilateral fractures. Comparison Group I (single implant) and Group II (combined implant).
| Criteria | Global (N: 28) | Group I (N: 17) | Group II (N: 11) | P-value |
|---|---|---|---|---|
| Proximal femur fracture AO 31N(%) | ||||
| AO 31 A | 10 (36%) | 8 (47%) | 2 (18%) | NS (0.17) |
| AO 31 B | 18 (64%) | 9 (53%) | 9 (82%) | |
| Garden I/II | 8 (45%) | 5 (56%) | 3 (33%) | NS (0.23) |
| Garden III/IV | 10 (55%) | 4 (44%) | 6 (67%) | |
| Pauwels I | 1 (5%) | 1 (11%) | 0 (0%) | NS (0.37) |
| Pauwels II | 6 (33%) | 4 (44%) | 2 (22%) | |
| Pauwels III | 11 (62%) | 4 (44%) | 7 (78%) | |
| Shaft fracture comminutionN(%) | NS (0.13) | |||
| Winquist 1 | 5 (18%) | 4 (24%) | 1 (9%) | |
| Winquist 2 | 10 (36%) | 8 (47%) | 2 (18%) | |
| Winquist 3 | 6 (21%) | 3 (18%) | 3 (27%) | |
| Winquist 4 | 7 (25%) | 2 (12%) | 5 (45%) | |
| Hip CTN(%) | 23 (82%) | 15 (88%) | 8 (73%) | NS (0.30) |
N=number of patients with available data.
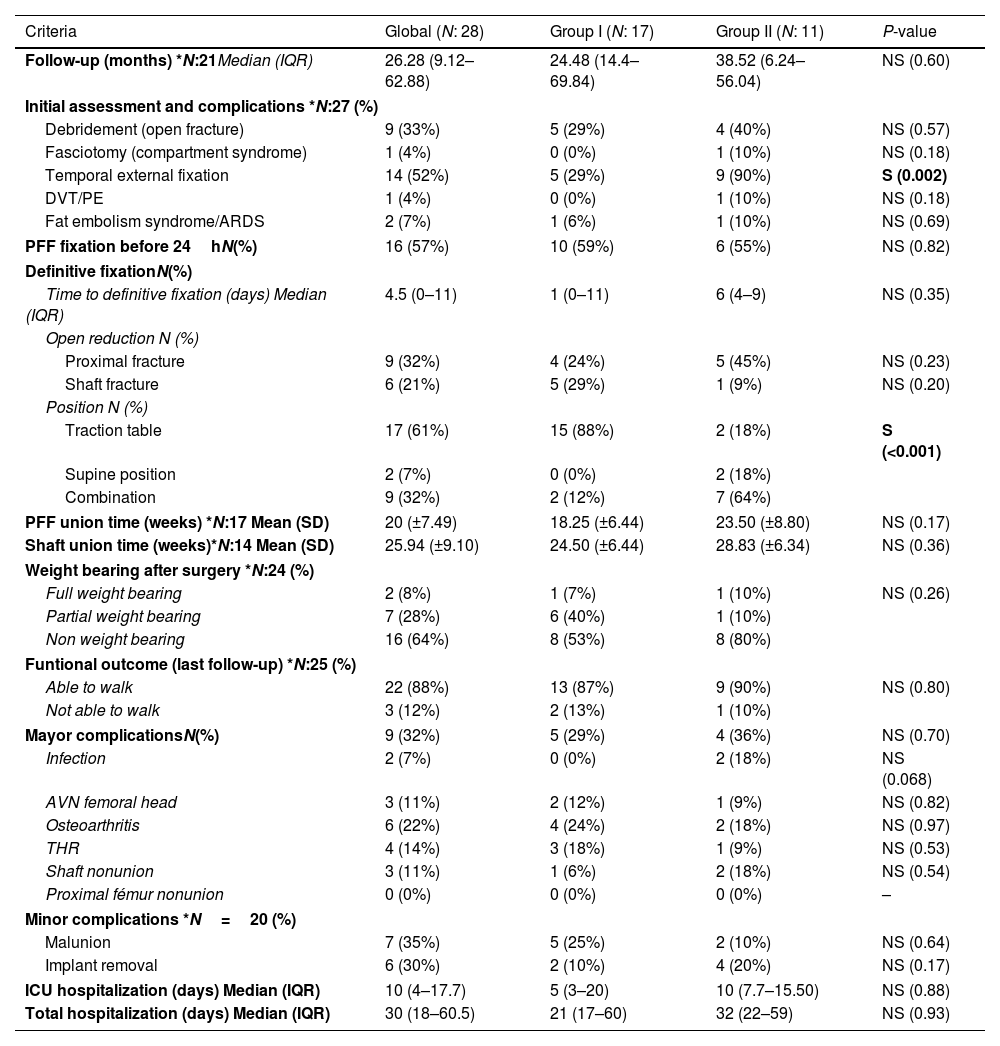
About the initial management, nine of the FSF (33%) were open fractures and needed irrigation and debridement, and there was one patient (4%) with acute compartment syndrome of the thigh treated with fasciotomies. 14 patients were treated with damage control orthopedics (DCO) strategy, 9 of Group II (90%) and 5 of Group I (29%) with significant difference (p 0.002). About the acute complications, there were 1 DVT and 2 fat embolism syndromes. Open reduction was performed in 9 (32%) PFF and in 6 (21%) FSF. Patient position in the operating room was related with surgical procedure: traction table was used in 15 of the 17 patients (88%) of group I, while in group II the majority (64%) underwent a two stages position (supine position and traction table), with statistically significant difference (p<0.001). Mean time from injury to definitive fixation was 4.5 (0–11) days without difference in two groups. Globally, 16 patients (57%) went on PFF fixation in first 24h after injury, without statistically signification (p 0.82) between Group I (10 patients, 59%) and Group II (6 patients, 55%) (Table 3).
Many different implants were used for fixation of the fractures. Group I included 17 patients who underwent surgery with anterograde femoral nail: 14 long proximal femoral nail (PFN or PFNA, Synthes) and 3 Trigen Meta-TAN nail (S&N). Group II included 11 patients, 9 of them underwent surgery with a retrograde femoral Trigen Meta-Nail (S&N) for the FSF combined with other devices for the PFF: 2 patients with cancellous lag screws (7.3mm CS, Synthes) and 7 with proximal femoral plates [4 Classic Compression Hip Screw CHS/AMBI (S&N), 2 Dynamic Hip Screw DHS (Synthes) and 1 proximal femoral hook plate (LCP, Synthes)] combined in 5 of the 7 cases with an additional cancellous screw. Two patients of group II were treated with a proximal device (one with CS and the other with PFNA) and a plate for the shaft (one with a long DHS, Synthes, and the other with a LCP plate, Synthes).
About the complications, patients were followed up for a mean time of 26.28 (9.12–62.88) months. PFF (N=17) healed at an average union time of 20 weeks (SD: 7.4 weeks). A longer average union time was found in Group II, 23.50 weeks vs 18.25 weeks in Group I, but the difference wasn’t statistically significant (p 0.17). In FSF, excluding the data from 3 nounions (N=14), the average union time was 25.94 weeks (SD: 9.1 weeks). Most patients performed partial (28%) or non (64%) weight bearing during first 6–8 weeks. Almost 90% of patients (22 of 25 patients) were able to walk at the last follow-up date (Table 3).
The major orthopedic complications (Tables 3 and 4) included 3 osteonecrosis of the femoral head with cortical collapse Grade III–IV Ficat and Arlet (11%), developing osteoarthritis in 2 of them. The most frequent major complication was osteoarthritis, found in 5 cases (18%), 4 of them underwent a total hip replacement (THR). There were 2 infections (7%) that required reintervention, both of them were initially treated with DCO strategy in group II (p 0.068) and one of them was an open FSF. In one of the infection cases, 5 reoperations were required for irrigation, debridement and implant removal after union, ending in early osteoarthritis and THR carried out in two stages; in the other infection case a two stages replacement was performed with a PMMA spacer with gentamicin and subsequent new thicker nailing. Shaft fracture nonunion was observed in 3 patients (11%): one was the infection mentioned previously, and the other two nonunions which required new surgery with reaming and insertion of a thicker nail. No periimplants fractures were observed.
Surgical treatment and complications. Comparison Group I (single implant) and Group II (combined implant).
| Criteria | Global (N: 28) | Group I (N: 17) | Group II (N: 11) | P-value |
|---|---|---|---|---|
| Follow-up (months) *N:21Median (IQR) | 26.28 (9.12–62.88) | 24.48 (14.4–69.84) | 38.52 (6.24–56.04) | NS (0.60) |
| Initial assessment and complications *N:27 (%) | ||||
| Debridement (open fracture) | 9 (33%) | 5 (29%) | 4 (40%) | NS (0.57) |
| Fasciotomy (compartment syndrome) | 1 (4%) | 0 (0%) | 1 (10%) | NS (0.18) |
| Temporal external fixation | 14 (52%) | 5 (29%) | 9 (90%) | S (0.002) |
| DVT/PE | 1 (4%) | 0 (0%) | 1 (10%) | NS (0.18) |
| Fat embolism syndrome/ARDS | 2 (7%) | 1 (6%) | 1 (10%) | NS (0.69) |
| PFF fixation before 24hN(%) | 16 (57%) | 10 (59%) | 6 (55%) | NS (0.82) |
| Definitive fixationN(%) | ||||
| Time to definitive fixation (days) Median (IQR) | 4.5 (0–11) | 1 (0–11) | 6 (4–9) | NS (0.35) |
| Open reduction N (%) | ||||
| Proximal fracture | 9 (32%) | 4 (24%) | 5 (45%) | NS (0.23) |
| Shaft fracture | 6 (21%) | 5 (29%) | 1 (9%) | NS (0.20) |
| Position N (%) | ||||
| Traction table | 17 (61%) | 15 (88%) | 2 (18%) | S (<0.001) |
| Supine position | 2 (7%) | 0 (0%) | 2 (18%) | |
| Combination | 9 (32%) | 2 (12%) | 7 (64%) | |
| PFF union time (weeks) *N:17 Mean (SD) | 20 (±7.49) | 18.25 (±6.44) | 23.50 (±8.80) | NS (0.17) |
| Shaft union time (weeks)*N:14 Mean (SD) | 25.94 (±9.10) | 24.50 (±6.44) | 28.83 (±6.34) | NS (0.36) |
| Weight bearing after surgery *N:24 (%) | ||||
| Full weight bearing | 2 (8%) | 1 (7%) | 1 (10%) | NS (0.26) |
| Partial weight bearing | 7 (28%) | 6 (40%) | 1 (10%) | |
| Non weight bearing | 16 (64%) | 8 (53%) | 8 (80%) | |
| Funtional outcome (last follow-up) *N:25 (%) | ||||
| Able to walk | 22 (88%) | 13 (87%) | 9 (90%) | NS (0.80) |
| Not able to walk | 3 (12%) | 2 (13%) | 1 (10%) | |
| Mayor complicationsN(%) | 9 (32%) | 5 (29%) | 4 (36%) | NS (0.70) |
| Infection | 2 (7%) | 0 (0%) | 2 (18%) | NS (0.068) |
| AVN femoral head | 3 (11%) | 2 (12%) | 1 (9%) | NS (0.82) |
| Osteoarthritis | 6 (22%) | 4 (24%) | 2 (18%) | NS (0.97) |
| THR | 4 (14%) | 3 (18%) | 1 (9%) | NS (0.53) |
| Shaft nonunion | 3 (11%) | 1 (6%) | 2 (18%) | NS (0.54) |
| Proximal fémur nonunion | 0 (0%) | 0 (0%) | 0 (0%) | – |
| Minor complications *N=20 (%) | ||||
| Malunion | 7 (35%) | 5 (25%) | 2 (10%) | NS (0.64) |
| Implant removal | 6 (30%) | 2 (10%) | 4 (20%) | NS (0.17) |
| ICU hospitalization (days) Median (IQR) | 10 (4–17.7) | 5 (3–20) | 10 (7.7–15.50) | NS (0.88) |
| Total hospitalization (days) Median (IQR) | 30 (18–60.5) | 21 (17–60) | 32 (22–59) | NS (0.93) |
Deep vein thrombosis (DVT), pulmonary embolism (PE), acute respiratory distress syndrome (ARDS), proximal femoral fracture (PFF), avascular necrosis (AVN), total hip replacement (THR). N=number of patients with available data.
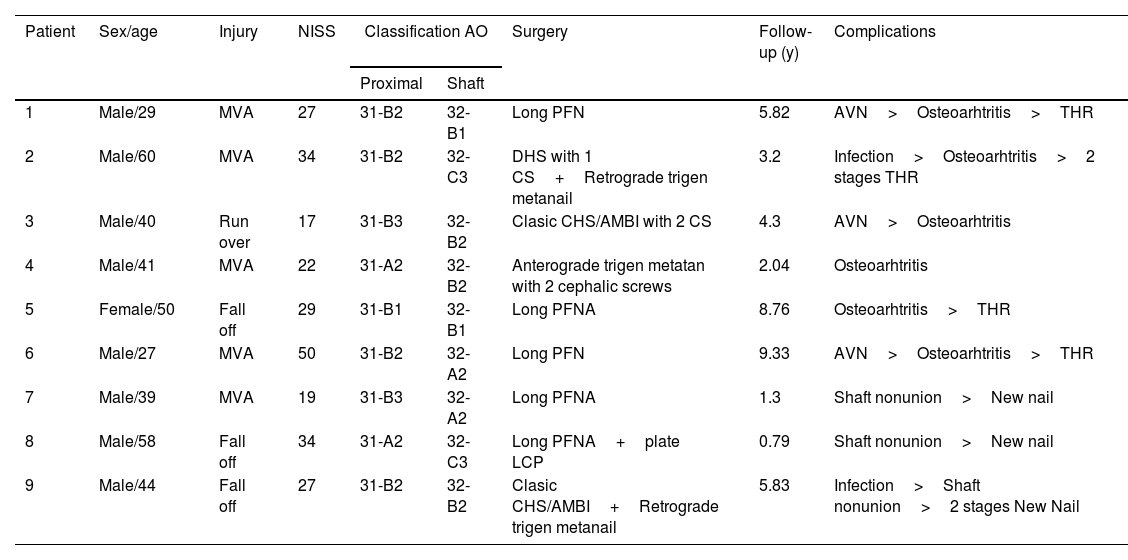
Main characteristics of patients with complications and surgical solicitations.
| Patient | Sex/age | Injury | NISS | Classification AO | Surgery | Follow-up (y) | Complications | |
|---|---|---|---|---|---|---|---|---|
| Proximal | Shaft | |||||||
| 1 | Male/29 | MVA | 27 | 31-B2 | 32-B1 | Long PFN | 5.82 | AVN>Osteoarhtritis>THR |
| 2 | Male/60 | MVA | 34 | 31-B2 | 32-C3 | DHS with 1 CS+Retrograde trigen metanail | 3.2 | Infection>Osteoarhtritis>2 stages THR |
| 3 | Male/40 | Run over | 17 | 31-B3 | 32-B2 | Clasic CHS/AMBI with 2 CS | 4.3 | AVN>Osteoarhtritis |
| 4 | Male/41 | MVA | 22 | 31-A2 | 32-B2 | Anterograde trigen metatan with 2 cephalic screws | 2.04 | Osteoarhtritis |
| 5 | Female/50 | Fall off | 29 | 31-B1 | 32-B1 | Long PFNA | 8.76 | Osteoarhtritis>THR |
| 6 | Male/27 | MVA | 50 | 31-B2 | 32-A2 | Long PFN | 9.33 | AVN>Osteoarhtritis>THR |
| 7 | Male/39 | MVA | 19 | 31-B3 | 32-A2 | Long PFNA | 1.3 | Shaft nonunion>New nail |
| 8 | Male/58 | Fall off | 34 | 31-A2 | 32-C3 | Long PFNA+plate LCP | 0.79 | Shaft nonunion>New nail |
| 9 | Male/44 | Fall off | 27 | 31-B2 | 32-B2 | Clasic CHS/AMBI+Retrograde trigen metanail | 5.83 | Infection>Shaft nonunion>2 stages New Nail |
Motor vehicle accident (MVA), New Injury Severity Score (NISS), proximal femoral nail (PFN) or PFN antirrotation (PFNA, Synthes), canulated screws (CS, Synthes), dinamic hip screw (DHS, synthes), compression hip screw (CHS/AMBI, S&N), retrograde trigen metanail (S&N), locking compression plate (LCP, Synthes), avascular necrosis (AVN).
There were no significant differences (p 0.70) in major complications between groups, that responds to the main objective of the study. No statistically significant association (p 0.49) was found between major complications and the type of PFF (31-A vs 32-B) (Table 3). However, it was found that the use of combined implants predominates in intracapsular fractures (31-B) without statistical significance (p 0.13) and in greater complexity and comminution shaft fractures (32-B or C), without statistical significance (p 0.081). About other objective of the study there were 6 cases of major complications between the PFF operated in less than 24h and only 3 in the ones operated after the first day, without statistical difference (p 0.68).
About the considered minor complications, 2 patients in Group I and 4 in Group II needed osteosynthesis implant removal. We found 5 malreductions in Group I, 3 of the PFF and 2 of the FSF; and 2 in Group II, both in the PFF, without statistically significant difference (p 0.64) (Table 3). None of them needed second surgery or have a clinical impact in the follow-up. Between the 5 PFF malreduction, 4 had a substantial displacement in the initial assessment and it was impossible to obtain a perfect reduction.
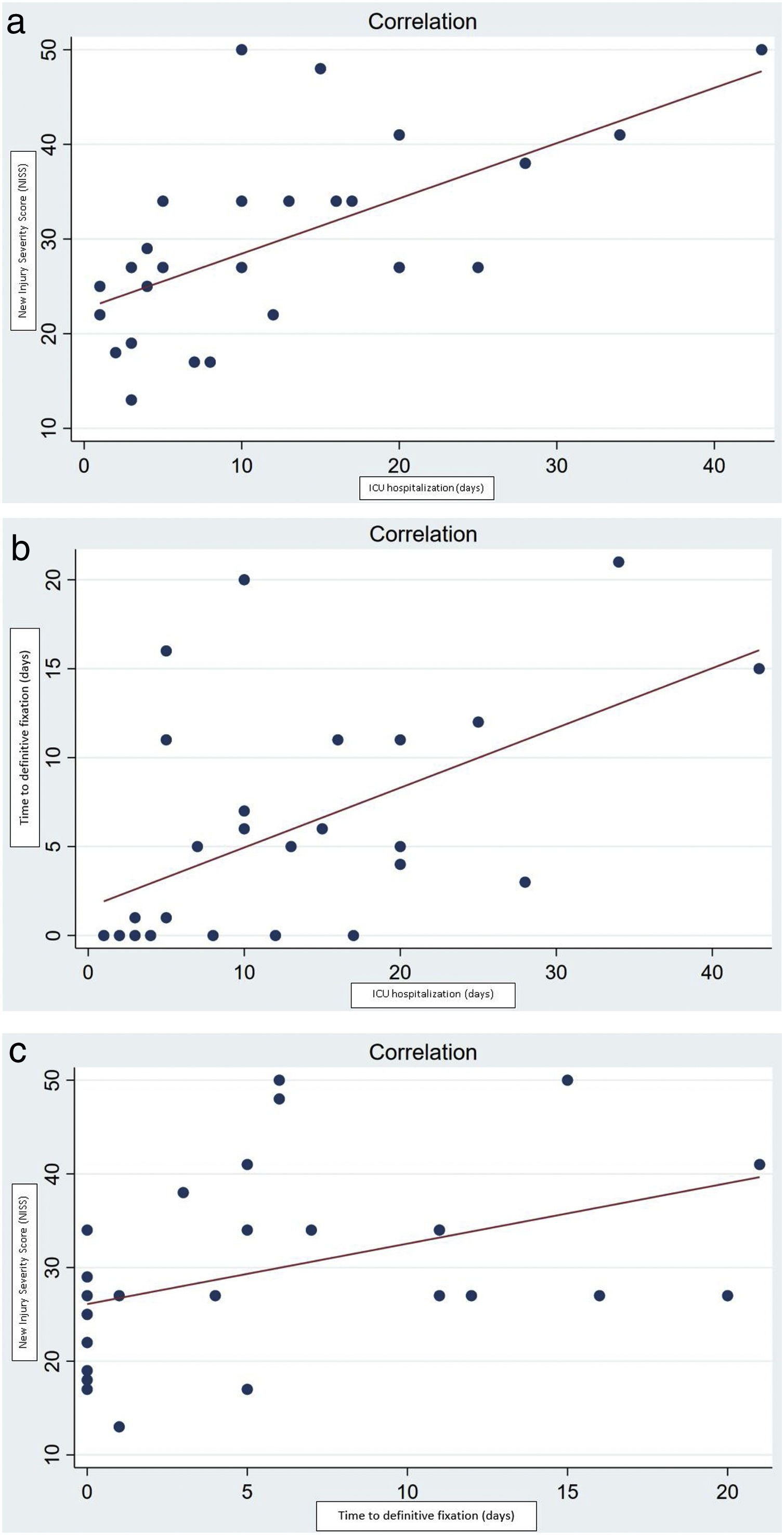
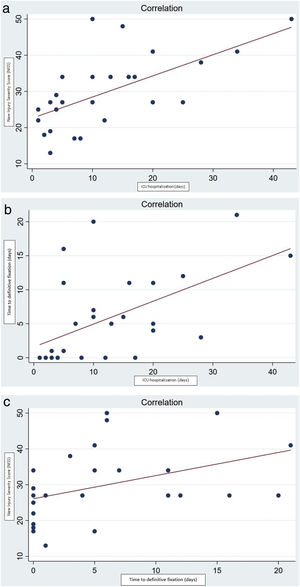
We found a positive Pearson's correlation between NISS score and ICU hospitalization (p 0.0004, Fig. 2), positive correlation between time to definitive fixation and ICU hospitalization (p 0.0025, Fig. 3) and positive correlation between NISS score and time to definitive fixation (p 0.0247, Fig. 4). These 3 variables were related to the appearance of major complications (N=9) without statistical signification for any of them: time to definitive surgery (p 0.92), ICU hospitalization (p 0.64) and NISS (p 0.72).
(a) Positive Pearson correlation (value=0.624) between scores on the New Injury Severity Score (NISS) and length of ICU hospitalization (p=0.0004). (b) Positive Pearson correlation (value=0.548) between time to definitive fixation and length of ICU hospitalization (p=0.0025). (c) Positive Pearson correlation (value=0.424) between scores on the New Injury Severity Score (NISS) and time to definitive fixation (p=0.0247).
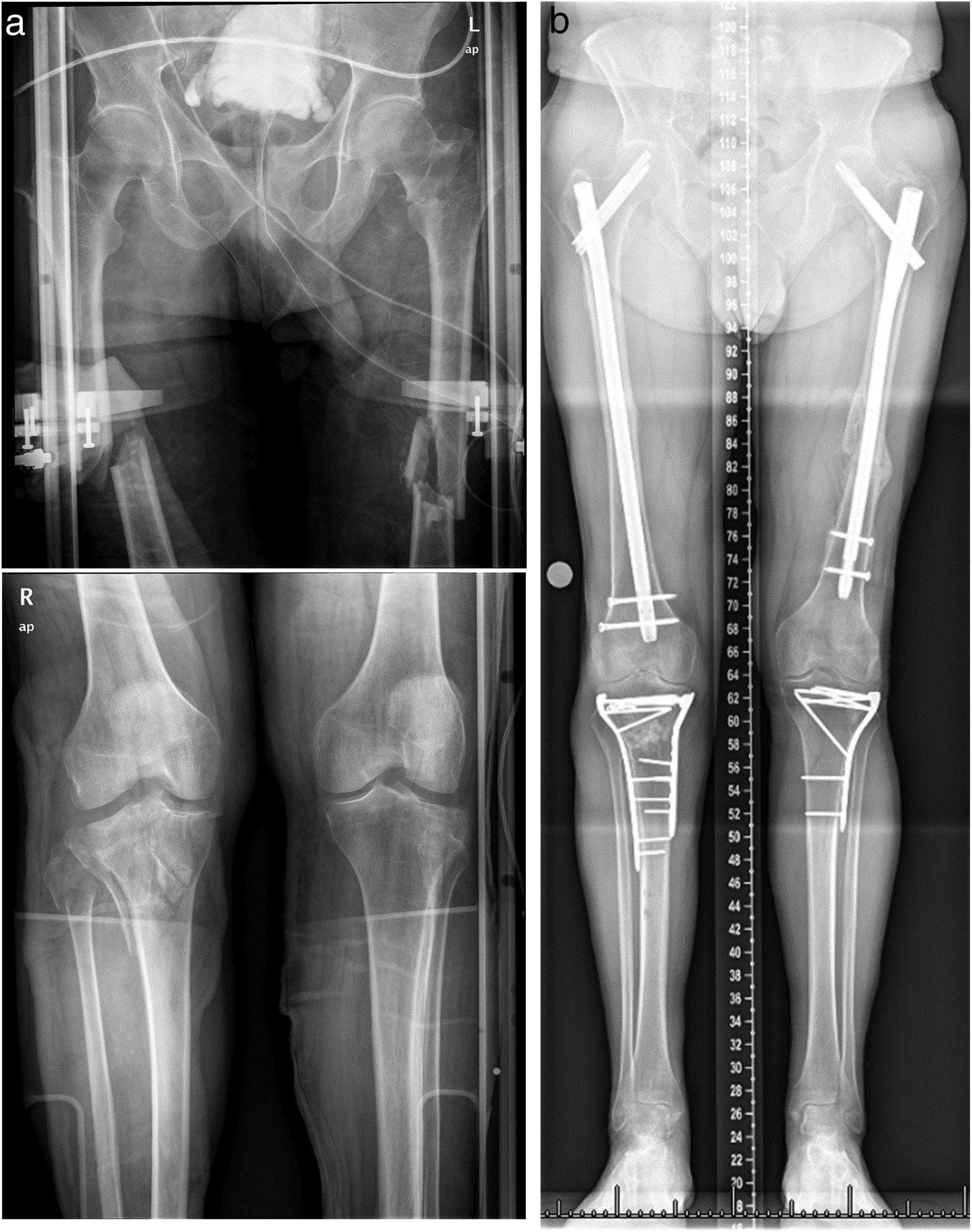
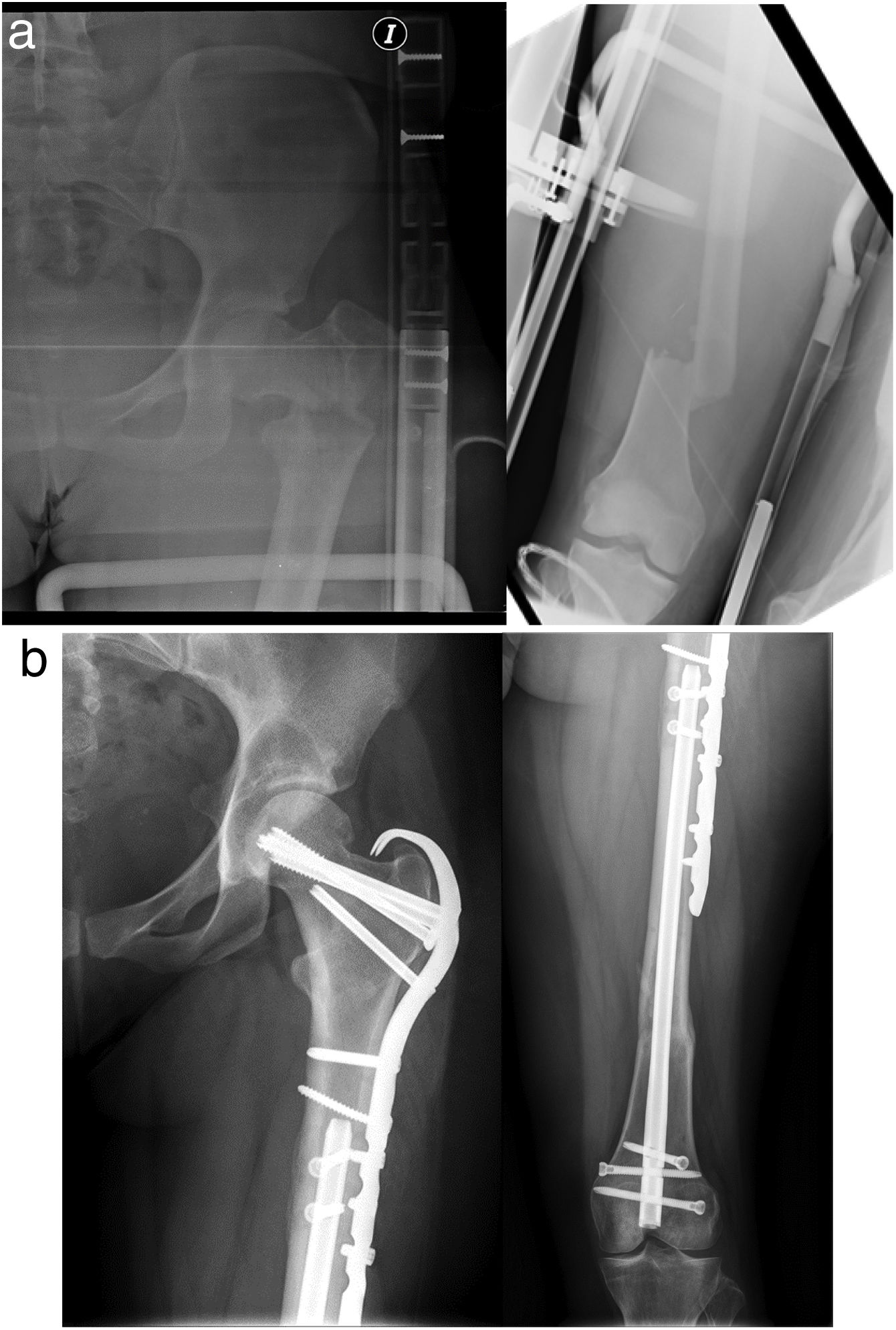
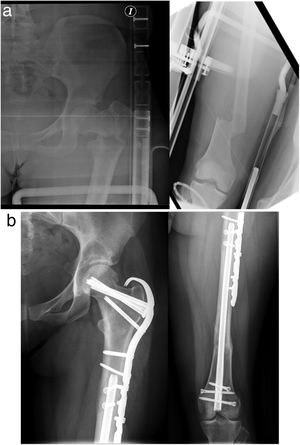
(a) Pre-operative AP radiographs of a 64-year-old man showing pertrochanteric fracture 31-A1 and ipsilateral comminuted shaft fracture 32-B2 in left femur, contralateral FSF and bilateral tibial plateau fractures. (b) Post-operative AP radiographs showing fixation with a long proximal femoral nail PFNA (DePuy Synthes) in left femur.
(a) Pre-operative AP radiographs of a 24-year-old woman with a complex proximal femoral fracture and ipsilateral shaft fracture 32-A3. (b) Post-operative AP radiographs showing fixation with retrograde femoral trigen Meta-Nail (S&N) for the FSF combined with a hook locking compression plate (LCP, DePuy Synthes) with two interfragmentary compression cancellous screw (CS).
Ipsilateral femoral neck and shaft fractures are relatively uncommon injuries, the most frequently reported incidence oscillates between 2% and 9%, but in various modern series the incidence of the combination is approximately 3% of all the FSF.11,16 In our study we were unable to give an approximated incidence in our center.
Since the first case report17 in 1953, numerous case series have called the attention to this combination of fractures and have given us information on the most frequent injury patterns. This pattern of injury usually occurs as a result from high-energy trauma in young males, therefore the percentage of associated systemic and orthopedic lesions is high. With regard to bone injury, the FSF is usually comminuted and located in the middle third of the diaphysis and the PFF is typically basicervical, sparsely displaced and vertically oriented. Globally in our study, these demographic parameters and lesion morphology characteristics are met.
One of the features of interest in our series is the 100% of preoperative diagnosis of proximal femur fractures. This efficiency is based on a high level of suspicion, an exhaustive evaluation of simple X-rays or a liberal request for a CT scan if deemed necessary. In recent series the percentage of delayed diagnosis ranges between 0 and 26%4,18 and it has been clear that basing the diagnosis exclusively on the use of CT does not ensure the proper diagnosis. If CT is performed it should be thin cut, high resolution, and it must be thoroughly studied in both coronal and sagittal planes.11
The absence of an accepted classification and the lack of quality scientific evidence leads to a great variety in the strategies of fixation. In fact, in our study a solid treatment protocol cannot be establish, as the final decision depended on the fracture pattern of our cases and the experience of leading surgeons. However, there were two fundamental decisions on which we would like to offer some tips: the use of simple or combined implants and the time of definitive surgery.
When a single implant is used, the most common is the long anterograde cephalomedullary nail, classically used in cases when the PFF is pertrochanteric and sparsely displaced. The most paradigmatic case for the use of a double implant is the presence of a displaced FSF associated with a displaced intracapsular PFF, and in these cases the most frequent combination is the retrograde femoral nail associated with a proximal implant (isolated CS or SHS). In our study, no significant differences were observed between the type of fracture and the use of single or combined implants, but a clear tendency to use one implant was identified in cases with 31A and non-displaced 31B PFF.
About the timing of definitive fixation in our series, it depended on the associated injuries, which were very common in our patients. The greater severity of patient in group II, measured by the NISS scale, was related to a higher length of ICU hospitalization. Likewise, this made it difficult to perform a definitive fixation in the first 24h, therefore DCO strategy was carried out. Without statistical significance, we observed a trend to a greater displacement of the PFF and greater comminution of the FSF in this group II. The greater complexity of fractures and the timing related to the severity of the injuries could have influenced the decision of performing definitive fixation with 2 implants.
In most series, no correlation has been identified between the time of the intervention and the development of complications, especially by analyzing AVN. However, it has been recorded a lower incidence of complications when adequate reduction and stabilization is achieved. One hypothesis is that the definitive emergent fixation of PFF could associate a higher frequency of malunion or nonunion. In our series, more complications were also observed among patients with PFF operated on first 24h, without significant difference. Prospective studies with a larger sample size will be necessary to determine if this potential difference is due to a specific type of fracture, synthesis, surgeon or timing of fixation.3
Although there is heterogeneity in the choice of implants by the surgeons in charge, there are a number of common postures. Firstly, the preferred device for the synthesis of the FSF was the reamed nail. In our center the use of non-reamed nails is anecdotal. The use of unreamed or narrow nails, open fracture and a high degree of comminution have been associated with complications such as nounion or malunion.19 Secondly, most surgeons prefer to use the double implant strategy with a SHS and additional CS for the fixation of 31B PFF, especially displaced and Pauwells type III.20 Using these management principles, and considering the heterogeneity in decision-making that has been described, the results in complications such as nonunion or malunion that have been obtained in the study are comparable to other recent series.8,9,16
Our study had several limitations, including the fact that it was retrospective in nature, with the problems inherent in this type of design. The collection of variables through the consultation of the HCE implied that some of these had not been properly registered, without having standardized scales. No clear conclusions can be drawn about the superiority of one treatment strategy over another, possibly due to the limited number of patients, wide range of injuries and the heterogeneity in management. The sample size is small to retrieve robust results and we also could not assured the validity to attribute these outcomes and complications to the use of either a single implant or a combination of implants; there are quite a few confounding variables (plating versus nailing for a shaft fracture, open versus closed fracture, level of comminution or a much larger preponderance of one type of proximal femoral fracture in one cohort compared to the other). With respect to the greatest strength of our study, is that our hospital is a tertiary referral center with an ICU specialized in polytraumatized patients. Consequently, we had a large volume of patients with all type of PFF, in contrast with the majority of studies that they only focus on the intracapsular fractures. Prospective studies with a larger sample size will be necessary to determine which is the best surgical treatment for these special fractures.
ConclusionsNo differences were found between the use of one or combined implants in ipsilateral proximal femur and shaft fractures in polytraumatized patients, neither in complications nor in time to definitive fixation. However, there was a trend to fixation with combined implants when definitive surgery was delayed. Whichever implant is chosen, a correct osteosynthesis technique is crucial.
High complication rates, even with an appropriate treatment, could be explained by the complexity of the fractures and the associated injuries. There was no difference in complications between patients undergoing surgery in the first 24h or posteriorly. Prospective studies with a larger sample size will be necessary to determine which is the best surgical treatment.
Level of evidenceLevel of evidence iv.
Authors’ contributionsAll authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Gómez Alcaraz, Jorge; Auñón Martín, Ismael; Bustamante Recuenco, Daniel and Olaya González, Carlos.
The first draft of the manuscript was written by Gómez Alcaraz, Jorge. Ajuria Fernandez, Eliam contributed to the translation of the manuscript and all authors commented on previous versions of the manuscript.
All authors read and approved the final manuscript. Capel Agundez, Aranzazu conceived the original idea and supervised the findings of this work.
Conflicts of interestThe authors report no conflict of interest. The authors have not received benefits from any source for this study.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.
Ethics Committee ApprovalResearch project approved by the Ethics Committee of Medicines of the Hospital 12 de Octubre; CEIm: No. 21/117.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data, which is been anonymized.