The aim of this study is to show the results of scaphotrapeziotrapezoid (STT) joint osteoarthritis treatment performing resurfacing arthroplasty with scaphoid anchorage.
Material and methodAn observational, descriptive and retrospective study was performed. Ten patients with isolated STT joint osteoarthritis were studied between 2013 and 2015. The mean follow-up time was 26months. Clinical results, functional and subjective scores were reviewed.
ResultsThe patients were satisfied, achieving an average of 2.1 (0–3) on the VAS score and 16 (2 to 28) in the DASH questionnaire, and returning to work in the first three months post-surgery. Recovery of range of motion compared to the contralateral wrist was 96% in extension, 95% in flexion, 87% in ulnar deviation and 91% in radial deviation. The average handgrip strength of the wrist was 95% and pinch strength was 95% compared to the contralateral side. There were no intraoperative complications or alterations in postoperative carpal alignment.
ConclusionResurfacing arthroplasty is proposed as a good and novel alternative in treating isolated SST joint arthritis. Achieving the correct balance between the strength and mobility of the wrist, without causing carpal destabilisation, is important to obtain satisfactory clinical and functional results.
El propósito de este estudio es mostrar los resultados obtenidos con el empleo de la artroplastia de recubrimiento con anclaje escafoideo en el tratamiento de la artrosis escafotrapeciotrapezoidea (ETT) aislada.
Material y métodoSe realiza un estudio observacional, descriptivo y retrospectivo del tratamiento de 10 pacientes con artrosis ETT aislada sintomática durante los años 2013 a 2015. El seguimiento medio es de 26meses (12-50). Se han evaluado los resultados clínicos, los funcionales y la satisfacción del paciente.
ResultadosLos pacientes se encuentran satisfechos, obteniendo una media de 2,1 (0-3) en la escala VAS y de 16 (2-28) en el cuestionario DASH, reincorporándose a las actividades laborales en los primeros 3meses posquirúrgicos. La recuperación del arco de movilidad en comparación con la muñeca contralateral es del 96% en extensión, del 95% en flexión, del 87% en inclinación cubital y del 91% en inclinación radial. La fuerza puño media es del 95% y la fuerza de pinza, del 95%, en comparación con el lado contralateral. No han surgido complicaciones intraoperatorias ni alteraciones en la alineación carpiana posquirúrgicas.
ConclusionesLa artroplastia de recubrimiento con anclaje escafoideo supone una alternativa novedosa y satisfactoria en el tratamiento de la artrosis ETT aislada. Lograr un balance adecuado entre la fuerza y la movilidad de la muñeca, sin producir una desestabilización carpiana, es importante para obtener resultados clínicos y funcionales satisfactorios.
Scaphotrapeziotrapezoid osteoarthritis (STT) is the second most common cause of arthritis in the wrist,1 after radioscapholunate arthritis. It can be observed in wrist X-rays in 15–29% of cases,2 but up to 83% are described in cadaver studies, associated with trapeziometacarpal arthritis.3,4 The reported prevalence of STT in cadavers, in the absence trapeziometacarpal arthritis, varies from 2% to 16% of cases.4–6 Females are most affected and it is associated with advanced age.4,7
In cadaver studies of 73 wrists with a mean age of 84 years, Bhatia et al.5 found, scaphotrapeziotrapezoid osteoarthritis in 83% of the cases, with different levels of involvement of the trapeziometacarpal joint.8 However, Brown et al.9 suggest there is poor correlation between arthritis found radiographically and that present in cadaver dissections. There is an estimated 11% prevalence of clinically symptomatic isolated STT arthritis, making this a rare disorder.2,10,11 However its real incidence is as yet unknown,1,4,5,9,12 and is believed to exceed that which is clinically apparent.5,13
The disorder was characterised and staged radiographically in 1978 by Crosby et al.4, and subsequently in 2010 by White et al.12
The initial therapeutic approach is symptomatic, by analgesic treatment, local infiltrations and the use of orthosis. Surgery is a last resort when conservative treatment has failed.
Because the role of the STT joint in the biomechanics of the wrist and thumb2 is unknown, the surgical approach to the condition poses a challenge to orthopaedic surgeons.
The complications of STT arthrodesis,14 the most widely used procedure, and resection of the distal scaphoid,7 have lead to the development of new surgical alternatives, with a view to improving the outcomes of traditional intervention, and achieve the difficult balance between eliminating pain without sacrificing strength or thumb movement, and avoid causing carpal destabilisation.
The most frequent interventions include distal scaphoid resection and tendon interposition,15 pyrocarbon implants,11,16 trapeziectomy and ligament reconstruction and tendon interposition17,18 together with partial trapezoidal resection19 and even arthroscopic procedures.20
The aim of this study was to present the clinical, radiological and functional outcomes using resurfacing arthroplasty with scaphoid anchorage, in the treatment of isolated STT arthritis.
Material and methodWe undertook an observational, longitudinal and retrospective study (level IV) from 2013 to the present date, to evaluate the results obtained in patients with isolated STT, surgically treated by STT resurfacing arthroplasty with scaphoid anchorage, between 2013 and 2015.
The inclusion criterion in selecting the study sample was the presence of clinically symptomatic STT refractory to conservative treatment, and associated trapeziometacarpal joint arthritis was the exclusion criterion.
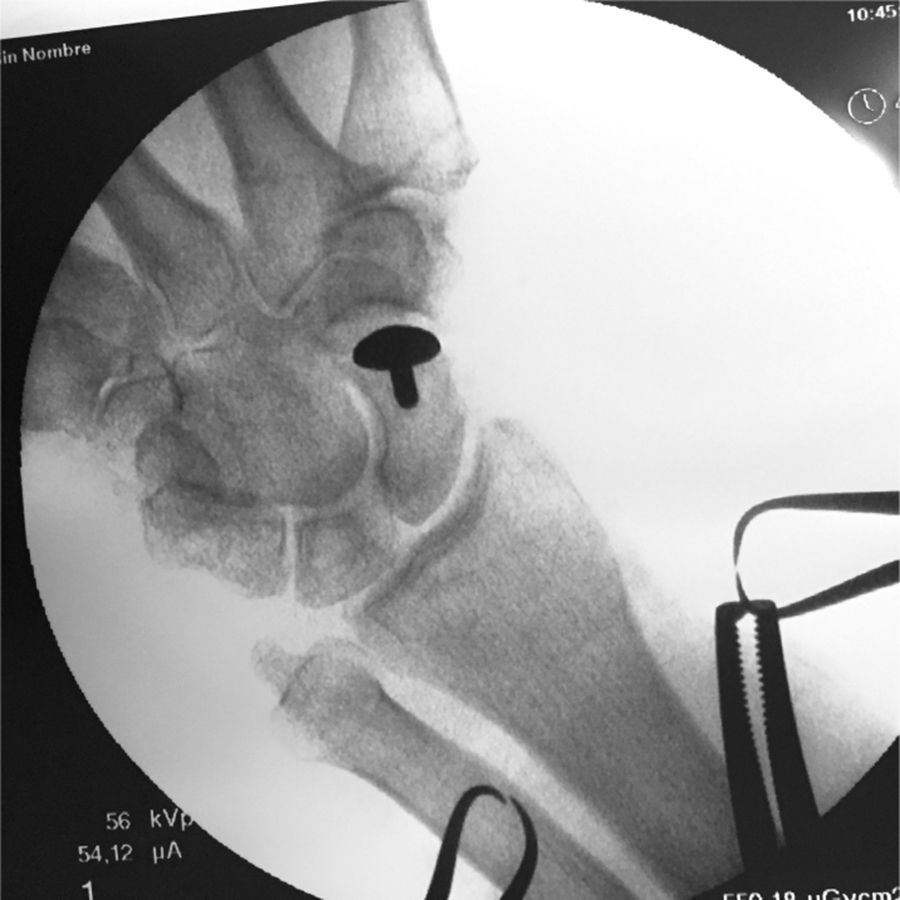
All the patients underwent a preoperative protocol and post-operative follow-up (immediate, at 3 months and once a year from placement of the implant), along with a complete clinical and radiographic study (Figs. 1–3).
Preoperative posteroanterior radiography of left wrist; scaphotrapeziotrapezoid arthritis grade III according to the classification by Crosby et al.4
Ten patients were assessed–8 women (80%) and 2 men (20%)–with isolated STT arthritis treated surgically using resurfacing arthroplasty with scaphoid anchorage (INCA), with a mean age of 65 (56–74) all right handed, of whom 7 (70%) were manual workers. The dominant side was operated in 7 (70%) of the patients.
All the patients had pain in the region of the STT, at the radio-palmar aspect of the wrist, which became worse on gripping and pinching activities, and reduced strength compared to the contralateral side.
There was no history of trauma in any case. The mean period from the onset of symptoms until surgery was 16 (6–30) months.
Seven of the 10 (70%) patients had bilateral isolated STT arthritis revealed on x-ray, which in all cases was a grade 1 according to Crosby et al.,4 and 6 out of 10 cases (60%) had carpal tunnel syndrome.
The INCA prosthesis, cobalt-chromium-molybdenum alloy and bilayer coating of pure porous titanium and hydroxyapatite, was used as the implant in all cases (Lépine, France).
All the patients were treated as outpatients by the same surgeon and the same surgical team, using loco-regional anaesthesia and ischaemia (antebrachial tourniquet) of the affected limb. All the patients received prophylactic antibiotics.
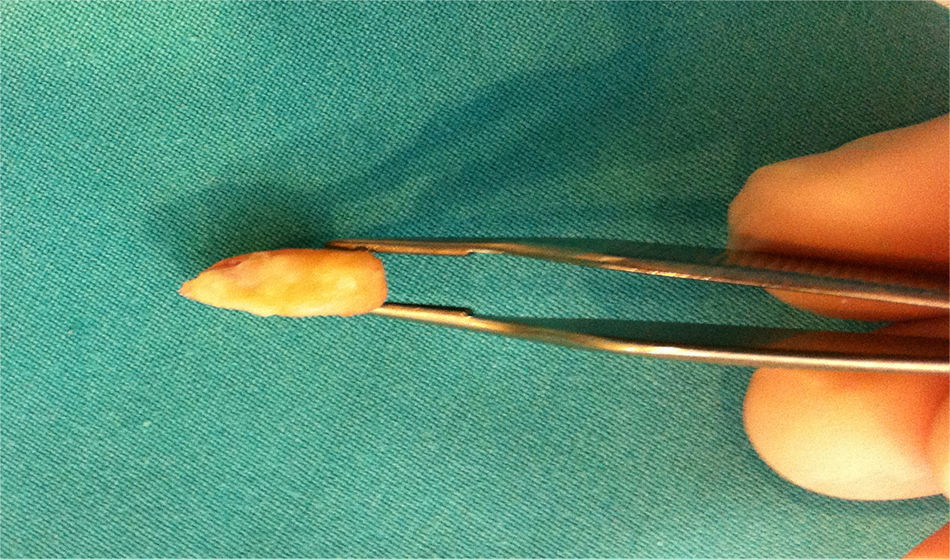
Surgical techniqueA dorsal radial approach is used with a transversal skin incision over the STT joint. The sensitive branch of the radial nerve and the radial artery are systematically located, and separated and protected. The STT joint capsule exposure is located through the interval between the tendon of the extensor carpi radialis brevis and extensor pollicus longus (ulnarly retracted) and the extensor ollicis brevis (radially retracted). The arthroplasty is performed transversally, preserving the capsular flaps for subsequent closure, and the STT joint accessed performing the osteotomy of the distal scaphoid perpendicular to its longitudinal axis, of approximately 3mm (Figs. 4 and 5), respecting the proximal insertion of the dorsal lateral scaphotrapezial ligaments and the anteromedial stout scaphotrapezial ligament.21,22
The surface of the distal scaphoid cut is considered when selecting the correct implant size, and tests of the 3 sizes available were made (14/10, 16/11, 18/12) (Fig. 6). Then, after placing the implant, its mobility and stability is checked, closure is by layers, reconstructing the joint capsule and the skin closure with resorbable suture.
All patients are immobilised by palmar plaster splint, including the wrist and the thumb column for 3 weeks, and then passive and active mobilisation is started.
The wrist's range of motion is assessed by standard goniometry, with axes centred over the third metacarpal and radial diaphysis as a reference.
Thumb mobility is measured by standard goniometry from the neutral position of the pain (10° abduction and 30° antepulsion with respect to the axis of the forearm), according to the IFSSH criteria.23 Opposition is determined using the Kapandji24 test, with values from 1 to 10 depending where the distal end of the thumb reached in maximum opposition. Comparison is made with the contralateral side.
Strength is measured in a standardised way using a Jamar Hidraulic Hand Dynamometer with the patient seated, with their arm by the side of the body, elbow flexed 90° and the forearm in neutral rotation.
We used the visual analogue scale (VAS) for clinical assessment of pain, where 0 represented no pain and 10 continual or unbearable pain, and the patients’ functional outcomes and satisfaction were measured using the DASH questionnaire.25
Radiographic analysis of the patients comprised 3 projections (anteroposterior, lateral and oblique) of both wrists, enabling the extent of STT osteoarthritis to be determined, according to the classification of Crosby et al.,4 and adequate assessment of the axes represented by the scaphoid, semilunar and large bones, which enabled us to measure the scapholunate and large semilunar angles radiographically.
The angle made by the lines forming the axis of the semilunar and scaphoid represents the scapholunate angle, for which we take values between 30° and 60° as the normality reference. The semilunar large angle is the combination of the axis of the semilunar and the large bone, assuming normality values of between 0° and 15°.26
The mean postoperative follow-up period was 26 (12–50) months.
There were no losses to follow-up.
ResultsThe INCA prosthesis was used in 10 patients. The associated carpal tunnel syndrome was operated during the same intervention in the 6 patients with the condition.
The mean surgery time was 41 (40–45) minutes, the most used implant size was 14 – up to 8 times – and a size 16 was used in the other 2 patients. There were no complications during the surgical procedure.
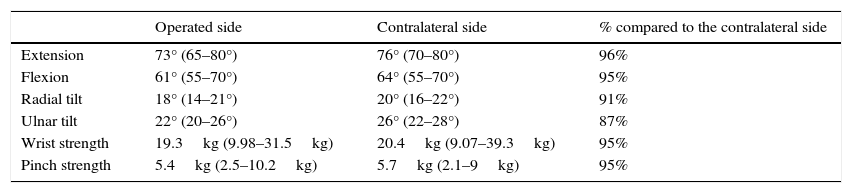
The wrist's range of motion in terms of extension was a mean of 73° (65–80°), 96% compared to the contralateral wrist; mean flexion was 61° (95%), mean ulnar tilt was 22° (87%) and radial tilt 18° (91%). In terms of thumb mobility, the mean antepulsion was 22° (20–24°), mean retropulsion 28° (21°–30°), mean abduction 31° (22°–40°) and mean adduction 21° (17–25°). Opposition according to Kapandji's24 scale was 10 in all the patients.
Grip and index finger terminolateral pinch strength evolved more gradually and progressively, with a mean grip strength of 19.3kg (95%) and the mean pinch strength was 5.4kg (95%) compared with the contralateral side (Table 1).
Sample of the results achieved in terms of mobility and strength, for the operated side, the contralateral side and their comparison expressed as a percentage.
| Operated side | Contralateral side | % compared to the contralateral side | |
|---|---|---|---|
| Extension | 73° (65–80°) | 76° (70–80°) | 96% |
| Flexion | 61° (55–70°) | 64° (55–70°) | 95% |
| Radial tilt | 18° (14–21°) | 20° (16–22°) | 91% |
| Ulnar tilt | 22° (20–26°) | 26° (22–28°) | 87% |
| Wrist strength | 19.3kg (9.98–31.5kg) | 20.4kg (9.07–39.3kg) | 95% |
| Pinch strength | 5.4kg (2.5–10.2kg) | 5.7kg (2.1–9kg) | 95% |
The placement of the implant in the distal scaphoid, by increasing its height, caused a change in carpal alignment. Radiographic measurement showed mean scapholunate angle values of 52° (33°–65°), the mean postoperative angle being 31°(14°–52°). The mean preoperative semilunar-large angle was 8° (4°–13°), the mean postoperative angle being 10° (4°–14°).
All the patients returned to their daily activities in the first 3 months after the operation. Likewise all the patients had improved subjective assessment of pain score (VAS), with a preoperative mean of 8.1 (7–9) and a postoperative mean of 2.1 (0–3). Functional assessment using the DASH questionnaire showed a postoperative mean of 16 (2–28), and all the patients were satisfied with the surgical intervention.
Temporary irritation of the sensitive branch of the radial nerve was a postoperative complication. This occurred in 2 of the 10 patients operated (20%) and the symptoms completely resolved within the first 6 postoperative weeks. There were no dislocations, osteolytic changes or loosening of the implant.
DiscussionUncertainty remains as to the participation of the STT joint in arthritis and the biomechanics of the wrist and thumb joint.2 The difficulty of clinically identifying the condition and its low incidence, together with therapeutic outcomes that do not achieve adequate balance in terms of strength, mobility and progression of the disorder, keep the debate about the different forms of treatment open.27
The use of scaphoid anchorage implants is a novel form of treatment for isolated STT arthritis. The references in the literature to this form of treatment are few but satisfactory. An example of this is the results presented by Teissier and Daumillare28 on a total of 15 patients, with a mean follow-up of 39 months in 2015.
The results of our study show that after 26 months’ mean follow-up the patients experienced major clinical and functional improvement, and were able to resume their working and daily activities promptly – within the first 3 months.
The epidemiological results of the study are similar to those found in the literature, the condition being more frequent in females, and predominating in the sixth decade of life.
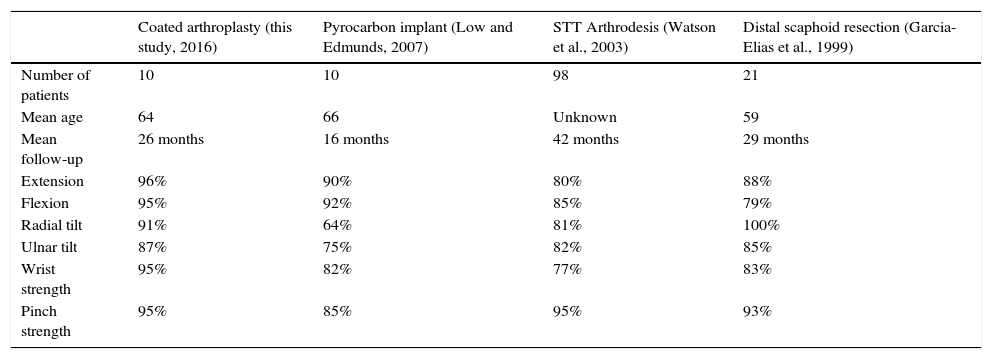
Recovery of range of motion was the first variable to show improvement, a recovery of motion above 90% was achieved, with the exception of ulnar tilt, with 87% recovery, still higher than that found in other studies (75% with the pyrocarbon implant: Low and Edmunds11; 82% with STT arthrodesis: Watson et al.29; 85% with distal scaphoid resection: Garcia-Elias et al.7 (see Table 2, modified from Low and Edmunds).
Comparison between four studies showing different treatment forms for scaphotrapeziotrapezoid, modified from Low and Edmunds.11
| Coated arthroplasty (this study, 2016) | Pyrocarbon implant (Low and Edmunds, 2007) | STT Arthrodesis (Watson et al., 2003) | Distal scaphoid resection (Garcia-Elias et al., 1999) | |
|---|---|---|---|---|
| Number of patients | 10 | 10 | 98 | 21 |
| Mean age | 64 | 66 | Unknown | 59 |
| Mean follow-up | 26 months | 16 months | 42 months | 29 months |
| Extension | 96% | 90% | 80% | 88% |
| Flexion | 95% | 92% | 85% | 79% |
| Radial tilt | 91% | 64% | 81% | 100% |
| Ulnar tilt | 87% | 75% | 82% | 85% |
| Wrist strength | 95% | 82% | 77% | 83% |
| Pinch strength | 95% | 85% | 95% | 93% |
Recovery of strength, achieving values of up to 95% for grip strength and 95% for grip strength, was the last parameter to recover, and occasionally exceeded the strength of the contralateral hand. The strength values obtained are satisfactory and comparable to those obtained with other forms of treatment (see Table 2, modified from Low and Edmunds), with the exception of presented by Langenhan et al.,18 where recovery of strength by trapeziectomy, ligament reconstruction and tendon interposition achieved recovery of grip and pinch strength of up to 100% compared to the other side.
Scaphoid fixation of the implant, together with the integration achieved thanks to the hydroxyapatite coating, provide stability to the implant. This fact is essential to maintain joint congruence and firmness over the radial column, preserving mobility at mediocarpal level. Thus, the complication of prosthetic dislocation, which occurs in interposition arthroplasty without scaphoid anchorage, as described with the use of pyrocarbon implants.11,16 However, we do not rule out the onset of other complications subsidiary to the implant used in our study, which have not occurred to date, but long-term follow-up must be continued.
Correct placement of the implant at scaphoid level, despite being more technically easy than other procedures, is a factor that can change patients’ clinical and functional outcomes. It is important to regain scaphoid length and make a correct choice of implant size without causing pinching between the prosthesis and the proximal trapezio-trapezoid joint.
Interposition arthroplasty15 has been used to prevent progression and carpal destabilisation caused by resection of the distal scaphoid,7 its arthroscopic excision20 and even procedures where osteotomy is not performed at the level of the scaphoid, such as trapeziectomy and ligament reconstruction and tendon interposition,17,18 or its association with partial trapeziectomy,19 with satisfactory outcomes. Its use does not prevent progression of the deformity to DISI, as Rectenwald et al.30 (in two cases) after a trapezoidectomy of almost 50%, for pantrapezial arthritis. When Andrachuk and Yang,19 excised a third of the proximal trapezoid without causing carpal destabilisation. Even in cases of trapeziectomy for trapeziometacarpal arthritis the deformity progresses to DISI, especially in patients with STT arthritis.31 STT arthritis sometimes presents associated with a pattern of DISI. It is not known whether this is caused by STT arthritis or whether instability causes the STT arthritis. In this situation, the risk of radiographic progression of instability is greater, therefore sufficient graft should be put into the scaphoid to ensure its length is maintained when an arthroplasty is used, and carpal destabilisation should be anticipated and prevented, when resection techniques, scaphoid arthoplasty and trapeziectomies are performed, and additional carpal stabilisation procedures should be considered.19,32,33
The principal advantage of this implant lies in restoring the original carpal kinematics and preventing the progression of poor alignment to DISI, which could be caused by maintenance of the height of the scaphoid by the implant. At the current time of follow-up no radiographic or clinical signs of progression to carpal collapse have been encountered. However, studies with more patients and a longer follow-up period are necessary to identify and prevent this problem.
Among the complications that appeared during follow-up was the onset of paraesthesia in the territory of the sensitive branch of the radial nerve in 2 patients, in one case functional recovery started insidiously, and complete resolution of symptoms occurred within the first 6 postoperative weeks.
The satisfactory results achieved in the study show that INCA prostheses are a good alternative for treating isolated and symptomatic arthritis.
This study seeks to show the results achieved with a novel technique in treating a disorder that is difficult to treat.
The study had limitations in terms of its methodological characteristics. Comparison with the contralateral wrist, where we found an incidence of STT arthritis of the lowest Crosby grade, in up to 70% of cases, and the lack of references on coated arthroplasties in this disorder mean it is necessary to compare results with different forms of treatment.
More prospective and randomised research studies are considered necessary, and comparison with different forms of treatment. Further studies should include a larger number of patients with a longer follow-up period.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that neither human nor animal testing have been carried out under this research.
Data confidentialityThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Privacy rights and informed consentThe authors declare that no patients’ data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Humada Álvarez G, Simón Pérez C, García Medrano B, Faour Martín O, Marcos Rodríguez JJ, Vega Castrillo A, et al. Tratamiento de la artrosis escafotrapeciotrapezoidea aislada con artroplastia de recubrimiento con anclaje escafoideo. Rev Esp Cir Ortop Traumatol. 2017;61:412–418.