Rotational ankle fractures are common, have diverse personalities and affect both robust and fragile patients. Postoperative complications are frequent, creating a sizeable economic burden. The primary purpose of this study was to expand current knowledge on predictors of postoperative complications after low-energy ankle fracture fixation.
Materials and methodsA retrospective single-center cohort study was completed of patients undergoing internal fixation OF low-energy ankle fractures. The primary outcome was first-year postoperative complications, classified as major (surgical) or minor (non-surgical). Data on patients, their injuries, and treatments were collected. To identify potential predictors of outcomes, logistic regression methods were used, with a backward-stepwise method used for model fitting.
ResultsIn total, 663 patients of median age 59 years were analyzed. We found a high rate of complications (28.4%), with wound-healing issues and infections predominant. Overall, 14.8% had minor complications, while 13.6% required an unplanned reoperation. On multivariable analysis, the most consistent predictors of complications were older age (OR=1.02 per year), longer operating time (3.32 per hour), and smoking (2.91).
ConclusionsOlder patients and smokers who sustain fractures requiring more complex surgery are at higher risk of postoperative complications.
Las fracturas rotacionales del tobillo son frecuentes, tienen personalidades diversas y afectan tanto a pacientes robustos como a frágiles. Las complicaciones postoperatorias son frecuentes y generan una considerable carga económica. El objetivo principal de este estudio es ampliar los conocimientos actuales sobre los factores predictores de las complicaciones postoperatorias tras la fijación de fracturas de baja energía del tobillo.
Materiales y métodosEstudio de cohortes retrospectivo en un único centro sobre pacientes sometidos a fijación interna por fracturas de baja energía del tobillo. El resultado primario fueron las complicaciones postoperatorias durante el primer año, clasificadas como mayores (quirúrgicas) o menores (no quirúrgicas). Se recopilaron datos sobre pacientes, lesiones y tratamientos. Para identificar posibles factores predictores de los resultados se utilizaron métodos de regresión logística, con un ajuste del modelo por pasos hacia atrás.
ResultadosEn total, se analizaron 663 pacientes con una mediana de edad de 59años. Se observó una elevada tasa de complicaciones (28,4%), predominando los problemas de cicatrización y las infecciones. En general, el 14,8% tuvieron complicaciones menores, mientras que el 13,6% requirieron una reintervención no planificada. En el análisis multivariable, los predictores más consistentes de complicaciones fueron la edad avanzada (OR=1,02 por año), un tiempo quirúrgico prolongado (3,32 por hora) y el tabaquismo (2,91).
ConclusionesLos pacientes de edad más avanzada y los fumadores que sufren fracturas que requieren intervenciones quirúrgicas más complejas tienen un mayor riesgo de complicaciones postoperatorias.
Low-energy ankle fractures are very frequent, accounting for approximately 10% of all fractures. Their incidence has been reported as from 71 to 184 cases per 100,000 inhabitants per year,1,2 making them the second leading cause of orthopedic hospitalization and surgery after hip fractures and the first in people under 60 years old.3 Therefore, both direct and indirect associated economic burdens are high, especially when dealing with complex injuries or complications.4
Rates of complications reported after ankle fracture surgery range from 1% to 36%.5–24 Old age and diabetes are commonly-identified predictors of adverse events.8,9,15,16 Knowledge of modifiable risk factors is of foremost importance, since it could guide the updating of healthcare protocols, thereby reducing postoperative morbidity and financial costs.
The primary goal of this study was to identify which factors influence the need for unplanned reoperations during the first postoperative year after internal fixation of a low-energy ankle fracture. Secondarily, we investigated non-surgical complications and the combination of both surgical and non-surgical issues. We hypothesized that patients experiencing greater deterioration in their baseline conditions, more severe fractures, and requiring more extensive treatment would present a higher risk of complications.
Materials and methodsThis retrospective cohort study (level of evidence IV) was approved by our institutional review board (reference number PR(ATR)397/2017) and this paper written guided by the STROBE statement. All patients were operated on consecutively at a single public and university level I trauma center from November 2009 to April 2019. Seventy-four surgeons and training surgeons with variable dedication to orthopedic trauma participated in the fixation procedures. We included all skeletally mature patients (age≥15 years old) undergoing surgical fixation of a low-energy rotational ankle fracture (AO/OTA segment 44). Patients with trimalleolar fixation, records of previous ankle surgery, infections or malignant conditions around the ankle, bilateral fractures, fractures occurring in a multiple-trauma scenario (Injury Severity Score≥16) were excluded. Postoperative follow-up was for one year.
Postoperative complications were defined as any record of a local postoperative complication, including dehiscence or skin breakdown, infection, and mechanical failure, during the first postoperative year. Complications were subsequently categorized as either major or minor. Major complications required an unscheduled reoperation and were our primary outcome of interest; elective procedures, like syndesmotic screw removal, were excluded. Minor complications did not require further unplanned reinterventions. Non-surgical and surgical first-year local postoperative complications were then coalesced into “any local complication”.
We collected independent variables on patients’ baseline characteristics, injuries, and treatments; all summarized in Table 1. Given that we only encountered 14 cases with trimalleolar fixation, we incorporated them into the bimalleolar cases for analysis. We decided, a priori, to test a modest number of predictors whose validity was already supported by previously published literature.
Depiction of predictors and descriptive statistics.
| Predictors | Resultsa |
|---|---|
| Age: age in years at the day of admission for fracture treatment | 59 (45–72) |
| Diabetes: oral antihyperglycemics agents, insulin intake or target organ damage | 95 (14.33) |
| Smoking: records of tobacco abuse or ongoing cessation treatment | 115 (17.4) |
| Open fracture: wound in relation to any fracture foci | 26 (3.9) |
| Fracture-dislocation: significant joint ankle incongruity at the time of the fracture requiring reduction maneuvers during initial management | 154 (23.2) |
| Preoperative skin breakdown: severe contusion or abrasion, blisters, or necrosis | 146 (22.0) |
| Time from admission to surgery: days taken from admission to surgical fixation | 5 (2–8) |
| Surgical time (hours): time to complete the surgical procedure | 1.5 (1.2–1.8) |
| Fracture fixationb | |
| Unimalleolar: either fibula or tibia is fixed | 308 (46.5) |
| Bi- and trimalleolar: both fibula and tibia are fixed | 355 (53.5) |
Radiographs for each case were assessed using RAIM Viewer software (Corporació Sanitària Parc Taulí, Spain). Medical records were obtained from the institutional healthcare SAP database (SAP SE, Germany), which contains all clinically relevant information. Images and medical records were evaluated once by one of three designated researchers, who were both training orthopedic surgeons and the coauthors of this paper. Data were collected on paper-based case report forms and entered into a Microsoft Excel database. Input validation rules were applied, and the database was subjected to a depuration process by two independent investigators. All cases with missing data for any of the study variables were eliminated from final analysis. To check randomness in data loss, a runs test was performed on the age of excluded subjects.
To maximize statistical power, all patients who met the eligibility criteria were included. We found 90 patients with the main adverse outcome. This allowed us, following standard practices, to create regression models with up to nine variables (one independent variable per 10 cases). Likewise, we sought a minimum sample size of 550, defined by the formula described by Bujang.25 Stata 14.2 (StataCorp, USA) was used for analysis. Descriptive analysis of the overall sample was performed, with categorical variables summarized as counts and percentages, while continuous variables were summarized as medians and interquartile ranges (IQR) due to the non-normality of distributions. To improve precision, no categorization of continuous variables was implemented. Odds ratios (OR), their 95% confidence interval (95% CI), and associated p values were calculated by multivariable logistic regression to measure the association between risk factors and the three binary outcomes (major, minor, and any complications). For independent variable selection, a backward stepwise selection technique was used. Since we used just a modest number of predictors, we did not consider bivariate analysis necessary for model selection. To initiate multivariable analysis, a model containing all the independent variables was generated. At each step, the variable with the largest p value was removed until all p values were ≤0.20. We detected a close-to-significance interaction (p=0.06) between operating time and delay of surgery that was controlled for in the final model. We ruled out all other interactions and confounders using chunk tests. Since inadequate statistical power existed for subgroup analysis of major complications, only bivariate analyses were performed, and these results should be interpreted with caution. Any two-tailed p value ≤0.05 was considered statistically significant.
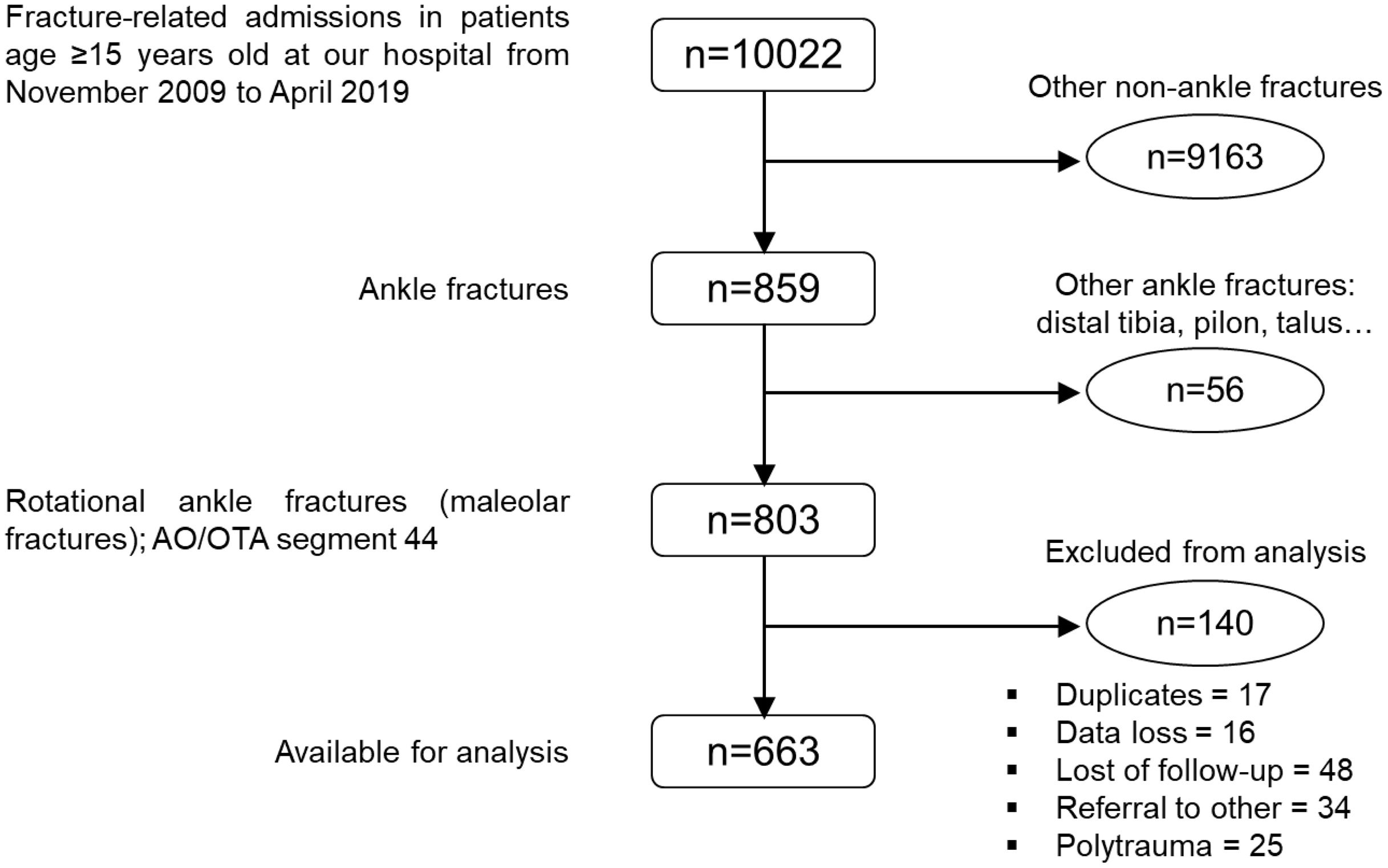
ResultsA total of 803 potential participants were identified. Among these 803, 17 were removed as duplicates; data were missing on 16 patients; and 48 were lost to follow-up. Since the ages of the lost cases were completely random (p=0.71), we did not consider this a source of bias. In addition, 34 patients were referred to other healthcare centers, mainly because of motor vehicle accidents or sports injuries, while a further 25 polytrauma cases were excluded. This may have slightly biased our sample, since these injuries tend to be associated with younger age. This left 663 patients of median age 59 years (IQR=27) available for final analysis (Fig. 1). Descriptive statistics for each independent variable are summarized in Table 1.
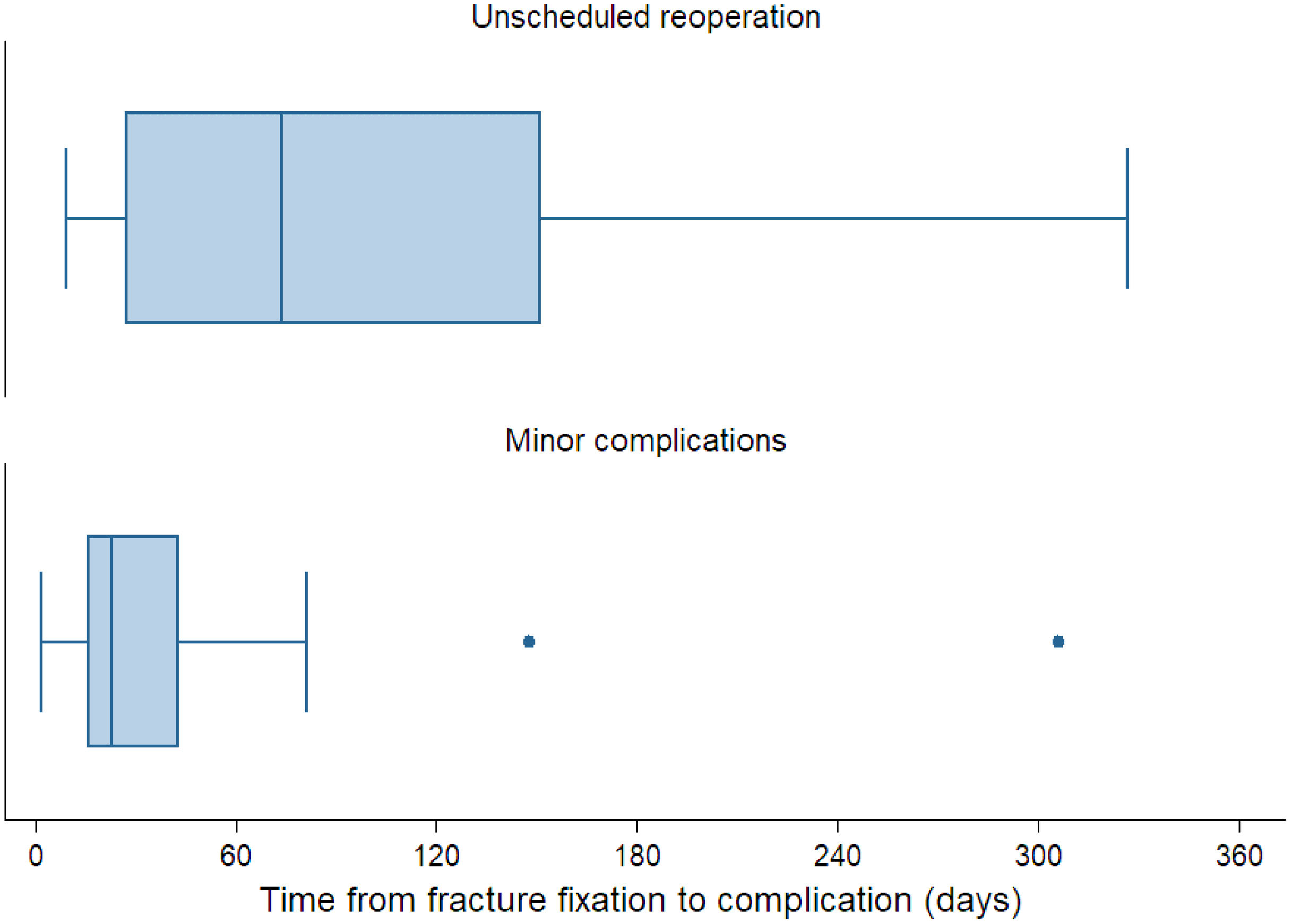
Among the 663 patients, 90 (13.6%) required an unplanned surgical intervention during the first postoperative year and were, thus, considered to have had a major complication. Sixty-two patients needing reintervention (9.4%) had impaired wound healing and infections. After debridement, primary wound closure was possible in 42 of these 62 cases (6.3%), while soft-tissue reconstruction by plastic surgeons was needed for 20 (22.2%). All patients undergoing debridement had their implants removed, excluding four among whom primary closure was achieved. The implants were removed to enable primary closure and eliminate the infection. At that time, fractures were deemed adequately healed, occurring at a median of 117 days after fixation (IQR=152). Cases necessitating soft tissue reconstruction underwent reintervention earlier, at a median of 33 days (IQR=35). Twenty-eight patients (4.2%) had mechanical failure requiring the revision of fixation. Among these 28, 19 cases (2.9%) of mechanical failure were related to incorrect treatment of syndesmotic instability, while nine (1.4%) involved total failure or non-union requiring complete revision of the fixation. Ninety-eight patients (14.8%) developed minor (non-surgical) complications. All minor complications entailed wound-healing issues that resolved with adequate wound care with or without antibiotics. Overall, 28.4% of the patients (n=188) developed some form of local complication, most of them within the first six postoperative months (Fig. 2).
Box plots showing the time from fracture fixation until the diagnosis of major and minor complications. Most reinterventions took place during the first six postoperative months. In the case of minor complications, the vast majority occurred during the first three postoperative months.
Diabetes was not common enough to be a statistically significant predictor in any of the fitted multivariate models, though we did find a greater percentage of diabetic patients in those patients who required reoperation (20.0 vs. 13.4%) or had complications overall (16.5 vs. 13.5%) (Table 2). Older age, smoking, and longer operating time were the most consistent predictors, remaining as predictors of all three outcomes investigated (major, minor, and any complications).
Comparative descriptive statistics.
| Predictors | Unscheduled reoperation | Minor complication | Any complication | |||
|---|---|---|---|---|---|---|
| Yes=90 (13.6%) | No=573 (86.4%) | Yes=98 (14.8%) | No=565 (85.2%) | Yes=188 (28.4%) | No=475 (71.6%) | |
| Age (in years) | 62 (51–77) | 58 (43–72) | 63.5 (52–73) | 57 (43–72) | 63 (51.5–73) | 55 (42–71) |
| Diabetes | 18 (20.0%) | 77 (13.4%) | 13 (13.3%) | 82 (14.5%) | 31 (16.5%) | 64 (13.5%) |
| Smoking | 20 (22.2%) | 95 (16.6%) | 24 (24.5%) | 91 (16.1%) | 44 (23.4%) | 71 (14.9%) |
| Alcoholism | 8 (8.9%) | 26 (4.5%) | 7 (7.1%) | 27 (4.8%) | 15 (8.0%) | 19 (4.0%) |
| Open fracture | 13 (14.4%) | 13 (2.3%) | 3 (3.1%) | 23 (4.1%) | 16 (8.5%) | 10 (2.1%) |
| Fracture-dislocation | 45 (50.0%) | 109 (19.0%) | 33 (33.7%) | 121 (21.4%) | 78 (41.5%) | 76 (16%) |
| Preoperative skin breakdown | 37 (41.1%) | 109 (19.0%) | 35 (35.7%) | 111 (19.6%) | 72 (38.3%) | 74 (15.6%) |
| Time from admission to surgery | 6 (3– 4) | 4 (2–8) | 6 (3–11) | 4 (2–8) | 6 (3–12) | 4 (2–7) |
| Operating time (hours) | 1.7 (1.5–2.2) | 1.4 (1.2–1.8) | 1.7 (1.4–2.0) | 1.5 (1.2–1.8) | 1.7 (1.4–2.0) | 1.4 (1.2–1.7) |
| Fracture fixation | ||||||
| Unimalleolar | 22 (24.4%) | 286 (49.9%) | 24 (24.5%) | 284 (50.3%) | 46 (24.5%) | 262 (55.2%) |
| Bi- and trimalleolar | 68 (75.6%) | 287 (50.1%) | 74 (75.5%) | 281 (49.7%) | 142 (75.5%) | 213 (44.8%) |
Categorical variables as: count (percentage).
Continuous variables as: median (interquartile range).
Risk of a first-year reoperation increased with increasing patient age in years (OR=1.02 per year), smoking (2.54), an open fracture (3.56), fracture-dislocation (2.31), preoperative skin breakdown (1.62), delay of internal fixation in days (1.12 per day) and operating time in hours (3.97 per hour). For minor complications, age (1.01), smoking (2.28), operating time (1.92) and bimalleolar fracture fixation (2.25) remained as significant predictors. We found significant relationships between the global complications’ outcome and seven of the nine independent variables we studied: age (1.02), smoking (2.91), fracture-dislocation (2.03), skin breakdown (1.96), delay in surgery (1.10), operating time (3.32) and bimalleolar fixation (1.97). Figs. 3 and 4 are predictive marginal effect plots for the probability of any local complication by patient age and operating time, respectively. Complete multivariate analysis results are summarized in Table 3.
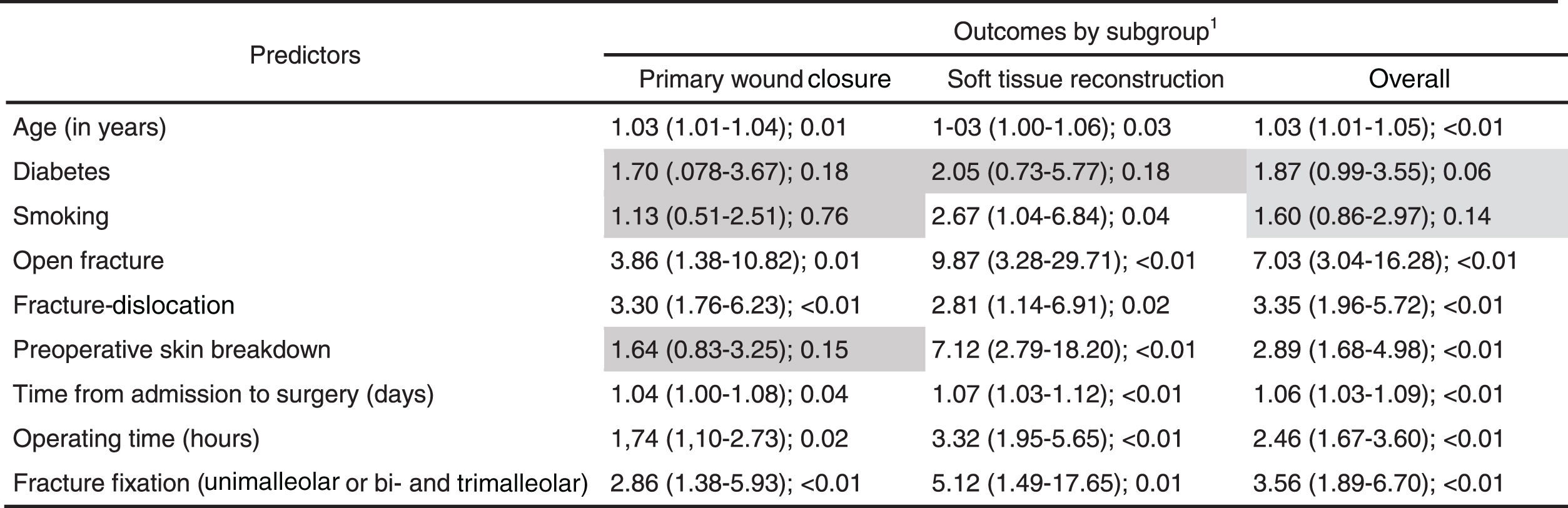
Paradoxically, on bivariate analysis for specific major complications, only diabetes and smoking were not associated with a significant increase in the risk of infection. The presence of an open fracture focus was revealed as the most powerful predictor of the need for surgical debridement (OR=7.03), followed by bimalleolar fixation (3.56) and the presence of joint dislocation (3.35) (Table 4). Regarding mechanical complications, the most consistent predictor for the need for revision of fixation was the presence of fracture-dislocation (OR=4.80) (Table 5). We insist on the need for readers to interpret the results of our bivariate analysis with caution.
Results of bivariate analysis (logistic regression) on major complications related to mechanical failure.
1Results of logistic regression shown as: OR (95% CI); p value. Gray background for cells containing non-significant results.
2No failure of fixation or nonunion were recorded in open fractures. It was not possible to test this relationship, so this cell has been left empty.
In our sample of 663 patients with ankle fractures, predominantly comprising mature patients, we observed complications in 188 cases, accounting for 28.4%. Of these 28.4%, almost half (13.6% of the total sample) required reoperation for management, while 14.8% of the sample had non-surgical complications. The three baseline factors that predicted both major and minor adverse events, and adverse events overall, were older patient age, longer operating time, and a history of smoking.
Though considerable disparity in reporting methods in the available literature makes it difficult for us to compare our results against those previously published,26 our incidence of postoperative complications was higher than most. The reported intermediate-term rate of unscheduled reoperation ranges from 1.0 to 10.8%.5,11,13,15–21,23,27,28 Unplanned reoperations related to wound healing problems and infections are performed in 9.4% of patients. Infections are associated with greater comorbidity and fracture severity.17,29–31 Reoperations due to mechanical problems are performed in 4.2% of patients, a rate that increases with increasing severity and instability of the initial injury.6,28,29,32 The main indication for revised fixation is inadequate treatment of a syndesmotic injury, followed by mal-reduction and articular penetration of implants.28,30–33 Rates for minor complications have been reported to range from 1.0 to 12.9%,9,10,13,17,20,22,34 most of them superficial infections. Non-surgical wound-healing issues are associated with greater consumption of healthcare resources, as they require closer monitoring by healthcare personnel and involve a higher frequency of visits to emergency services and readmissions.10,15,21
Older age is a well-established predictor of postoperative complications.5,7–10,14,27,30 Poor bone quality and impaired tissue repair increase the risks of dehiscence, infection, and mechanical problems. Older patients also tend to present with more co-morbid diseases and score worse on comorbidity indexes, both of which are also associated with an increased risk of complications.9,10,12,14,19,20,22–24 Despite all this, surgical treatment of ankle fractures in the elderly is considered reproducible, offering acceptable complication rates and even improved survival rates.8,9,23,30 Reported mean patient ages for such fractures range from 43 to 55 years.5,10–16,27,29 Our sample had a somewhat older median age of 59 years. We attribute at least some of the excess morbidity we observed to the older age of our patients and our broad definition of outcomes.
Longer operating time is also a well-documented risk factor for postoperative complications.11,14 In our series, the surgical procedures of patients who developed complications averaged being 17.6% longer. This relationship can be attributed to longer tourniquet use and surgical exposure, but also to greater complexity of the initial injury or the performance of a less-experienced surgical team. Delay in surgical treatment has also been documented as a predictor of postoperative complications.14 This may be related to organization issues, but also to greater injury severity and soft tissue damage around the fracture.
Preoperative skin breakdown has been inconsistently reported as a risk factor for complications. It is always advisable to wait for the resolution of any edema and the healing of any skin lesion before proceeding with fracture fixation.9,11,30 This said, the optimum timing of surgery remains an issue of debate. Before the procedure, patients’ suitability for surgery needs to be assessed regularly and procedures scheduled with utmost care. During surgery, the rapid achievement of therapeutic goals is mandatory. Regarding surgical technique, patients requiring bimalleolar fixation generally experience complications more frequently than those requiring unimalleolar fixation, especially on the medial side. Fracture mechanisms involving external rotation or abduction, which are the most common, cause valgus deformities and the proximal fragment of the medial focus to impinge on the soft tissue coverage, which is more precarious in this area. Consequently, the skin is torn from the inside out, causing an open fracture, or it is severely bruised, which predisposes patients to healing problems and infection.5,10,24
Smoking is associated with an increased risk of dehiscence, infection, delayed union, and worse functional outcomes.9,11,17,35 In our study, smoking almost tripled the risk of local complications. In general terms, smoking is linked to a poor prognosis, an increased risk of fracture, and greater consumption of healthcare resources. It also synergistically increases the effect of other risk factors, like older age and diabetes.17,35 Diabetes mellitus is one of the main predictors of poor postoperative prognosis after ankle fracture fixation.5,7,9,10,12,13,15,16 However, in our study, we were unable to identify a statistically-significant association between diabetes and the outcomes we investigated, likely due to the small number of patients with diabetes.
Some of the strongest predictors of complications we identified were related to fracture severity. The odds ratio (OR) for surgical complications was 3.56 for open fractures and 2.31 for fracture-dislocations on multivariable analysis. We found 3.9% of the fractures overall to be open in our study; but this incidence was 14.4% among patients needing reoperation. In the literature, from 5.8 to 9.8% of ankle fractures are open.6,7,14,16,28 Open fractures are clearly associated with increased risks of both complications and reoperation.7,12–14,17,20,21,27,30 The impaired skin trophism related to aging and chronic diseases predisposes patients to open lesions.
There is a logical association between joint dislocations and open fractures, which cause an inside-out break in the skin.13,32,36 Ankle fracture-dislocations have been reported to have an incidence from 5.8 to 32.4%.6,36 In our sample, this was the case for 23.2% of all patients and 50% of those who required reoperation. Concomitant joint dislocation increases the risk of complications, including reoperation and impaired ankle function.6,27,30,32,36 Worse outcomes are linked to a higher incidence of ligamentous and soft tissue injuries, a more technically-demanding anatomical reduction, and osteochondral injuries.29,32,36
Our study has several limitations that include its retrospective nature, single-center recruitment, absence of randomization, and no assessment of inter-observer reliability for radiological evaluations. The asymmetrical composition of the sample, in terms of patient age, also may limit the generalizability of our results. We did not gather data on the training level or specialization in ankle fractures of the treating surgeons, nor did we collect accurate information on surgical approaches, specific implants used, or adequately characterize diabetes (including insulin usage or target organ involvement) or grading of open fractures. These factors could have potentially influenced our results. We also did not track the progression of complications over the 10-year recruitment period. However, the number of predictors was limited to ensure the statistical power of the study and the number of outcomes evaluated is limited due to the challenge of retrospectively obtaining reliable clinical data. Strengths of this study include its large sample size and evaluation of previously documented risk factors.
ConclusionsWe experienced high rates of both major and minor complications and found their most consistent predictors to be patient age, operating time, and smoking. Since low-energy ankle fractures are very common and associated with substantial economic burdens, future research needs to expand our knowledge of these predictors.
Level of evidenceLevel of evidence iii.
Authors’ contributionsAll authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by JVAP, OPA, SCA, MAC and MMRV. The first draft of the manuscript was written by JVAP, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethical approvalThis study was approved by our institutional review board (reference number PR(ATR)397/2017).
Consent to participate and publishThis is a retrospective study. Its realization did not imply any risk for the participants and all the collected data were de-identified. Therefore, IRB approved a full waiver of informed consent.
Availability of data and materialsThe data that support the findings of this study are available from the corresponding author, JVAP, upon reasonable request.
FundingNo funding was received for conducting this study.
Conflict of interestsThe authors have financial conflicts of interest to declare with Smith & Nephew, Zimmer-Biomet, Stryker and MBA Surgical Empowerment.