To determine the impact of each cause of revision surgery in total hip arthroplasty during the period 2009–2013. To analyse the relationship between these causes with different variables.
Materials and methodsA study was conducted on 127 patients who had hip replacement revision surgery in our hospital during this period. Parameters, such as age, sex, date of primary arthroplasty, prosthetic replacement date, and main cause of the revision were recorded. Those revisions performed within 5 years after the primary arthroplasty were considered as early rescue.
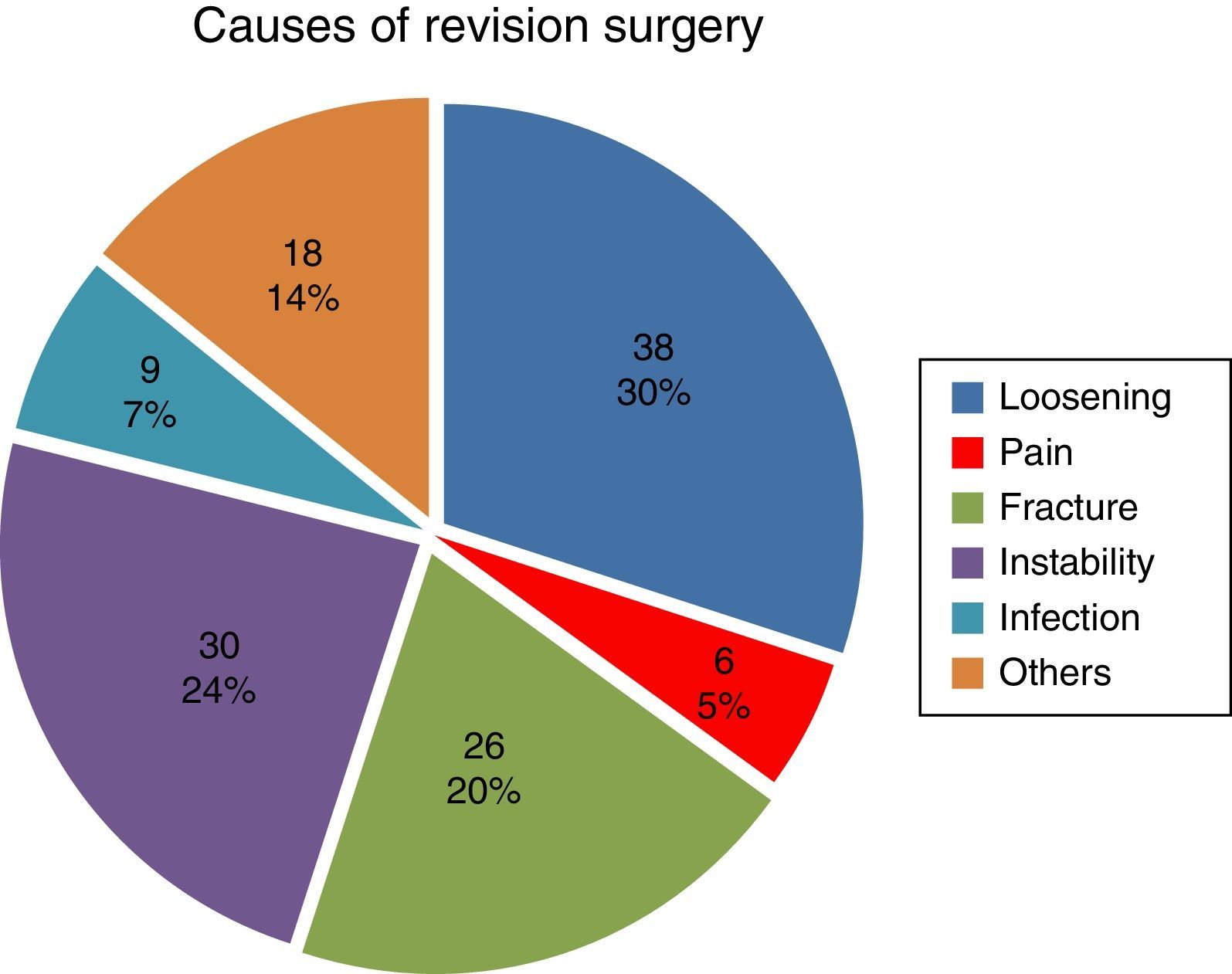
ResultsThe most common cause of rescue was aseptic loosening in 38 (30%) followed by instability in 30 (24%).
In terms of age at the time of rescue, statistically significant differences were found, with it being significantly higher in patients re-operated for a fracture.
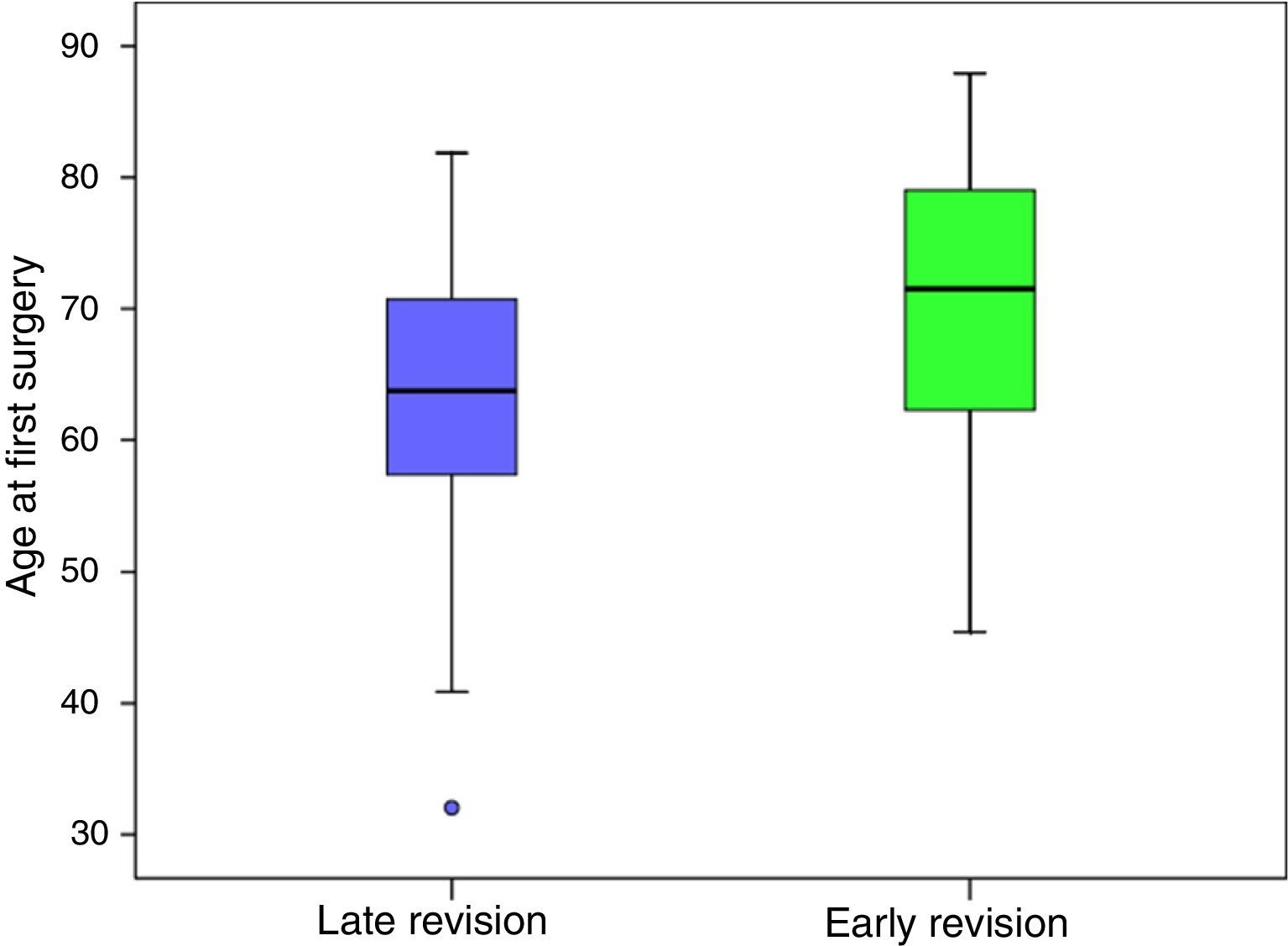
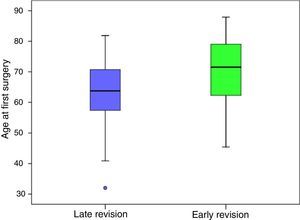
Differences in age at first surgery were found to be 7 years younger than those with late rescue (63.40) with respect to early (70.21).
DiscussionSimilar results to ours have been observed in other published series, except for the higher incidence of instability in early rescue.
ConclusionsThis study demonstrates aseptic loosening and instability as the most frequent causes of revision surgery in our hospital. Age is a very influential factor in relation to longevity of primary arthroplasty. Complications were higher in when the primary hip replacement is implanted in older patients.
Se pretende evaluar la incidencia de cada una de las causas de cirugía de revisión de artroplastia total de cadera en el periodo comprendido entre 2009 y 2013 con relación a diferentes variables.
Material y métodosHemos analizado 127 cirugías de revisión de artroplastia total de cadera realizadas en 127 pacientes en nuestro centro durante dicho periodo. Se registraron parámetros como edad, sexo, fecha de artroplastia primaria, fecha de reemplazo de prótesis y causa principal de reintervención. Se consideraron rescate precoz aquellas reintervenciones realizadas antes de los 5 años tras la artroplastia primaria.
ResultadosLa causa de rescate más frecuente fue el aflojamiento 38 (30%) seguido de inestabilidad 30 (24%).
En cuanto a la edad en el momento del rescate, se encontraron diferencias estadísticamente significativas: los pacientes con reintervención por fractura eran significativamente mayores.
Se encontraron diferencias en cuanto a la edad en la primera cirugía: eran 7 años más jóvenes aquellos con rescates tardíos (63,40) con respecto a los precoces (70,21).
DiscusiónHemos observado resultados similares a los de las demás series publicadas, excepto una mayor incidencia de inestabilidad en rescate precoz.
ConclusionesEste estudio demuestra el aflojamiento aséptico y la inestabilidad como causas más frecuentes de rescate en nuestro centro. La edad es un factor muy influyente en cuanto a la longevidad de la artroplastia primaria. Son mayores las complicaciones en pacientes en los cuales se implanta la artroplastia primaria de cadera a edad más avanzada.
Hip replacement revision surgery is a habitual procedure in our centre. It is becoming increasingly frequent due to the higher number of primary prostheses implanted and the increasing age of the population. Data available to date show an increase in the incidence of total hip arthroplasty replacement in the Spanish population of from 20.2 to 21.1 per 100,000 inhabitants/year from 2001 to 2008, respectively.1 In this period there has also been an increase in the incidence of primary hip arthroplasty from 99 to 105 per 100,000 inhabitants/year.2 Due to this total hip replacement is now being used for an increasingly older age range, so that the corresponding patient profile has more comorbidities.2
The above-mentioned aspects of primary hip arthroplasty also apply to revision surgery, although they are even more marked. This procedure is now being used in an older population than is the case for primary surgery, with more comorbidities.1 This is combined with longer times of surgery, more bleeding and therefore greater risks than those arising in primary surgery.
Due to the many reasons that lead us to the need to reoperate an implanted hip prosthesis, our series aims to evaluate the incidence of each one of the causes for total hip replacement revision operations performed in our centre during a 5-year period.
Materials and methodsAll primary hip arthroplasty rescue surgeries from 1 January 2009 to 31 December 2013 were recorded retrospectively. Patient age and sex were recorded, together with the date of the primary hip replacement, the date of prosthesis replacement and the main cause of repeat surgery. Those re-operations performed before 5 years had passed after the first arthroplasty were classified as early revision surgery.
Exclusion criteria were: patients under the age of 18 years old, pregnant women, B2 periprosthetic fractures in which it was decided to use open reduction and internal fixing due to the poor general condition of the patient, revision arthroplasties of partial hip prostheses and rescue arthroplasty revision surgery.
Statistical analysisInitially a descriptive analysis was undertaken, in which qualitative variables were expressed as frequencies and percentages. Continuous variables were expressed as an average±standard deviation and the median (minimum–maximum). The Kolmogorov–Smirnov tests were used to detect the normality of the variables.
Parametric and non-parametric tests were used to determine the potential association between study variables (Chi-squared, Student's-t for independent samples and single factor Anova).
In all of the analyses differences when P<0.05 were considered to be statistically significant. The analyses were carried out using SPSS 15.0.
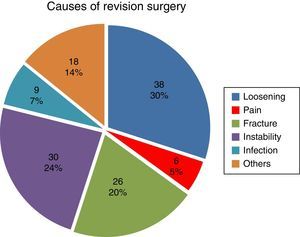
ResultsDuring the period from 1 January 2009 to 31 December 2013 a total of 127 hip rescue surgical operations were performed, corresponding to 127 patients. We classified the reasons for revision surgery as: instability, aseptic loosening, periprosthetic fracture, early or late infection, pain and others (including osteolysis without loosening, wear of the polyethylene and other less common reasons such as breakage of the ceramic head, early migration of the acetabulum, etc.).
The most frequent cause of revision was loosening, with 38 cases (29.9%), followed by instability with 30 cases (23.6%). Pain was the least frequent cause, with 6 cases (4.7%) (Fig. 1).
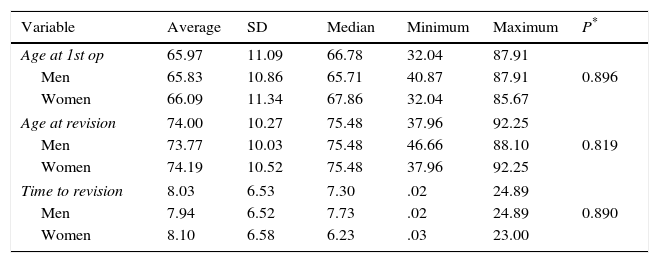
Regarding the sex of the patients, 71 (55.9%) were women, with an average age at the first surgical operation of 65.97 (±11.09) years old and an average age at revision surgery of 74.00 (±10.27) years old. There was no statistically significant difference between the average age of the men and women at the moment of the first operation (P=0.896), or at the time of revision surgery (P=0.819). Nor were any differences detected according to sex in terms of the time period before revision surgery took place (P=0.890) (Table 1).
Descriptive analysis according to sex of patient, age at each surgical operation and time to revision.
| Variable | Average | SD | Median | Minimum | Maximum | P* |
|---|---|---|---|---|---|---|
| Age at 1st op | 65.97 | 11.09 | 66.78 | 32.04 | 87.91 | 0.896 |
| Men | 65.83 | 10.86 | 65.71 | 40.87 | 87.91 | |
| Women | 66.09 | 11.34 | 67.86 | 32.04 | 85.67 | |
| Age at revision | 74.00 | 10.27 | 75.48 | 37.96 | 92.25 | 0.819 |
| Men | 73.77 | 10.03 | 75.48 | 46.66 | 88.10 | |
| Women | 74.19 | 10.52 | 75.48 | 37.96 | 92.25 | |
| Time to revision | 8.03 | 6.53 | 7.30 | .02 | 24.89 | 0.890 |
| Men | 7.94 | 6.52 | 7.73 | .02 | 24.89 | |
| Women | 8.10 | 6.58 | 6.23 | .03 | 23.00 | |
SD, standard deviation; Age at 1st op, age at first surgical operation.
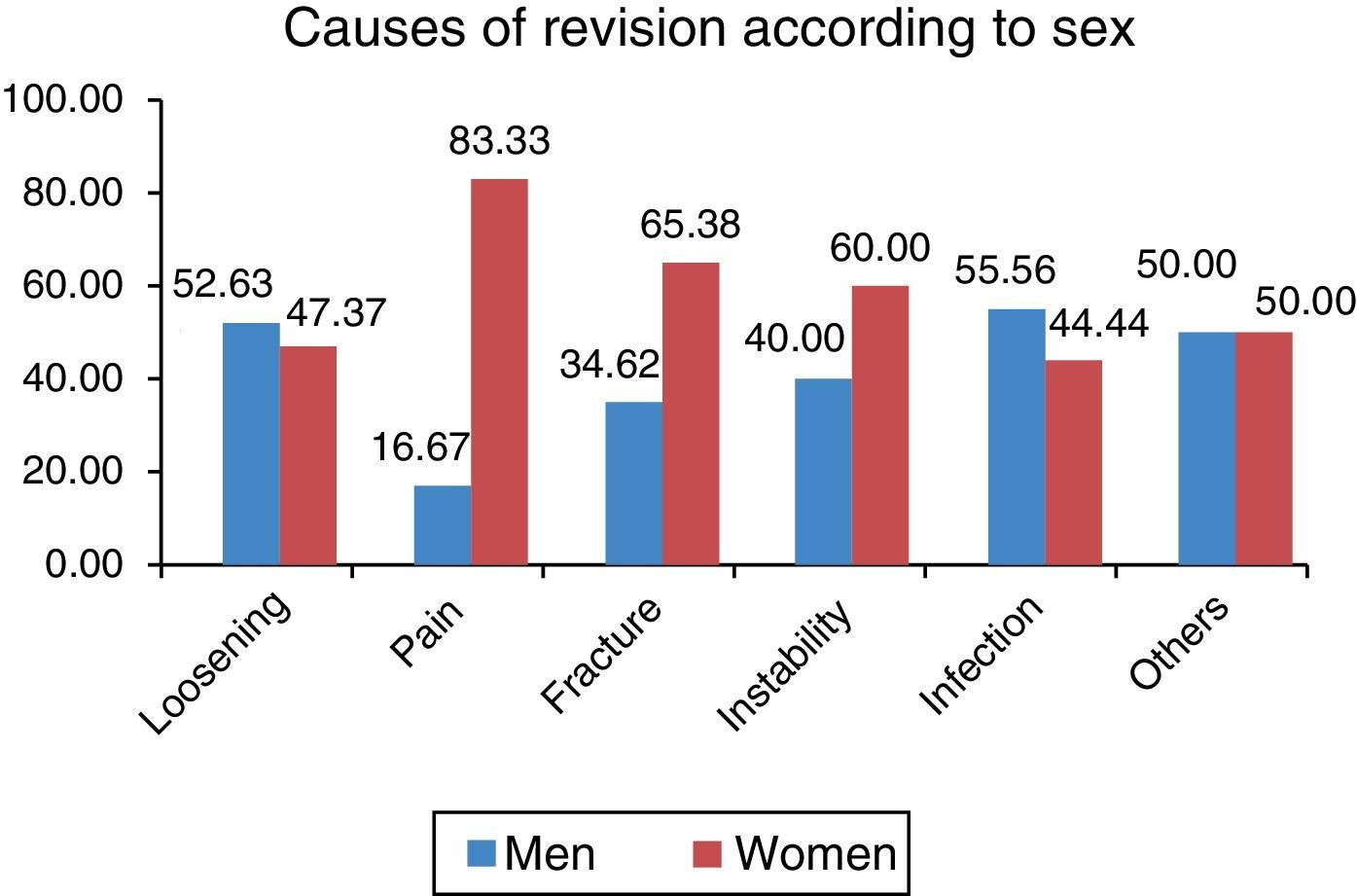
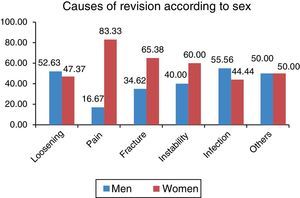
No statistically significant differences were found regarding the causes of the revision surgery according to sex (P=0.436), although a higher percentage of women were found to have been operated again due to pain, periprosthetic fracture and instability, while a higher percentage of men were operated again due to infection and loosening (Fig. 2).
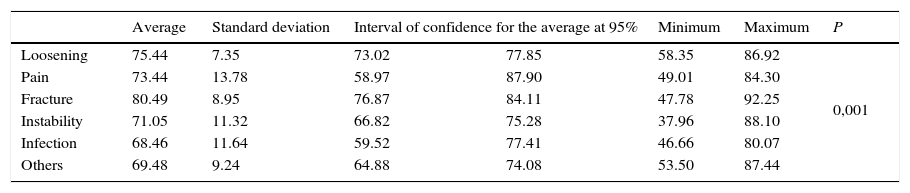
Regarding age at the moment of revision surgery, statistically significant differences were found in connection with the reason for this (P=0.001): patients who were operated again due to fracture were significantly older than those operated because of infection (P=0.024), instability (P=0.006) and due to other causes (P=0.004) (Table 2).
Descriptive analysis according to patient ages at the moment of revision surgery and cause.
| Average | Standard deviation | Interval of confidence for the average at 95% | Minimum | Maximum | P | ||
|---|---|---|---|---|---|---|---|
| Loosening | 75.44 | 7.35 | 73.02 | 77.85 | 58.35 | 86.92 | 0,001 |
| Pain | 73.44 | 13.78 | 58.97 | 87.90 | 49.01 | 84.30 | |
| Fracture | 80.49 | 8.95 | 76.87 | 84.11 | 47.78 | 92.25 | |
| Instability | 71.05 | 11.32 | 66.82 | 75.28 | 37.96 | 88.10 | |
| Infection | 68.46 | 11.64 | 59.52 | 77.41 | 46.66 | 80.07 | |
| Others | 69.48 | 9.24 | 64.88 | 74.08 | 53.50 | 87.44 | |
P: single factor Anova.
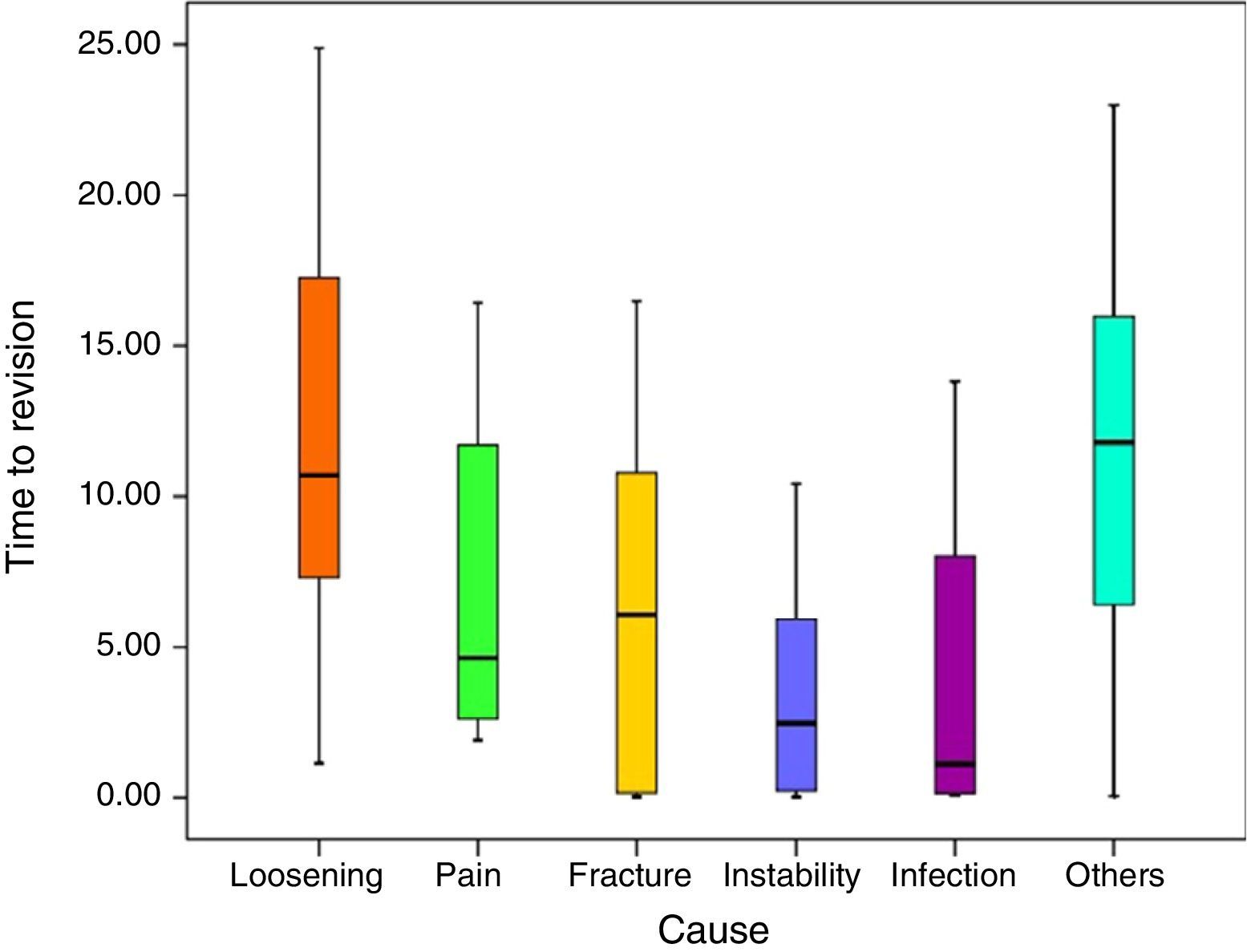
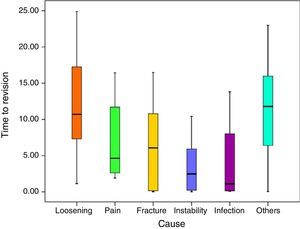
Statistically significant differences were also found in terms of the time that had passed before revision surgery according to the reasons for the same (P<0.001). Paired differences in connection with loosening were statistically significant (P<0.001), except for the comparison with other causes of the revision surgery (P=.999) and with pain (P=.541).
Of the 9 patients which required revision surgery due to infection, 4 (44.4%) of these cases arose during the first year after surgery, while 3 (33.3%) occurred more than 5 years after the primary surgery (Fig. 3).
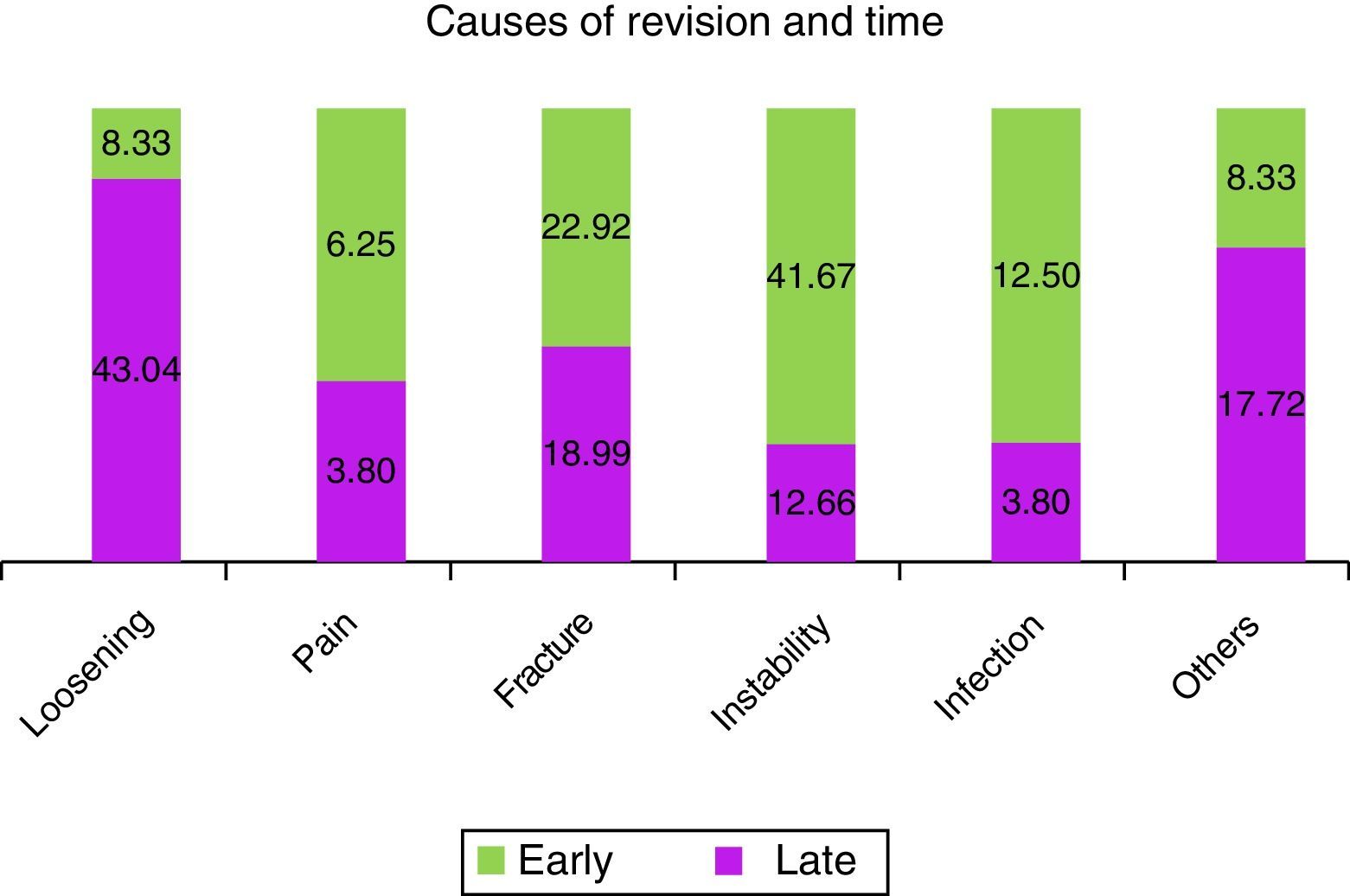
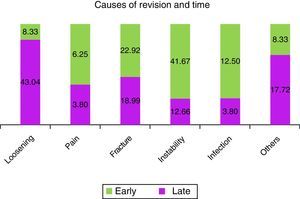
When the early rescue operations were studied statistically significant differences were found regarding age at primary surgery (P=0.001). Patients with late revision surgery were almost 7 years younger, with an average age of 63.40 (±9.88) years old, compared to early revision patients at an average age of 70.21 (±11.76) years old (Fig. 4). An association was also found between the cause of revision (P<0.001), as instability was associated (41.7%) with early revision, while loosening (43.0%) was associated with late revisions (Fig. 5).
DiscussionSeveral studies have shown a significant improvement in longevity as well as quality of life following total hip replacement surgery.3–6 Likewise, this has been shown to be a cost-effective procedure,3–6 with a duration of approximately 10 years in 92–94% of patients, according to the Scandinavian series.7
Several reasons for revision surgery of total hip replacement have been described in the literature. In our study we considered 5 main categories of reasons: instability, aseptic loosening, pain and a miscellaneous group of reasons which, due to the low number of patients in our sample, we have analysed together. These include osteolysis without loosening, isolated wear of the polyethylene, breakage of the ceramic components, breakage of the acetabulum, breakage of the rod and early migration of the acetabulum.
In our series we found that the most important reasons were loosening and instability. This is also the case in other similar studies, such as the American series published by Bozic et al.,8 which found an incidence of instability of 22.5% of cases, loosening in 19.7% and infection in 14.8%. Scandinavian series give similar results, in which rescue surgery took place due to instability in 33.5% of cases in Denmark, 23.4% in Sweden and 23.8% in Norway7 (24% in our series). On the other hand, we have observed an increase in the number of revision surgery operations from 2009 to 2013. This tendency had already been observed by Villanueva et al.1 from 2001 to 2008, using the national Spanish database of hospital discharges.
In our series we analysed the reasons for rescue surgery according to the length of time before it took place. Those operations which took place within 5 years of the primary surgery were classified as early revisions, while those which occurred after this period were classified as late revisions. The main reasons in the first group were instability and infection, while in the second group loosening and the miscellaneous group of other reasons were the main reasons. The study by Melvin et al.9 analysed the causes of failure in their series of primary hip replacement patients. Those patients operated less than 5 years after the primary surgery were termed early revisions by them, as was the case in our study. This revision found a total of 29% of revisions were due to aseptic loosening, 19.5% were due to infection and 19.1% to instability. In our series, 12.5% of early revisions were due to infection, a lower rate than the one cited by Melvin et al. (19.5%); nevertheless, the patients in our series had a statistically higher incidence of instability (41.67% as opposed to 19.1% in the American series).9
Instability following primary hip arthroplasty is still one of the most common complications, and it is therefore one of the main reasons for revision surgery. This causes major frustration for the surgeon, a clear increase in morbimortality and a loss of patient confidence.
A bibliographical revision by Fernández-Fairén et al.10 described in incidence of luxation in primary total hip replacement that varies from 0.5% to 9.2%. These figures are even higher for rescue arthroplasties, with an incidence of up to 28%.11,12 Some studies describe luxation as the most frequent complication in the first 90 days13 and the first cause of revision surgery of primary hip prosthesis.8 Our series confirms these results in the context of early rescue surgery.
The high incidence of instability may be due to certain technical aspects, such as the habitual use of the posterolateral route.14 This is usually used in our medical area, while in the majority of cases 28mm heads are used in this period. Additionally, no anatomical references are used when aligning the acetabulum at this time. Currently, the increase in the diameter of the prosthesis head and above all an improvement in the alignment of the acetabular implant (using anatomical references such as the crossed ligament or the sciatic notch)15 together with systematic reinsertion of the posterior capsule and the rotators have clearly reduced the incidence of instability. Likewise, the influence of factors intrinsic to the patients themselves has become clear, such as their feminine sex (as is the case in our study), age greater than 70 years old, previous fractures, a preoperative American Society of Anaesthesiologists score (ASA) of 3–4,16 inflammatory arthritis,17 a body mass index higher than 3018 and mental disorders.19
Regarding infection as the cause of rescue surgery, we had 9 cases during our five-year period. According to Tsukuyama's classification,20 in our series we found one case of positive intraoperative cultures, 4 cases of early postoperative infection, 2 of acute haematogenous infection and one chronic late infection. All of the cases with infection were treated using surgery and antibiotic therapy. Of the 9 cases diagnosed as infection, 6 were due to Staphylococcus aureus, of which 2 were methicillin resistant. In the other patients the main germ isolated was Staphylococcus epidermidis in 2 cases and Streptococcus faecalis in 1.
As was pointed out above, the American study by Bozic et al.8 described an incidence of 14.8% of infection as the reason for rescue surgery. On the other hand, the Scandinavian series7 offer figures of 15.8% (Denmark), 15.0% (Sweden) and 15.5% (Norway). The last annual report of the Australian Orthopaedic National Joint Replacement Registry (AONJRR) cites an incidence of 17.3%. These figures are moderately higher than that of our series, where infection is the reason for rescue surgery in 7% of all such operations (Fig. 1).
Our case of intraoperative cultures in patients due to supposed aseptic loosening confirms the fact described in previous studies that low degree infection may be a cause. In the study by different Danish centres published by Moojen et al.,21 it was found that 4–13% of the patients with a preoperative diagnosis of aseptic loosening presented positive intraoperative cultures. In our series this percentage only amounted to 2.56%, which leads us to suspect that we have under-diagnosed cases that went on to develop a postoperative infection considered to be post-surgical, or that they failed at an early stage due to loosening. This fact has led us to change our behaviour: we now systematically take more than 3 samples in all rescue implants.
Aseptic loosening of total hip replacement is the first cause of late rescue surgery in our series. We included the group of osteolysis without loosening in the group of “others” due to its small sample, even though biologically it is the commencement of the loosening process. Its incidence is increasing in the population with a primary prosthesis implanted at a younger age, as is shown by our results. Münguer et al.22 analysed a registry of patients with aseptic loosening and found an incidence that decreased by 1.8% for each additional year of age at the moment of prosthesis implantation. This is due to a reduced functional demand. Regarding other variables such as sex, males are found to be at greater risk in this study, while weight and height had no influence,22 as was confirmed in our series, although this was not statistically significant. The average duration of the implant in the cases of aseptic loosening was found to be 12.12 years (Fig. 3) in our study: there were a total of 21 revision operations due to the acetabulum (55.26%), 8 operations due to the stem (21.5%) and 9 operations due to both (femoral and acetabular) components (23.68%).
We know that the incidence of periprosthetic fractures is rising continuously. This is directly proportional to the increase in primary hip replacements and the ageing of the population. In our series it is the third cause of rescue surgery. A tendency has been observed for these fractures to occur in increasingly elderly patients (Fig. 3), with uncemented fixing,23–25 wedge-shaped stems26 and with an associated underlying disease.
Periprosthetic fractures may occur during the operation, when they usually go unnoticed, or over the long term due to a traumatic event, usually a low energy one, in elderly patients. Other factors may also influence them, such as previous osteolysis or stress forces on a previous failed prosthesis.27
In our series we recorded the periprosthetic fractures that required a change of components. They were generally of the B2 and B3 types according to the Vancouver classification,28 excluding those that were stabilised by a plate. Osteosynthesis surgery was performed in some cases of B2 or B3 fracture due to associated patient comorbidities. These would have made the replacement surgery indicated for fractures of this type impossible.
The figures given by the Scandinavian series,7 5.1% (Denmark), 6.7% (Sweden) and 3.5% (Norway) are significantly lower than the one corresponding to our series (20%) (Fig. 1). Nevertheless, the 18.2% of periprosthetic fractures cited in the latest Australian registry (AOANJRR) is closer to that of this study. This datum may be due to the age of our population, as 28.58% are older than 65 years old according to the latest data of the IGE (Galician Statistical Institute).
Although our study followed strict inclusion and exclusion criteria, it has certain limitations due to its retrospective nature. It also lacks the total number of initial primary hip replacements, and the patients had been operated in other centres as well as ours. Patients may also have been lost if, having been operated on first in our hospital, they were operated in other centres for revision surgery.
To conclude, failure of total hip replacements is an increasingly habitual reason for consultation and repeat operation. The most frequent causes of this are instability, aseptic loosening and periprosthetic fractures. Analysis of our series gives similar results to those of previous studies, except for the high rate of instability during the first year. This study has enabled us to change what we do in primary as well as revision surgery, with the aim of continuing to improve our results.
On the other hand, we found that patient age strongly influences the duration of the primary replacement. The results of records show that the failure rate due to aseptic loosening is higher in the younger population (AOANJRR) because of increased physical activity and the existence of previous structural or morphological alterations (dysplasia, the sequelae of trauma, etc.). On the other hand, our study shows a marked tendency for early failure in patients who received their first replacement at an older age. This is due to the higher risk of instability, infection and periprosthetic fractures, above all.
Levels of evidenceLevel III.
Conflict of interestThe authors have no conflict of interest to declare.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Please cite this article as: Capón-García D, López-Pardo A, Alves-Pérez MT. Causas de cirugía de revisión en artroplastia total de cadera. Análisis epidemiológico retrospectivo. Rev Esp Cir Ortop Traumatol. 2016;60:160–166.