To evaluate the outcomes of cementless total hip replacement after acute femoral neck fracture in active patients.
Material and methodsA prospective matched study was conducted to compare the results of 76 patients with fractures and 76 patients with osteoarthritis. The Harris score, short-WOMAC and SF-12 were used for the clinical assessment. The mean follow-up was 7.3 years (range 5–11).
ResultsThere were no significant differences in medical or surgical complications between the 2 groups. Functional outcomes were similar, but more walking aids were used in the fracture group. There were 6 revisions among the fracture group (one dislocation, 2 deep infections, 3 aseptic loosening), and 2 aseptic loosening among controls. There was no significant difference in arthroplasty survival at 10 years (88.7 vs. 96.1%, P=.15). The mortality rates at 2 and 10 years were similar.
ConclusionCementless total hip replacement for treatment of acute femoral neck fracture showed results similar to those of elective surgery for osteoarthritis in these selected patients.
Evaluar los resultados de la artroplastia total de cadera no cementada tras fractura cervical femoral aguda, en pacientes previamente activos.
Material y métodosEstudio prospectivo emparejado de 76 pacientes con fractura y 76 con coxartrosis. Para la valoración clínica se utilizó la escala de Harris, el WOMAC reducido y el SF-12. Seguimiento medio de 7,3 años (rango 5–11).
ResultadosNo había diferencias significativas en las tasas de complicaciones médicas o quirúrgicas. Los resultados funcionales fueron similares, pero con mayor utilización de ayudas para caminar en los pacientes con fractura. Entre estos hubo 3 luxaciones, y ninguna en los controles. Entre los pacientes fracturados hubo 6 revisiones (una luxación, 2 infecciones profundas y 3 aflojamientos asépticos), mientras en el grupo de coxartrosis hubo 2 aflojamientos asépticos. No había diferencia significativa en la supervivencia de la prótesis a 10 años (88,7 vs. 96,1%, p=0,15). Las tasas de mortalidad a 2 y 10 años fueron similares.
ConclusiónLa artroplastia total de cadera no cementada para tratamiento de fractura cervical femoral aguda se mostró similar a la cirugía electiva por artrosis en estos pacientes seleccionados.
Hemiarthroplasty has proven to be a suitable treatment for the majority of displaced femoral neck fractures.1 In general, total hip arthroplasty (THA) is not recommended for elderly patients with this fracture due to the poor postoperative functional expectations, increased risk of dislocation and greater cost.2 However, the increase in life expectancy and improved physical condition of elderly patients in developed countries have led to an increase of the drawbacks of hemiarthroplasty, primarily those derived from erosion of the acetabulum in active elderly patients.3,4 Systematic reviews, such as that conducted by Cochrane,5 have shown that the use of THA in displaced femoral neck fractures is more effective than hemiarthroplasty, as it provides better function, less pain and a lower revision rate without increasing medical complications. Conversely, the downside is a higher dislocation rate. Nevertheless, there is no consensus regarding its use in these fractures, as shown by a study of national arthroplasty records,6 in which THA in femoral neck fractures was used 6 times more frequently in Sweden than in England, 4 times more than in Australia and twice more than in Canada.
The effectiveness of elective THA has been extensively studied, including the use of uncemented THA in elderly patients.7 This experience has been extrapolated to the treatment of hip fractures; however, these fractures entail certain characteristics inherent to the lesion itself and to patients suffering pathologies other than coxarthrosis (or hip osteoarthritis). Although numerous studies have compared THA and hemiarthroplasty in elderly patients with hip fractures,8 very few studies have compared the use of THA in the treatment of these fractures and elective surgery.9–12
Our working hypothesis was that the initial diagnosis of femoral neck fracture did not influence the outcome of THA in previously active patients. Thus, our main objective was to evaluate the results of primary cementless THA as an initial treatment for acute femoral neck fractures in active patients with appropriate expectations regarding postoperative functional demand, compared with that of primary THA for coxarthrosis. The secondary objective was to assess the medical complications and mortality of hip fractures following primary THA.
Materials and methodsIn January 2001 we initiated a prospective comparative study of the treatment of femoral neck fractures using uncemented THA. The study was approved by the Clinical Research Ethics Committee of our institution. The criteria for inclusion in the study group were acute displaced fracture, age 60 years or above, patients with independence for activities of daily living, unlimited walking radius, walking without aids and no cognitive impairment, as described in the section on assessment. Inclusion in the study was independent of radiographic bone quality. Patients with pathological fractures caused by neoplasms, rheumatoid arthritis and other inflammatory or metabolic arthropathies were excluded from the study. In order to evaluate the results of the THA, the study required a minimum postoperative follow-up period of 5 years. As control group we selected a cohort of consecutive patients undergoing uncemented THA due to primary coxarthrosis, with a 1:1 ratio according to the following variables: age (±3 years), gender, body mass index, date of surgery, prosthesis model and surgeon. We did not match the baseline condition of the hip, as the coxarthrosis group could present greater deterioration. Except for the primary diagnosis, the inclusion and exclusion criteria were similar to those of the study group.
Surgical ProtocolAll interventions were performed by 2 specialists in hip surgery (ALU and JSR) in a laminar flow room with spinal anesthesia. The Hardinge lateral pathway13 was used in all cases. We implanted 2 types of uncemented THA systems; one was the Meridian stem system with Trident® acetabular cup (Stryker, Mahwah, NJ, USA) used in 82 hips (41 following fracture and 41 following coxarthrosis) during the period 2001–2004 and the other was the stem system with Duofit® cup (Samo, Bologna, Italy) used on 70 hips (35 following fracture and 35 following coxarthrosis) during the period 2005–2007. In both systems, the stems were straight and collarless, made of titanium alloy with proximal porous coating of plasma spray and metaphyseal pressure fitting, with similar geometry. All acetabula were hemispherical, made of titanium alloy with a porous plasma-spray coating and pressure fitting after milling. They were secured with 2 divergent screws in all cases, regardless of bone quality. We also used high molecular weight polyethylene inserts in all hips. These inserts were sterilized with gamma radiation in air, and had an elevation of 12° and a metal head of 28mm. All patients followed a standard postoperative protocol. We applied antibiotic prophylaxis for 24h with first-generation cephalosporin, and thromboprophylaxis with low molecular weight heparin for 1 month. The patients received postoperative blood transfusions whenever hemoglobin levels fell below 8g/dL. We did not use prophylaxis against heterotopic ossification. Load using a walking frame or crutches was authorized on the day after surgery if the pain allowed it.
AssessmentsAll patients with hip fractures were assessed by an internist and an anesthesiologist upon admission. Preoperatively, both the group of patients suffering fractures and those with coxarthrosis were assessed using the scale of activities of daily living by Katz et al.14 and the Mini-Mental test.15 According to the scale by Katz et al., all patients in both groups presented an A level of independence, as they did not require assistance for personal hygiene, dressing, sitting and rising from a chair or bed; and they had sphincter continence and were self-sufficient to feed. Cognitive function using the Mini-Mental test provided a score of 10 in all patients. The initial general health condition was assessed according to the number of comorbidities, taking into account that those which most affected the prognosis in hip fractures16 were arterial hypertension, heart disease, lung disease, kidney disease, stroke, diabetes, rheumatism and Parkinson's disease. The pre-anesthetic risk was assessed according to the scale of the American Society of Anesthesiologists.17 We did not consider carrying out a clinical or preoperative functional assessment of the hip, as it was not possible to carry it out successfully in the group of patients suffering from fractures.
All patients in both the groups were assessed clinically and radiographically after surgery: at 6 weeks, 3 and 6 months, 1 year and then annually for at least 5 years. We used the Harris18 hip scale for clinical assessment. Anterior thigh pain was scored as absent, mild, moderate or severe, using the same criteria as in the pain subcategory of the Harris scale. Quality of life was also assessed, using the SF-12 questionnaire validated for Spanish19 for overall quality (physical and mental dimensions) and the reduced version WOMAC20 for the lower limbs (pain and function dimensions), both adjusted to a 0–100 scale (worst to best outcome).
We obtained standard, anteroposterior and lateral radiographs preoperatively and on each postoperative visit. The stability of the components was determined by comparing the radiographs at 6 weeks postoperatively with the last assessment conducted. For the acetabulum we applied the criteria of Gonzalez della Valle et al.21 for uncemented components, considering unstable those which presented continuous radiolucencies of 1mm or more, incomplete for at least 2mm or migration of more than 2mm or rotation greater than 2°. For the femoral component we applied the criteria of Engh et al.22 for uncemented stems, considering unstable those which presented continuous radiolucency of at least 2mm, progressive sinking greater than 5mm or a change in position of at least 3°. We used the areas of Gruen et al.23 to locate radiolucent areas, and heterotopic ossification was graded according to Brooker et al.24
Statistical analysisThe statistical analysis was performed using the software package SPSS® (SPSS Inc., Chicago, IL, USA), version 15.0. Values of P≤.05 were considered significant. We used the Kolmogorov–Smirnov test to determine normal distribution. For comparisons between cohorts we conducted univariate analysis for categorical variables using the chi-square tests in variables with normal distribution, or the Mantel–Haenszel test for nonparametric data. For continuous variables we used the Student's t test or the Mann–Whitney test. Relative risks (RR) were estimated with 95% confidence intervals (CI). We used logistic regression analysis to identify independent predictors of risk, calculating the hazard ratio with 95% CI. Kaplan–Meier analysis was used to calculate the cumulative survival and the log-rank test to compare survival curves.
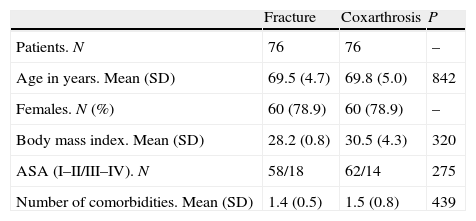
ResultsBetween January 2001 and December 2007 we treated 455 patients suffering from acute displaced femoral neck fracture at our center, of which 90 met the inclusion criteria, of which we excluded 14 who were under the age of 60 years. Thus, the study group consisted of 76 patients treated with cementless THA. The group included 60 females and 16 males, with a mean age of 69.5 years (range: 62–86 years). The control group consisted of another 76 patients. The preoperative characteristics of both groups are shown in Table 1, with no significant differences between them. Moreover, considering the prosthesis model used, there were no significant differences regarding age (P=.53), gender (P=.61) and BMI (P=.37).
Preoperative data.
| Fracture | Coxarthrosis | P | |
| Patients. N | 76 | 76 | – |
| Age in years. Mean (SD) | 69.5 (4.7) | 69.8 (5.0) | 842 |
| Females. N (%) | 60 (78.9) | 60 (78.9) | – |
| Body mass index. Mean (SD) | 28.2 (0.8) | 30.5 (4.3) | 320 |
| ASA (I–II/III–IV). N | 58/18 | 62/14 | 275 |
| Number of comorbidities. Mean (SD) | 1.4 (0.5) | 1.5 (0.8) | 439 |
ASA, American Society of Anesthesiologists; SD, standard deviation.
The mean postoperative follow-up period was 7.3 years (range: 5–11 years) in the fracture group and 7.1 years (range: 5–11 years) in the coxarthrosis group (P=.62). The mean delay of surgery in the fracture group was 3.2 days (range: 1–9 days). The mean hospital stay was 10.9 days (range: 5–12 days) in the fracture group and 7.2 days (range: 5–12 days) in the coxarthrosis group (P=.001). In both groups, all patients came from their homes and returned to them. The risk of perioperative blood transfusion was similar in both groups (RR 1.6; 95% CI 1.2–3.4; P=.18) in the fracture group (14 patients, 18.4%) and in the coxarthrosis group (9 patients, 11.8%).
Functional resultsIn the analysis of functional and radiographic results of THA, we excluded deaths of patients who had not undergone the minimum postoperative follow-up period of 5 years (6 fracture patients and 2 coxarthrosis patients). These cases did not include any THA complications in the last assessment conducted. Thus, the analysis of results included 70 patients with fractures and 74 with coxarthrosis.
There were no significant differences between groups regarding postoperative Harris score (Table 2) in the last follow-up, and in the case of surgical revisions and in the subsequent result. In the fracture group, 67 patients (95.7%) reported absent or mild pain in the hip and in 3 cases (4.3%) it was moderate or severe, whilst in the coxarthrosis group this was reported in 72 (97.3%) and 2 (2.7%) cases, respectively (P=.47). In the fracture group, thigh pain was not reported or was discontinuous in 69 patients (98.6%), and continuous or severe in 1 case (1.4%), whilst in the coxarthrosis group this was reported in 71 (96.0%) and 3 (4.0%) cases, respectively (P=.62). Regarding walking aids, in the fracture group there were 58 patients (82.8%) who did not use them or used a cane occasionally, 8 (11.4%) who used a cane permanently and 4 (5.8%) with 2 canes or a walking frame, whilst in the coxarthrosis group there were 71 patients (95.9%) who did not use a cane or did so occasionally and 3 (4.1%) who required a cane permanently. This difference regarding walking aids was significant (P=.009). The model of prosthesis employed did not influence the functional score, pain in the hip or thigh, or use of walking aids (P>.31). Subjective assessments, both regarding hip function with the WOMAC questionnaire and perceived quality of life with the SF-12 questionnaire, showed no significant differences between the groups (Table 2).
Postoperative functional results.
| Fracture | Coxarthrosis | P | |
| Patients. N | 70 | 74 | – |
| Follow-up in years. Mean (SD) | 7.3 (2.4) | 7.1 (2.3) | 62 |
| Harris scale. Mean (SD) | 87.8 (13.7) | 90.4 (7.7) | 18 |
| Hip pain. N (%) | 3 (4.3) | 2 (2.7) | 47 |
| Thigh pain. N (%) | 1 (1.4) | 3 (4.0) | 62 |
| Walking aid. N (%) | 12 (17.1) | 3 (4.0) | .009 |
| WOMAC pain. Mean (SD) | 91.5 (12.9) | 89.0 (13.9) | 31 |
| WOMAC function. Mean (SD) | 83.8 (16.4) | 87.1 (11.9) | 22 |
| SF-12 physical. Mean (SD) | 79.7 (17.6) | 84.2 (15.4) | 10 |
| SF-12 mental. Mean (SD) | 82.4 (17.2) | 87.6 (18.3) | 08 |
SD, standard deviation; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
The last evaluation did not include any significant differences between groups regarding the mean acetabular inclination angle (P=.43), which in the fracture group was 43.4° (range: 31–55°) and in the coxarthrosis group was 44.7° (range: 28–54°), or regarding the rate of varus femoral components (P=.32), which in the fracture group was 5 (7.1%) and in the coxarthrosis group was 3 (4.0%). There were no significant differences regarding the prosthetic model used (P>.51).
Regarding the condition of components, and in cases with revision, prior thereto, in the fracture group there were 66 acetabula (94.2%) with bone fixation and without radiolucency or osteolysis, another 2 with non-progressive radiolucency under 2mm in areas 2 and 3 with stable fibrous fixation and without clinical significance, and another 2 with full radiolucency, which required revisions. At the femoral level, in the fracture group there were 66 stems (94.2%) with bone anchorage, 3 with non-progressive radiolucencies under 2mm in zones 1 and 7 and without clinical significance, and 1 with progressive collapse, which required revision. In the coxarthrosis group, 71 acetabula (95.9%) had bone fixation with no radiolucency or osteolysis, 3 had non-progressive radiolucencies under 2mm in zone 2, all without clinical significance and bone fixation, and 1 acetabulum had complete radiolucency which required revision. At the femoral level, there were 73 stems (98.6%) with bone fixation and 1 with progressive collapse, which required revision. In both the groups, the stem or acetabulum model employed did not influence the condition of the fixation of components (P>.57). There were 5 heterotopic ossifications in the fracture group and 4 in the coxarthrosis group, all of them grade 1 and without clinical significance.
Surgical revisions and complicationsIn the evaluation of results we considered valid those cases with a minimum follow-up of 5 years. Postoperative complications are shown in Table 3. There were intraoperative fractures without displacement at the level of the calcar femorale in 2 hips (2.8%) in the fracture group, and in 1 hip (1.3%) in the coxarthrosis group (P=.47). All were treated by wired cerclage, without subsequent collapse of the stem and satisfactory functional outcomes. There were 4 infections (5.7%) in the fracture group. Of these, 2 were superficial and healed conservatively with satisfactory results, whilst the other 2 required surgical revision with replacement in 2 stages, with unsatisfactory results. In the coxarthrosis group, there were 2 superficial infections (2.6%), which healed conservatively with satisfactory results, with no cases of deep infection. The RR of infection did not differ between the groups (RR 2.1; 95%CI 0.3–12.3; P=.31). There were 3 dislocations (4.2%) in the fracture group, 2 of which appeared early and were resolved conservatively, whilst the other occurred at 2 months postoperatively and required replacement of the stem due to recurrence, all with satisfactory functional results. In the coxarthrosis group there were no dislocations.
Complications in total hip arthroplasty.
| Fracture | Coxarthrosis | RR | 95% CI | P | |
| Intraoperative fracture | 2 (2.8) | 1 (1.3) | 2.1 | 0.1–24.2 | .47 |
| Superficial infection | 2 (2.8) | 2 (2.7) | 1.0 | 0.1–7.7 | .66 |
| Deep infection | 2 (2.8) | 0 | – | – | .23 |
| Dislocation | 3 (4.2) | 0 | – | – | .11 |
| Unstable acetabulum | 2 (2.8) | 1 (1.3) | 2.1 | 0.1–24.2 | .47 |
| Unstable stem | 1 (1.4) | 1 (1.3) | 1.0 | 0.1–17.2 | .73 |
| Total septic revisions | 2 (2.8) | 0 | – | – | .23 |
| Total aseptic revisions | 4 (5.6) | 2 (2.7) | 2.1 | 0.3–12.3 | .31 |
CI, confidence interval; RR, relative risk.
Data expressed in n (%).
As belated mechanical complications, 3 patients in the fracture group, mentioned previously in the radiographic assessment, required aseptic revision. Two were due to loosening of the acetabulum, with revision at 65 and 80 months postoperatively, and the other due to progressive collapse of the stem, without prior intraoperative fracture at 73 months postoperatively. In the coxarthrosis group there were 2 cases, mentioned previously in the radiographic assessment, of revision due to aseptic loosening, 1 of the acetabulum at 27 months postoperatively and another of the stem at 15 months postoperatively. The risk of aseptic loosening did not differ between the groups (RR 1.6; 95%CI 0.2–9.9; P=.47), and there were no significant differences between the 2 models of prosthesis employed (P=.86).
In summary, 6 hips (8.4%) required revision in the fracture group, of which 2 (2.8%) affected both components due to septic causes and 4 (5.7%) due to an aseptic component (2 acetabula, 1 stem loosening and 1 stem by dislocation). In the coxarthrosis group, 2 (2.7%) cases required revision due to aseptic loosening (1 acetabulum and 1 stem). Considering all causes of revision, there were no significant differences in risk between both the groups (RR 3.5; 95%CI 0.6–17.3; P=.12). According to the Kaplan–Meier method, survival at 10 years of the implant, considering revisions for any cause, was 88.7% (95% CI 80.9–98.3) in the fracture group and 96.1% (95%CI 90.7–100) in the coxarthrosis group, with this difference not being significant (P=.15). Excluding the cases of infection, survival of the acetabula for aseptic causes (Fig. 1) was 92.5% (95%CI 85.2–99.8) and 97.1% (95%CI 93.1–100), respectively (P=.18), whilst that of the stems (Fig. 2), was 93.3% (95%CI 86.6–100) and 95.7% (95%CI 91.1–100), respectively (P=.17).
Morbidity and mortalityOut of all the patients included in the study, 6 of them (7.8%) in the fracture group presented perioperative medical complications (2 hematemesis, 1 diabetic decompensation, 2 renal failures, and 1 pulmonary decompensation), compared to 2 patients (2.6%) in the coxarthrosis group (urinary tract infections). In both groups there were no cases of deep vein thrombosis. The risk of medical complications was not significantly different (RR 3.1; 95%CI 0.6–16.1; P=.137). The presence of these complications did not affect the final functional result, which was satisfactory in all cases.
There were no hospital deaths in either group. In the fracture group, 2 patients died in the first postoperative year (2 heart diseases), 2 in the second year (heart disease and tumor), 2 in the third year (stroke and tumor), and 2 in the period between 5 and 10 postoperative years (heart disease and respiratory failure). In the coxarthrosis group, 1 patient died in the first year (stroke), another in the second year (stroke) and another 3 died in the period between 5 and 10 postoperative years (stroke, heart disease and tumor). There was no significant difference in the cumulative risk of death in any of the annual periods until 5 postoperative years (P>.10), or between 5 and 10 postoperative years (P=.32). The logistic regression analysis identified as a risk factor for death the number of comorbidities (hazard ratio 2.7; 95%CI 1.0–7.4; P=.045), but not age, gender or the score on the American Society of Anesthesiologists scale (P>.242).
DiscussionThe effectiveness of THA in degenerative hip disease has been clearly proven, as has the use of uncemented THA in elderly patients suffering osteoporosis.8 Likewise, THA has also shown its effectiveness in femoral neck fractures,6 although few studies have used uncemented THA in these fractures.9,10,25 Although hip fractures and coxarthrosis are different conditions, there are very few studies comparing the use of THA in these 2 scenarios. We have only found 4 such studies, 2 of them based on national arthroplasty registers11,12 and the other 2 comparing small samples with short follow-up periods.9,10 To the best of our knowledge, the present study is the largest prospective study and with the longest follow-up to date, although our series was composed of selected patients.
The main objective was to assess the results of THA after acute femoral neck fracture in active patients without dependencies, compared with those undergoing elective surgery for coxarthrosis. Our study found a satisfactory outcome in these selected patients. Functional outcomes were similar between the 2 groups, except for a greater use of walking aids in the group of patients with fractures. This was consistent with previous studies which provided function and quality of life assessments26,27 or compared clinical outcomes using the Harris pain scale.9,10
Dislocation was cited as a major complication following THA for femoral neck fracture.8 In addition to risk factors common to all THAs, such as the approach route and femoral head size,28 the higher propensity for dislocation among fracture patients has been attributed29 to a relatively greater laxity of the periarticular tissues, a greater range of preoperative mobility and an increased risk of falling. A recent metaanalysis4 showed dislocation rates between 0% and 20% among fracture patients; double that among the elective surgery group,11 although the work was based on studies with different approaches, prosthesis models and surgeons. In our study there were 3 dislocations (4.2%) among patients with fractures and none in the coxarthrosis group, which we considered clinically relevant, since the lack of statistical significance observed could be due to the size of the groups studied. Other studies did not find differences9 in the rates of dislocation among patients with fractures3,25 from 3.5% to 7.5%, using the same approach as in our study and similar prostheses. Nevertheless, most of these dislocations did not require revision of components.9,10,25
In our study, although there was a higher rate of revisions in the fracture group (8.5%) than in the coxarthrosis group (2.7%), the difference was not significant. However, this could be due to the sample size. The survival of the prostheses at 10 years, including septic and aseptic causes, was lower among fracture patients (88.7%) than among coxarthrosis patients (96.1%), but the difference was not significant, as also reported by other comparative studies.9,11,12 The use of cemented prostheses among fracture patients25,28 has also been associated with low revision rates of the components. By contrast, comparative studies11 based on arthroplasty registers reported a risk of revision among fracture patients which was 1.6 times higher than that among coxarthrosis patients, although this could be due to the high variability in the samples studied.
In our study, fracture patients had significantly longer hospital stays, possibly due to the preoperative time required for patient preparation and the greater number of perioperative complications. Although the 2 groups were similar regarding their scores on the American Society of Anesthesiologists scale and comorbidities, fracture patients presented a higher rate of medical complications. Nevertheless, these had no effect on mortality, perhaps due to the selection of our patients. The only risk factor for long-term mortality was the number of comorbidities. Another study30 noted that in addition to comorbidities, age was a risk factor for mortality following THA in fracture patients, although this series included non-selected patients with a greater mean age. Although mortality attributable to the fracture in the first 2 and 10 postoperative years was higher in the fracture group, it was not significantly different between both the groups (5.2% vs. 2.6% at 2 years and 10.5 vs. 6.5% at 10 years), and the causes of death were not related to the prosthesis. Other studies did not find a difference in mortality between fracture patients and elective surgery patients either.9,25 Some reported a lower mortality26 among previously healthy fracture patients than our study, of 6% at 6 years.
The present study has the strength of its prospective design, but also significant weaknesses. One is the use of 2 prosthesis models, despite the fact that they were very similar in design, and no significant differences in the results were found. The other is the sizes of the groups studied, which, although greater than those published previously, means that the results should be interpreted with caution in relation to the significance observed or lack thereof.
Based on the available data, in our study the diagnosis of femoral neck fracture in previously active patients did not seem to influence the outcome of the THA procedure. We believe that uncemented THA is a satisfactory treatment for these selected patients, comparable to its use in elective surgery for primary osteoarthritis in terms of complications, revisions and survival of patients and prostheses. Further, well-designed and long-term studies would be required to contrast these results.
Level of evidenceLevel of evidence ii.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace in the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Lizaur-Utrilla A, Sanz-Reig J, Miralles-Muñoz F. Artroplastia total de cadera no cementada tras fractura cervical femoral aguda en pacientes activos. Estudio prospectivo emparejado con seguimiento mínimo de 5 años. Rev Esp Cir Ortop Traumatol. 2014;58:152–159.